J Korean Radiol Soc.
1998 Mar;38(3):459-463. 10.3348/jkrs.1998.38.3.459.
Spontaneous Pneumomediastinum on CT: Related Condition and its Clinical Significance
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine.
- KMID: 2201402
- DOI: http://doi.org/10.3348/jkrs.1998.38.3.459
Abstract
-
PURPOSE: To tabulate underlying disease and to assess the clinical significance of CT-diagnosed spontaneouspneumonediastinum.
MATERIALS AND METHODS
We retrospectively reviewed CT scans and medical records of 11consecutive patients with spontaneous pneumomediastinum, and analyzed their clinical history and course, and infive cases, pulmonary function. CT scans of 126 patients with idiopathic pulmonary fibrosis (IPF) collected whilethe 11 consecutive patients were being treated were analyzed for the prevalence of pneumomediastinum. We analyzedCT findings with respect to the amount and distribution of air in the mediastinum, and the presence or absence ofair outside the mediastinum.
RESULTS
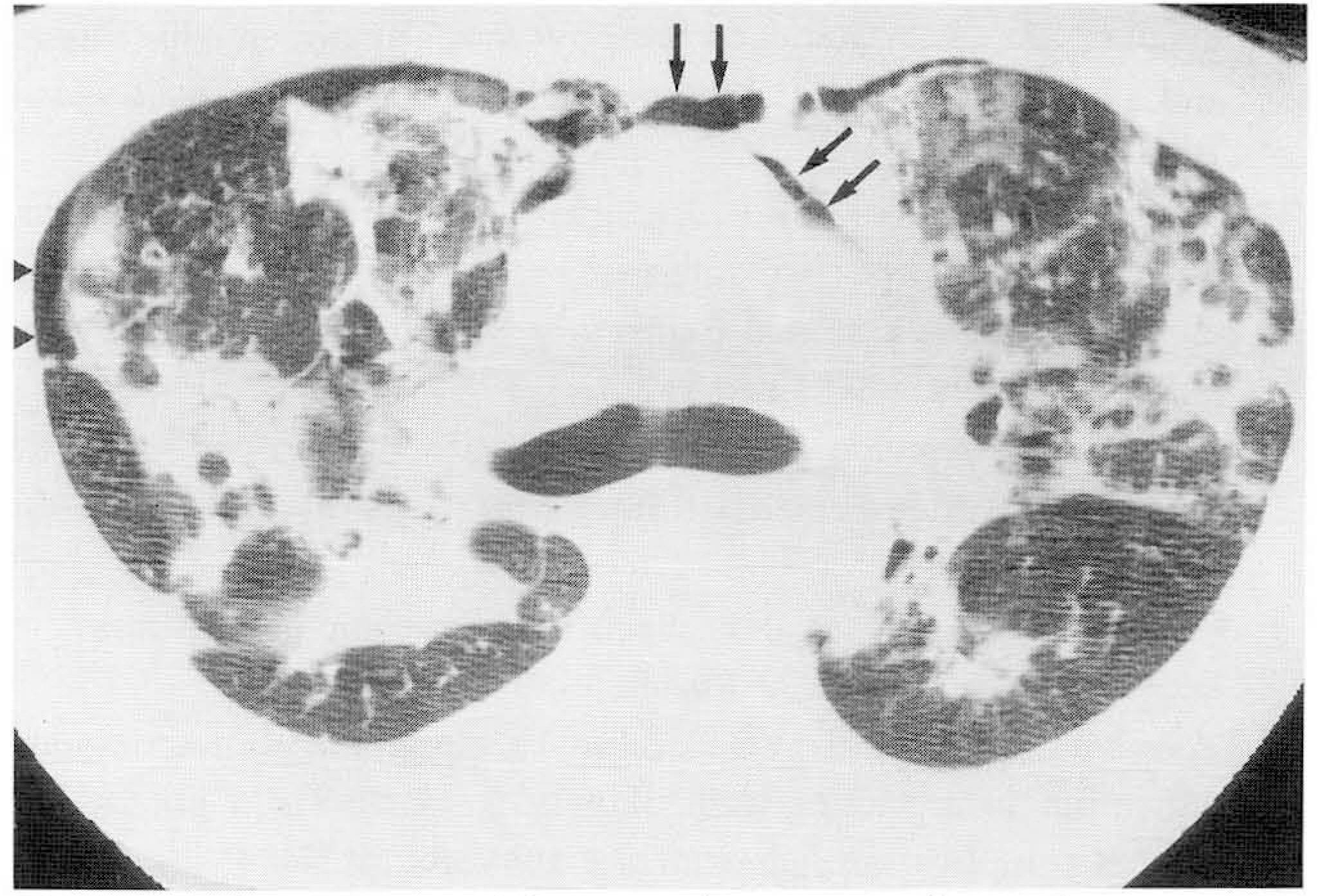
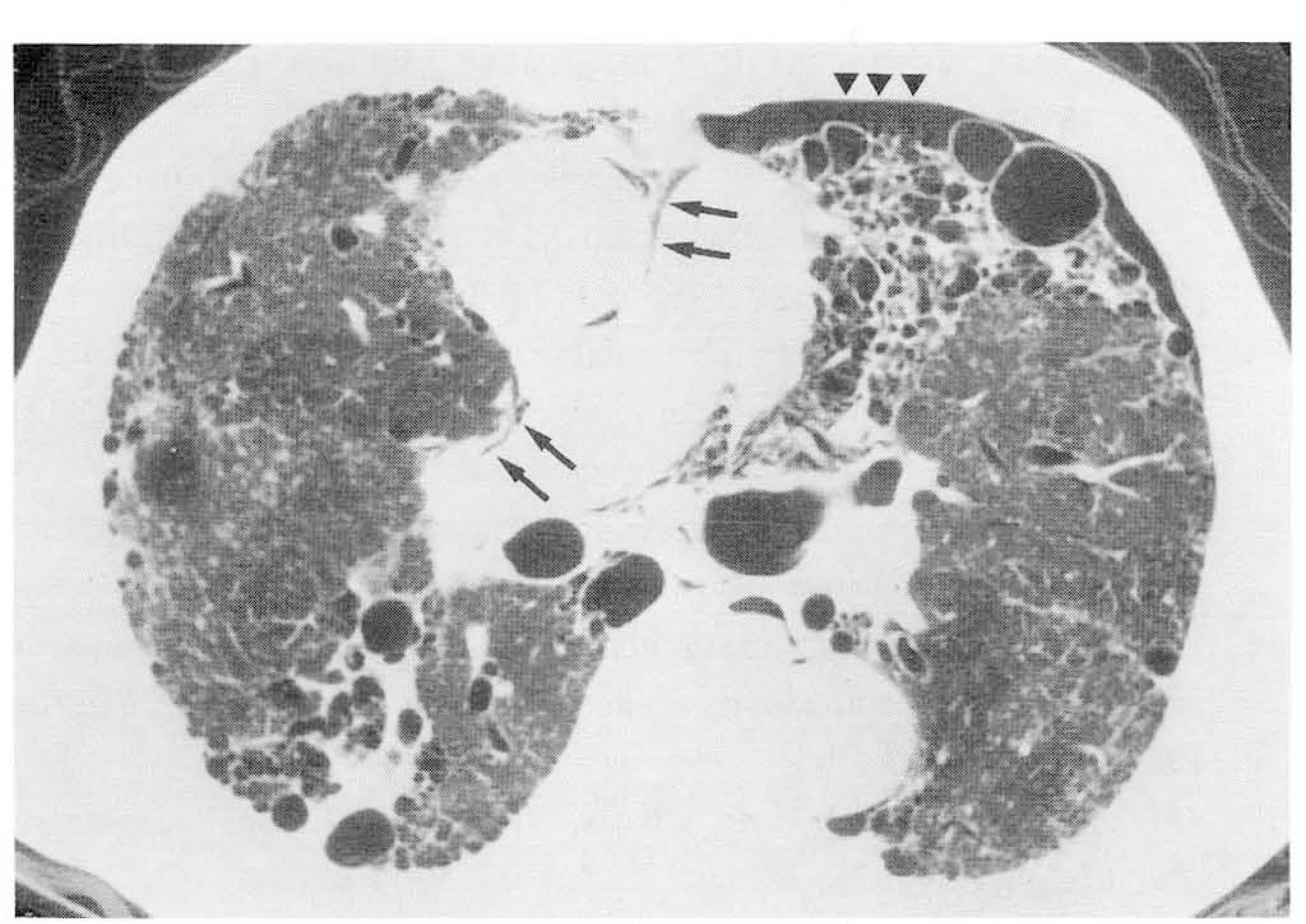
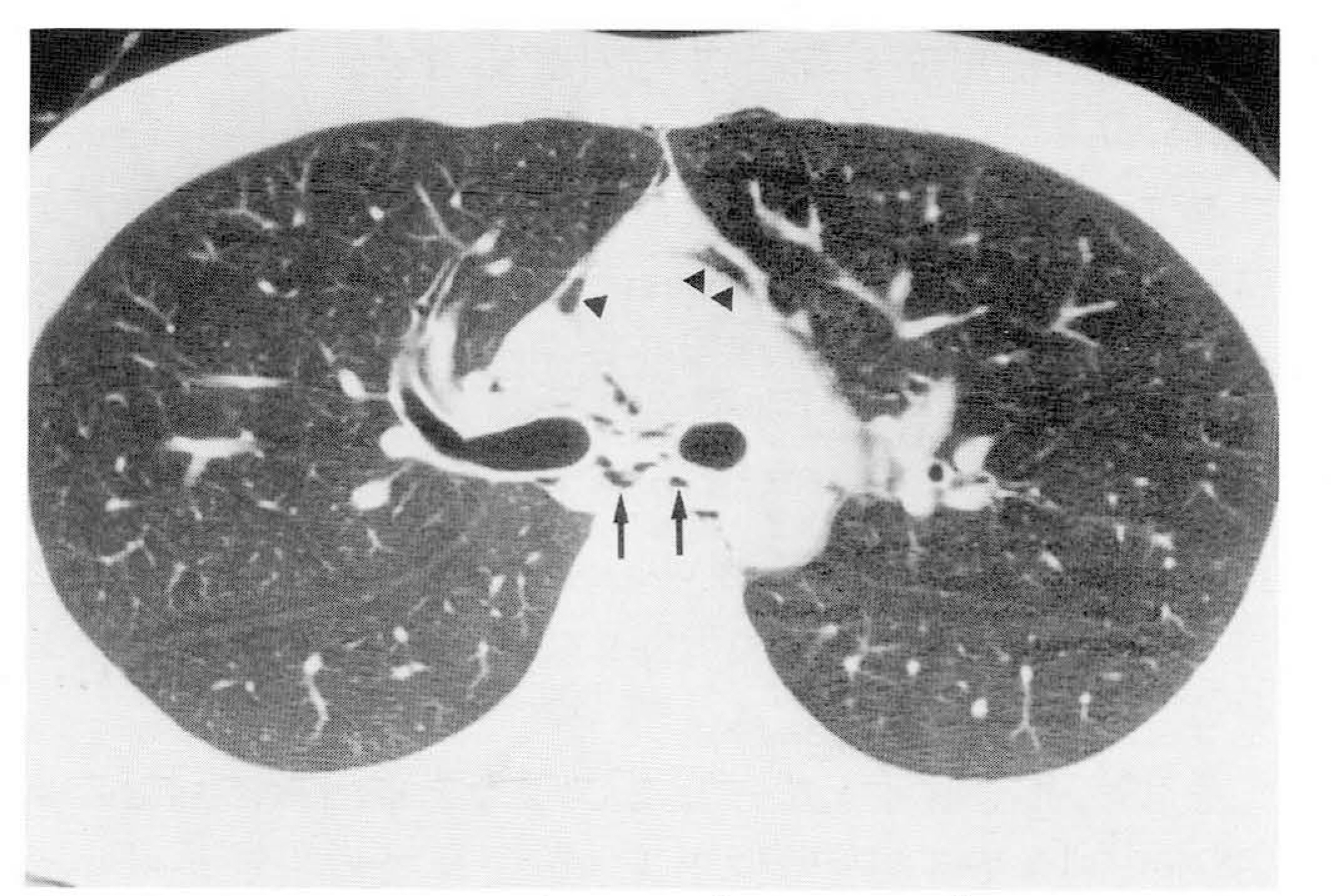
In the 11 patients, underlying diseases were IPF (n=4), bronchiolitisobliterans organizing pneumonia (BOOP)(n=2), bronchiectasis (n=2), tuberculous tracheal stenosis (n=1), andpulmonary tuberculosis with bullous emphysema (n=1); there was one without associated disease. Of the 126 patientswith IPF, four (3.2%) showed spontaneous pneumomediastinum. All ten with underlying diseases had severe dyspnea.In five patients, a pulmonary function test showed marked impairment. Two of four patients with IPF and both withBOOP died within 2 months of CT scanning, whereas the remaining six showed clinical improvement. The detectionrate of pneumomediastinum on plain chest radiograph was 82% (9/11). CT showed that mediastinal air was mostfrequently found in the retrosternal space. There were four cases of pneumothorax and two of subcutaneousemphysema.
CONCLUSION
Spontaneous pneumomediastinum might be associated with idiopathic pulmonary fibrosis andmight be a poor prognostic factor in patients with IPF or BOOP.
Keyword
MeSH Terms
Figure
Reference
-
1.Holmes KD., McGuirt WF. Spontaneous pneumomediastinum: evaluation and treatment. J Fam Pract. 1990. 31:422–499.2.Abolnik I., Lossos IS., Breuer R. Spontaneous pneumomediastinum, a report of 25 cases. Chest. 1991. 100:93–95.3.Reeder SR. Subcutaneous emphysema, pneumomediastinum, and pneumothorax in labor and delivery. Am J Obstet Gynecol. 1986. 154:487–489.
Article4.Man ο JC., Terra-Filho J., Silva CA. Pneumomediastinum, pneumothorax and subcutaneous emphysema following the measurement of maximal expiratory pressure in a normal subject. Chest. 1990. 98:1530–1532.
Article5.de la Fuente Aguado J., Roman F., Hernaez JM., Provencio M., de Letona JM. Pneumomediastinum after belching. Lancet. 1990. 336:1390.6.Cicuttini FM., Fraser KJ. Recurrent pneumomediastinum in adult dermatomyositis. J Rheum. 1989. 16:384–386.7.Weathers LS., Brooks WG., Declue TJ. Spontaneous pneumomediastinum in a patient with diabetic ketoacidosis: a potentially hidden complication. South Med J. 1995. 88:483–484.8.O'Connor I., Thomas GO. Spontaneous pneumomediastinum in a patient with fibrosing alveolitis. Resp Med. 1993. 87:313–314.9.Shahar J., Angelillo VA. Catamenial pneumomediastinum. Chest. 1986. 90:776–777.
Article10.Amorosa JK., Schaffer RM., Smith PR., Cohen JR., Robinson R. Sarcoidosis and mediastinal emphysema. Radiology. 1978. 127:314.
Article11.Munsell WP. Pneumomediastinum. A report of 28 cases and review of the literature. JAMA. 1967. 202:689–693.
Article12.Yellin A., Gapany-Gapanavicius M., Leiberman Y. Spontaneous pneumomediastinum: is it a rare cause of chest pain? Thorax. 1983. 38:383–385.
Article13.Shennib HF., Barkun AN., Blundell PE. Surgical decompression of a tension pneumomediastinum, a ventilatory complication of status asthmaticus. Chest. 1988. 93:1301–1302.14.Beyers JA., Melonas CF. The visible wall of a main bronchus: a new radiologic sign of pneumomediastinum. Br J Radiol. 1987. 60:877–879.15.Fujiwara T. Pneumomediastinum in pulmonary fibrosis, detection by computed tomography. Chest. 1993. 104:44–46.16.Yellin A., Gapany-Gapanavicius M., Lieberman Y. Spontaneous pneumomediastinum: is it a rare cause of chest pain? Thorax. 1983. 38:383–385.
Article17.Kerr IH. Interstitial lung disease: the role of the radiologist. Clin Radiol. 1984. 35:1–7.
Article18.Macklin MT., Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory disease and other conditions: an interpretation of the clinical literature in the light of laboratory experiment. Medicine. 1944. 23:281–358.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Pneumomediastinum Complicating with Asthma
- A Case of Spontaneous Pneumomediastinum and Pneumopericardium in a Patient with Acute Exacerbation of Idiopathic Pulmonary Fibrosis
- A case of spontaneous pneumomediastinum caused by endobronchial tuberculosis
- Perifissural Air Seen in the Pneumomediastinum on MDCT: the Incidence and Clinical Features
- A Case of Tracheomegaly and Recurrent Pneumomediastinum Combined with Pulmonary Fibrosis