J Korean Soc Endocrinol.
2006 Aug;21(4):328-332. 10.3803/jkes.2006.21.4.328.
A Case of Idiopathic Myelofibrosis Associated with Acromegaly Patient
- Affiliations
-
- 1Department of Internal Medicine, Kosin University College of Medicine, Korea.
- 2Department of Clinical Pathology, Kosin University College of Medicine, Korea.
- 3Department of Pathology, Kosin University College of Medicine, Korea.
- 4Department of Diagnostic Radiology, Kosin University College of Medicine, Korea.
- KMID: 2200848
- DOI: http://doi.org/10.3803/jkes.2006.21.4.328
Abstract
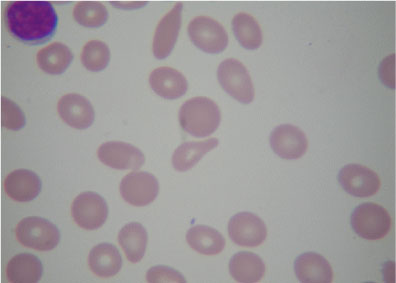
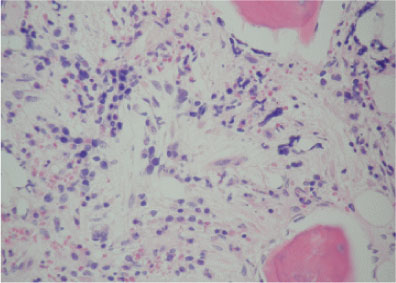
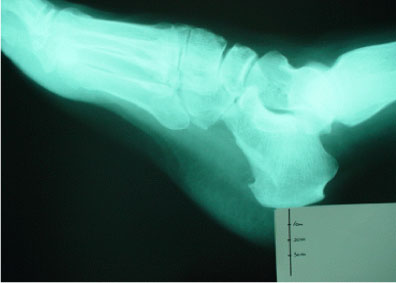
- Acromegaly is a chronic condition resulting from the excessive secretion of growth hormone and insulin like growth factor 1, generally from pituitary adenoma. Although there have been several reports suggesting the possible association of hematologic malignancies with acromegaly, myelofibrosis with acromegaly is very rare. Here we report 54-year-old male patient with myelofibrosis accompanied with acromegaly. We treated this patient with low dose thalidomide (50 mg/day) and prednisone (30 mg/day). We reported this case with literature review.
MeSH Terms
Figure
Reference
-
1. Colao A, Ferone D, Marzullo P, Lombardi G. Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocr Rev. 2004. 25:102–152.2. Melmed S. Acromegaly. N Engl J Med. 1990. 322:966–977.3. Tefferi A. Myelofibrosis with myeloid metaplasia. N Engl J Med. 2000. 342:1255–1265.4. Au WY, Chow WS, Lam KS, Ko GT, Cockram CS, Kwong YL. Acute leukaemia in acromegaly patients. Br J Haematol. 2000. 110:871–873.5. Murphy PT, Ahmed N, Hassen HT. Chronic myeloid leukemia and acromegaly in POEMS syndrome. Leuk Res. 2002. 26:1135–1137.6. Teramoto S, Ouchi V. Polycythemia vera in acromegaly. Ann Intern Med. 1997. 126:87.7. Imai Y, Akiyama N, Hanazono Y, Inamori K, Mitani K, Hirai H, Nagai R, Yazaki Y. Successful treatment of splenomegaly and anemia by VP therapy in idiopathic myelofibrosis complicated with acromegaly: a case report. Rhinsho Ketsueki. 1995. 36:1233–1236.8. Clemmons DR, Van Wyk JJ. Somatomedin-C and platelet-derived growth factor stimulate human fibroblast replication. J Cell Physiol. 1981. 106:361–367.9. Arya KR, Pathare AV, Chadda M, Menon PS. Diabetes in acromegaly. a study of 34 cases. J Indian Med Assoc. 1997. 95:546–547.10. Wright AD, Hill Dm, Lowly C, Fraser TR. Mortality in acromegaly. Q J Med. 1970. 39:1–6.11. Alexander L, Appleton D, Hall R, Ross WM, Wilkinson R. Epidemiology of acromegaly in the Newcastle region. Clin Endocrinol. 1980. 12:71–79.12. Bengtsson BA, Eden S, Ernest I, Oden A, Sjogren B. Epidemiology and long-term survival in acromegaly. Acta Med Scand. 1988. 223:327–335.13. Au WY, Chow WS, Lam KS, Ko GT, Cockram CS, Kwong YL. Acute leukemia in acromegaly patients. Br J Haematol. 2000. 110:871–873.14. Kvasnicka HM, Thiele J, Werden C, Zankovich R, Diehl V, Fischer R. Prognostic factors in idiopathic (primary) osteomyelofibrosis. Cancer. 1997. 80:708–719.15. Rupoli S, Da Lio L, Sisti S, Campanati G, Salvi A, Brianzoni MF, D'Amico S, Cinciripini A, Leoni P. Primary myelofibrosis: a detailed statistical analysis of the clinicopathological variables influencing survival. Ann Hematol. 1994. 68:205–212.16. Cervantes F, Barosi G, Demory JL, Reilly J, Guarnone R, Dupriez B, Pareira A, Montserrat E. Myelofibrosis with myeloid metaplasia in young individuals: disease characteristics, prognostic factors and identification of risk groups. Br J Haematol. 1998. 102:684–690.17. Dimopoulos MA, Eleutherakis-Papaiakovou V. Adverse effects of thalidomide administration in patients with neoplastic diseases. Am J Med. 2004. 117:508–515.18. Strupp C, Germing U, Scherer A, Kundgen A, Modder U, Gattermann N, Haas R. Thalidomide for the treatment of idiopathic myelofibrosis. Eur Haematol. 2004. 72:52–57.19. Mesa RA, Silverstein MN, Jacobsen SJ, Wollan PC, Tefferi A. Population-based incidence and survival figures in essential thrombocythemia and agnogenic myeloid metaplasia: an Olmsted County Study, 1976-1995. Am J Hematol. 1999. 61:10–15.20. Marchetti M, Barosi G, Balestri F, Viarengo G, Gentili S, Barulli S, Demory JL, Ilariucci F, Volpe A, Bordessoule D, Grossi A, Le Bousse-Kerdiles MC, Caenazzo A, Pecci A, Falcone A, Broccia G, Bendotti C, Bauduer F, Buccisano F, Dupriez B. Low-dose thalidomide ameliorates cytopenias and splenomegaly in myelofibrosis with myeloid metaplasia: a phase II trial. J Clin Oncol. 2004. 22:424–431.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Myelofibrosis Mimicking Malignant Lymphoma in Computed Tomography of Abdomen: A Case of Autoimmune Myelofibrosis associated with Systemic Lupus Erythematosus Showing Extensive Lymphadenopathy and A Case of Chronic Idiopathic Myelofibrosis wit
- Pyoderma Gangrenosum Associated with Idiopathic Myelofibrosis
- A Case of Cutaneous Extramedullary Hematopoiesis in Idiopathic Myelofibrosis
- Chronic Idiopathic Myelofibrosis Presenting as Cauda Equina Compression due to Extramedullary Hematopoiesis: A Case Report
- A Novel Jumping Translocation of 12q21 in a Patient with Chronic Idiopathic Myelofibrosis