J Korean Soc Radiol.
2014 Nov;71(5):239-248. 10.3348/jksr.2014.71.5.239.
Correlation between Computed Tomography and Pathological Findings of Gastrointestinal Stromal Tumors Treated with Imatinib Mesylate
- Affiliations
-
- 1Department of Radiology, Anam Hospital, College of Medicine, Korea University, Seoul, Korea. radiolbj226@gmail.com
- 2Department of Radiology, Asan Medical Center, College of Medicine, University of Ulsan, Seoul, Korea.
- 3Department of Imaging Medicine, College of Medicine, Kangwon National University, Chuncheon, Korea.
- KMID: 2208793
- DOI: http://doi.org/10.3348/jksr.2014.71.5.239
Abstract
- PURPOSE
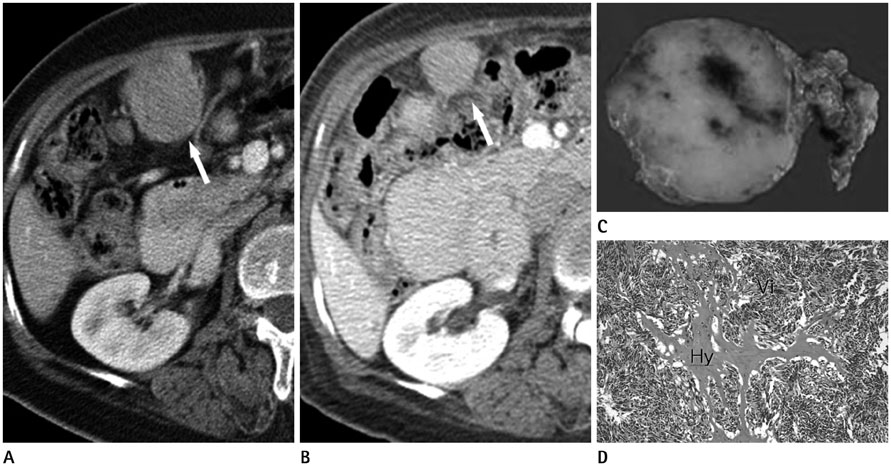
To evaluate the correlation between pathological and computed tomography (CT) findings of gastrointestinal stromal tumors (GISTs) after imatinib mesylate (imatinib) treatment.
MATERIALS AND METHODS
Twenty-six patients with GIST (17 men, 9 women; mean age, 56 years) who underwent treatment with imatinib and who were registered at our institution were included. Eight patients had primary and 18 had metastatic tumors. The correlation between CT and pathological findings was evaluated for all 26 tumors, which were resected after imatinib treatment.
RESULTS
The mean size change in the tumors after imatinib treatment was -1.4 cm (range, -7.8-2.5 cm). A reduction in tumor CT attenuation value was observed after imatinib treatment (mean, 29.1 Hounsfield units) in 20 of 26 tumors. Reduced attenuation was associated with non-tumorous pathological findings, including cystic degeneration (6/20), hemorrhagic necrosis (6/20), hyaline degeneration (6/20), and combined pathology without a viable portion (2/20). Of six tumors showing increased attenuation values after treatment, four (66.7%) showed an abundant viable portion. The increase in tumor size was not associated with the presence of a viable portion in any tumor.
CONCLUSION
CT attenuation changes in GISTs may adequately reflect the pathological findings in GISTs after imatinib treatment.
MeSH Terms
Figure
Reference
-
1. George S, Desai J. Management of gastrointestinal stromal tumors in the era of tyrosine kinase inhibitors. Curr Treat Options Oncol. 2002; 3:489–496.2. DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000; 231:51–58.3. Roberts PJ, Eisenberg B. Clinical presentation of gastrointestinal stromal tumors and treatment of operable disease. Eur J Cancer. 2002; 38:Suppl 5. S37–S38.4. Lehnert T. Gastrointestinal sarcoma (GIST)--a review of surgical management. Ann Chir Gynaecol. 1998; 87:297–305.5. Judson I. Gastrointestinal stromal tumours (GIST): biology and treatment. Ann Oncol. 2002; 13:Suppl 4. 287–289.6. Pidhorecky I, Cheney RT, Kraybill WG, Gibbs JF. Gastrointestinal stromal tumors: current diagnosis, biologic behavior, and management. Ann Surg Oncol. 2000; 7:705–712.7. Dennis KL, Damjanov I. Evaluating and reporting gastrointestinal stromal tumors after imatinib mesylate treatment. Open Pathol J. 2009; 3:53–57.8. Sarlomo-Rikala M, Kovatich AJ, Barusevicius A, Miettinen M. CD117: a sensitive marker for gastrointestinal stromal tumors that is more specific than CD34. Mod Pathol. 1998; 11:728–734.9. Eisenberg BL, Judson I. Surgery and imatinib in the management of GIST: emerging approaches to adjuvant and neoadjuvant therapy. Ann Surg Oncol. 2004; 11:465–475.10. Dematteo RP, Ballman KV, Antonescu CR, Maki RG, Pisters PW, Demetri GD, et al. Adjuvant imatinib mesylate after resection of localised, primary gastrointestinal stromal tumour: a randomised, double-blind, placebo-controlled trial. Lancet. 2009; 373:1097–1104.11. Choi H. Critical issues in response evaluation on computed tomography: lessons from the gastrointestinal stromal tumor model. Curr Oncol Rep. 2005; 7:307–311.12. Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. European Organization for Research and Treatment of Cancer. National Cancer Institute of the United States. National Cancer Institute of Canada. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000; 92:205–221.13. Benjamin RS, Choi H, Macapinlac HA, Burgess MA, Patel SR, Chen LL, et al. We should desist using RECIST, at least in GIST. J Clin Oncol. 2007; 25:1760–1764.14. Choi H, Charnsangavej C, de Castro Faria S, Tamm EP, Benjamin RS, Johnson MM, et al. CT evaluation of the response of gastrointestinal stromal tumors after imatinib mesylate treatment: a quantitative analysis correlated with FDG PET findings. AJR Am J Roentgenol. 2004; 183:1619–1628.15. Schiavon G, Ruggiero A, Schoffski P, van der Holt B, Bekers DJ, Eechoute K, et al. Tumor volume as an alternative response measurement for imatinib treated GIST patients. PLoS One. 2012; 7:e48372.16. Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010; 30:52–60.17. Choi H, Faria S, Benjamin R, Podoloff D, Macapinlac H, Charnsangavej C. Monitoring treatment effects of STI-571 on gastrointestinal stromal tumors (GIST) with CT and PET: a quantitative analysis. Chicago, IL: Presented at Radiological Society of North America Scientific Program;2002.18. Prasad SR, Jhaveri KS, Saini S, Hahn PF, Halpern EF, Sumner JE. CT tumor measurement for therapeutic response assessment: comparison of unidimensional, bidimensional, and volumetric techniques initial observations. Radiology. 2002; 225:416–419.19. Hong X, Choi H, Loyer EM, Benjamin RS, Trent JC, Charnsangavej C. Gastrointestinal stromal tumor: role of CT in diagnosis and in response evaluation and surveillance after treatment with imatinib. Radiographics. 2006; 26:481–495.20. Kim HC, Lee JM, Choi SH, Han H, Kim SS, Lee SH, et al. Cystic changes in intraabdominal extrahepatic metastases from gastrointestinal stromal tumors treated with imatinib. Korean J Radiol. 2004; 5:157–163.21. Chen MY, Bechtold RE, Savage PD. Cystic changes in hepatic metastases from gastrointestinal stromal tumors (GISTs) treated with Gleevec (imatinib mesylate). AJR Am J Roentgenol. 2002; 179:1059–1062.22. Oh JS, Lee JL, Kim MJ, Ryu MH, Chang HM, Kim TW, et al. Neoadjuvant imatinib in locally advanced gastrointestinal stromal tumors of the stomach: report of three cases. Cancer Res Treat. 2006; 38:178–183.23. Bechtold RE, Chen MY, Stanton CA, Savage PD, Levine EA. Cystic changes in hepatic and peritoneal metastases from gastrointestinal stromal tumors treated with Gleevec. Abdom Imaging. 2003; 28:808–814.24. Reynoso D. Bim mediates imatinib-induced apoptosis of gastrointestinal stromal tumors: Translational implications. UT GSBS Dissertations and Theses (Open Access). 2012. p. 11–12.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Imatinib-induced hepatitis treated by corticosteroids in a patient with metastatic gastrointestinal stromal tumor
- Two different KIT mutations may lead to different responses to imatinib in metastatic gastrointestinal stromal tumor
- A Case of Generalized Keratosis Pilaris Induced by Imatinib Mesylate
- Postoperative Cure for Metastatic Gastrointestinal Stromal Tumor
- Imatinib-induced DRESS Syndrome in Gastrointestinal Stromal Tumor