J Korean Acad Prosthodont.
2012 Apr;50(2):99-105. 10.4047/jkap.2012.50.2.99.
Three-dimensional finite element analysis for influence of marginal bone resorption on stress distribution in internal conical joint type implant fixture
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry, Pusan National University, Yangsan, Korea. cmjeong@pusan.ac.kr
- 2Osstem Implant Research Center, Busan, Korea.
- KMID: 2195498
- DOI: http://doi.org/10.4047/jkap.2012.50.2.99
Abstract
- PURPOSE
The change of the marginal bone around dental implants have significance not only for the functional maintenance but also for the esthetic success of the implant. The purpose of this study was to investigate the load transfer of internal conical joint type implant according to marginal bone resorption by using the three-dimensional finite element analysis model.
MATERIALS AND METHODS
The internal conical joint type system was selected as an experimental model. Finite element models of bone/implant/prosthesis complex were constructed. A load of 300 N was applied vertically beside 3 mm of implant axis.
RESULTS
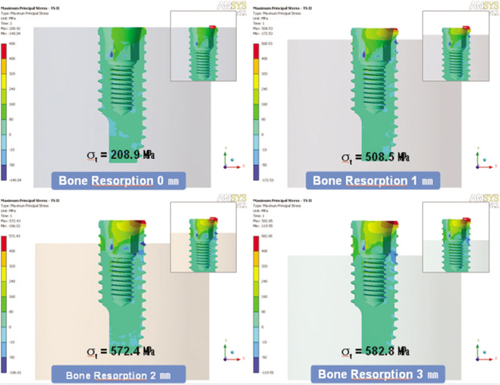
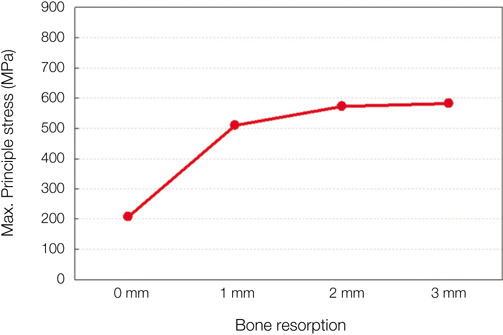
The pattern of stress distribution according to marginal bone resorption was similar. The maximum equivalent stress of implant was increase according to marginal bone resorption and the largest maximum equivalent stress was shown at model of 1 mm marginal bone resorption. Although marginal bone loss more than 1mm was occurred increasing of stress, the width of the stress increase was decreasing.
CONCLUSION
According to these results, the exposure of thin neck portion of internal conical joint type implant is most important factor in stress increasing.
Keyword
MeSH Terms
Figure
Reference
-
1. Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants: the Toronto study. Part III: Problems and complications encountered. J Prosthet Dent. 1990. 64:185–194.
Article2. Henry PJ, Laney WR, Jemt T, Harris D, Krogh PH, Polizzi G, Zarb GA, Herrmann I. Osseointegrated implants for single-tooth replacement: a prospective 5-year multicenter study. Int J Oral Maxillofac Implants. 1996. 11:450–455.3. Kitamura E, Stegaroiu R, Nomura S, Miyakawa O. Biomechanical aspects of marginal bone resorption around osseointegrated implants: considerations based on a three-dimensional finite element analysis. Clin Oral Implants Res. 2004. 15:401–412.
Article4. Quirynen M, Naert I, van Steenberghe D. Fixture design and overload influence marginal bone loss and fixture success in the Braånemark system. Clin Oral Implants Res. 1992. 3:104–111.
Article5. Ericsson I, Persson LG, Berglundh T, Marinello CP, Lindhe J, Klinge B. Different types of inflammatory reactions in peri-implant soft tissues. J Clin Periodontol. 1995. 22:255–261.
Article6. Berglundh T, Lindhe J. Dimension of the periimplant mucosa. Biological width revisited. J Clin Periodontol. 1996. 23:971–973.7. Hermann JS, Schoolfield JD, Schenk RK, Buser D, Cochran DL. Influence of the size of the microgap on crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged implants in the canine mandible. J Periodontol. 2001. 72:1372–1383.
Article8. Schwartz-Arad D, Herzberg R, Levin L. Evaluation of long-term implant success. J Periodontol. 2005. 76:1623–1628.
Article9. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986. 1:11–25.10. Smith DE, Zarb GA. Criteria for success of osseointegrated endosseous implants. J Prosthet Dent. 1989. 62:567–572.
Article11. Goodacre CJ, Kan JY, Rungcharassaeng K. Clinical complications of osseointegrated implants. J Prosthet Dent. 1999. 81:537–552.
Article12. Barbier L, Schepers E. Adaptive bone remodeling around oral implants under axial and nonaxial loading conditions in the dog mandible. Int J Oral Maxillofac Implants. 1997. 12:215–223.13. Wyatt CC, Zarb GA. Bone level changes proximal to oral implants supporting fixed partial prostheses. Clin Oral Implants Res. 2002. 13:162–168.
Article14. Misch CE, Suzuki JB, Misch-Dietsh FM, Bidez MW. A positive correlation between occlusal trauma and peri-implant bone loss: literature support. Implant Dent. 2005. 14:108–116.
Article15. Isidor F. Influence of forces on peri-implant bone. Clin Oral Implants Res. 2006. 17:8–18.
Article16. Saadoun AP, Le Gall M, Kricheck M. Microbial infections and occlusal overload: causes of failure in osseointegrated implants. Pract Periodontics Aesthet Dent. 1993. 5:11–20.17. Lindhe J, Berglundh T, Ericsson I, Liljenberg B, Marinello C. Experimental breakdown of peri-implant and periodontal tissues. A study in the beagle dog. Clin Oral Implants Res. 1992. 3:9–16.
Article18. Lang NP, Brägger U, Walther D, Beamer B, Kornman KS. Ligature-induced peri-implant infection in cynomolgus monkeys. I. Clinical and radiographic findings. Clin Oral Implants Res. 1993. 4:2–11.
Article19. Davies JE. Mechanisms of endosseous integration. Int J Prosthodont. 1998. 11:391–401.20. Wiskott HW, Belser UC. Lack of integration of smooth titanium surfaces: a working hypothesis based on strains generated in the surrounding bone. Clin Oral Implants Res. 1999. 10:429–444.
Article21. Levine RA, Clem DS 3rd, Wilson TG Jr, Higginbottom F, Solnit G. Multicenter retrospective analysis of the ITI implant system used for single-tooth replacements: results of loading for 2 or more years. Int J Oral Maxillofac Implants. 1999. 14:516–520.22. Maeda Y, Satoh T, Sogo M. In vitro differences of stress concentrations for internal and external hex implant-abutment connections: a short communication. J Oral Rehabil. 2006. 33:75–78.
Article23. Pieri F, Aldini NN, Marchetti C, Corinaldesi G. Influence of implant-abutment interface design on bone and soft tissue levels around immediately placed and restored single-tooth implants: a randomized controlled clinical trial. Int J Oral Maxillofac Implants. 2011. 26:169–178.24. Merz BR, Hunenbart S, Belser UC. Mechanics of the implant-abutment connection: an 8-degree taper compared to a butt joint connection. Int J Oral Maxillofac Implants. 2000. 15:519–526.25. Ash MM Jr. Wheeler's dental anatomy, physiology and occlusion. 1993. 7th ed. WB Saunders Co.;218–231.26. Welsch G, Boyer R, Collings EW. Materials properties handbook: titanium alloys. 1994. Materials Park, OH: ASM International.27. Holt JM, Mindlin H, Ho CY. Purdue University. Center for information and numerical data analysis and synthesis. Structural alloys handbook. 1994. West Lafayette, IN: CINDAS/Purdue University.28. O'Brein WJ. Dental materials and their selection. 1997. 2nd ed. Chicago: Quintessence pub. Co.;259–272.29. Cibirka RM, Razzoog ME, Lang BR, Stohler CS. Determining the force absorption quotient for restorative materials used in implant occlusal surfaces. J Prosthet Dent. 1992. 67:361–364.
Article30. Chun HJ, Shin HS, Han CH, Lee SH. Influence of implant abutment type on stress distribution in bone under various loading conditions using finite element analysis. Int J Oral Maxillofac Implants. 2006. 21:195–202.31. Choi JU, Jeong CM, Jeon YC, Lim JS, Jeong HC, Eom TG. Influnence of tungsten carbide/carbon coating on the preload of implant abutment screws. J Korean Acad Prosthodont. 2006. 44:229–242.32. Lim JY, Cho JH, Jo KW. Influence of crestal module design on marginal bone stress around dental implant. J Korean Acad Prosthodont. 2010. 48:224–231.
Article33. Rangert B, Krogh PH, Langer B, Van Roekel N. Bending overload and implant fracture: a retrospective clinical analysis. Int J Oral Maxillofac Implants. 1995. 10:326–334.34. Norton RL. Machine design: and integrated approach. 1995. 1th ed. Pearson eduction;43–45.35. Dowling NE. Mechanical behavior of materials : engineering for deformation, fracture, and fatigue. 1993. Englewood Cliffs: Prentice-Hall International Inc;252.36. Tada S, Stegaroiu R, Kitamura E, Miyakawa O, Kusakari H. Influence of implant design and bone quality on stress/strain distribution in bone around implants: a 3-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2003. 18:357–368.37. Petrie CS, Williams JL. Comparative evaluation of implant designs: influence of diameter, length, and taper on strains in the alveolar crest. A three-dimensional finite-element analysis. Clin Oral Implants Res. 2005. 16:486–494.
Article38. Hänggi MP, Hänggi DC, Schoolfield JD, Meyer J, Cochran DL, Hermann JS. Crestal bone changes around titanium implants. Part I: A retrospective radiographic evaluation in humans comparing two non-submerged implant designs with different machined collar lengths. J Periodontol. 2005. 76:791–802.
Article39. Holmgren EP, Seckinger RJ, Kilgren LM, Mante F. Evaluating parameters of osseointegrated dental implants using finite element analysis-a two-dimensional comparative study examining the effects of implant diameter, implant shape, and load direction. J Oral Implantol. 1998. 24:80–88.
Article40. Matsushita Y, Kitoh M, Mizuta K, Ikeda H, Suetsugu T. Two-dimensional FEM analysis of hydroxyapatite implants: diameter effects on stress distribution. J Oral Implantol. 1990. 16:6–11.41. Chun HJ, Cheong SY, Han JH, Heo SJ, Chung JP, Rhyu IC, Choi YC, Baik HK, Ku Y, Kim MH. Evaluation of design parameters of osseointegrated dental implants using finite element analysis. J Oral Rehabil. 2002. 29:565–574.
Article42. Hansson S, Werke M. The implant thread as a retention element in cortical bone: the effect of thread size and thread profile: a finite element study. J Biomech. 2003. 36:1247–1258.
Article43. Clelland NL, Gilat A. The effect of abutment angulation on stress transfer for an implant. J Prosthodont. 1992. 1:24–28.
Article44. Gotfredsen K, Berglundh T, Lindhe J. Bone reactions adjacent to titanium implants with different surface characteristics subjected to static load. A study in the dog (II). Clin Oral Implants Res. 2001. 12:196–201.
Article45. O'Brien GR, Gonshor A, Balfour A. A 6-year prospective study of 620 stress-diversion surface (SDS) dental implants. J Oral Implantol. 2004. 30:350–357.46. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981. 10:387–416.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influence of implant-abutment interface design, implant diameter and prosthetic table width on strength of implant-abutment interface: three-dimensional finite element analysis
- Stress analysis of supporting tissues and implants according to implant fixture shapes and implant-abutment connections
- A study on the various implant systems using the finite element stress analysis
- Finite element stress analysis of implant prosthesis according to connection types of implant-abutment
- Finite element stress analysis of implant prosthesis with internal connection between the implant and the abutment