J Korean Med Assoc.
2012 Jul;55(7):666-675. 10.5124/jkma.2012.55.7.666.
Recent trends in pharmacologic treatment of cancer pain
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Korea University College of Medicine, Seoul, Korea. anejhkim@korea.ac.kr
- KMID: 2192729
- DOI: http://doi.org/10.5124/jkma.2012.55.7.666
Abstract
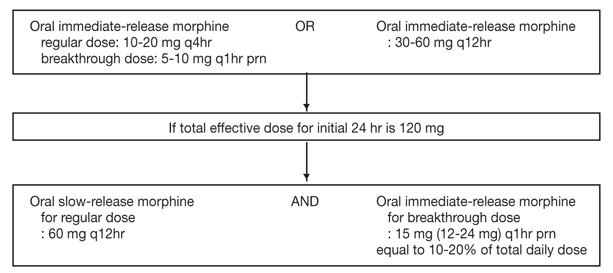
- Cancer pain is among the most undesirable side effects and complications for cancer patients. Severe cancer pain acts as physical and psychological stress and makes it difficult for patients to perform daily activities. Uncontrolled cancer pain can be emotionally devastating to patients. However, cancer pain can be controlled with pharmacologic treatment. Traditionally, cancer pain was treated according to the WHO three-step analgesic ladder based on the severity of pain. Recently, it has become to administer weak opioids as well as non-opioid analgesics to patients with mild pain. For moderate pain, weak opioids or strong opioids can be used. Non-opioid analgesics and adjuvant analgesics can be used as an adjuvant to opioids for all severities of cancer pain. Effective cancer pain management depends on the proper selection of a drug, dose, and route and depends on treatment of common side effects associated with the medication. The usage of medication should be individualized to each patient. If necessary, we may use other modalities such as radiotherapy, nerve block, and non-pharmacologic interventions for cancer pain control. The goal of treatment of cancer pain is to obtain complete or partial pain relief with tolerable side effects of the medication, and ultimately, to improve the quality of life of cancer patients.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Prescribing Opioids for Chronic Pain
Dong Uk Yoon, Ung Gu Kang
J Korean Neuropsychiatr Assoc. 2019;58(3):182-191. doi: 10.4306/jknpa.2019.58.3.182.Opioids use for chronic noncancer pain
In Cheol Hwang, Jae Yong Shim
J Korean Med Assoc. 2013;56(8):711-717. doi: 10.5124/jkma.2013.56.8.711.
Reference
-
1. Ministry of Health & Welfare. Cancer pain management guideline. 2012. 5th ed. Seoul: Ministry of Health & Welfare.2. Park JM. Korean Society of Anesthesiologists Anesthesiologists. Cancer pain. Anesthesiology & pain medicine. 2010. 2nd ed. Seoul: Ryo Moon Gak;379–398.3. Azevedo Sao Leao Ferreira K, Kimura M, Jacobsen Teixeira M. The WHO analgesic ladder for cancer pain control, twenty years of use. How much pain relief does one get from using it? Support Care Cancer. 2006. 14:1086–1093.
Article4. National Comprehensive Cancer Network. NCCN clinical practice guideline in oncology: adult cancer pain. 2012. 1. Fort Washington: National Comprehensive Cancer Network.5. American Pain Society Quality of Care Committee. Quality improvement guidelines for the treatment of acute pain and cancer pain. JAMA. 1995. 274:1874–1880.6. Yoon DM. Korean Pain Society. Cancer pain. Pain medicine. 2007. 3rd ed. Seoul: Koonja;425–442.7. Harris JT, Suresh Kumar K, Rajagopal MR. Intravenous morphine for rapid control of severe cancer pain. Palliat Med. 2003. 17:248–256.
Article8. Portenoy RK. Treatment of cancer pain. Lancet. 2011. 377:2236–2247.
Article9. Ripamonti CI, Bandieri E, Roila F. ESMO Guidelines Working Group. Management of cancer pain: ESMO Clinical Practice Guidelines. Ann Oncol. 2011. 22:Suppl 6. vi69–vi77.
Article10. Stockler M, Vardy J, Pillai A, Warr D. Acetaminophen (paracetamol) improves pain and well-being in people with advanced cancer already receiving a strong opioid regimen: a randomized, double-blind, placebo-controlled cross-over trial. J Clin Oncol. 2004. 22:3389–3394.
Article11. Israel FJ, Parker G, Charles M, Reymond L. Lack of benefit from paracetamol (acetaminophen) for palliative cancer patients requiring high-dose strong opioids: a randomized, double-blind, placebo-controlled, crossover trial. J Pain Symptom Manage. 2010. 39:548–554.
Article12. McNicol E, Strassels SA, Goudas L, Lau J, Carr DB. NSAIDS or paracetamol, alone or combined with opioids, for cancer pain. Cochrane Database Syst Rev. 2005. (1):CD005180.
Article13. Bruera E, Kim HN. Cancer pain. JAMA. 2003. 290:2476–2479.
Article14. Stevens RA, Ghazi SM. Routes of opioid analgesic therapy in the management of cancer pain. Cancer Control. 2000. 7:132–141.
Article15. Ripamonti C, Bandieri E. Pain therapy. Crit Rev Oncol Hematol. 2009. 70:145–159.
Article16. Foley KM. The treatment of pain in the patient with cancer. CA Cancer J Clin. 1986. 36:194–215.
Article17. Kornick CA, Santiago-Palma J, Khojainova N, Primavera LH, Payne R, Manfredi PL. A safe and effective method for converting cancer patients from intravenous to transdermal fentanyl. Cancer. 2001. 92:3056–3061.
Article18. Meuser T, Pietruck C, Radbruch L, Stute P, Lehmann KA, Grond S. Symptoms during cancer pain treatment following WHO-guidelines: a longitudinal follow-up study of symptom prevalence, severity and etiology. Pain. 2001. 93:247–257.
Article19. McNicol E, Horowicz-Mehler N, Fisk RA, Bennett K, Gialeli-Goudas M, Chew PW, Lau J, Carr D. Americal Pain Society. Management of opioid side effects in cancer-related and chronic noncancer pain: a systematic review. J Pain. 2003. 4:231–256.
Article20. Holzer P, Ahmedzai SH, Niederle N, Leyendecker P, Hopp M, Bosse B, Spohr I, Reimer K. Opioid-induced bowel dysfunction in cancer-related pain: causes, consequences, and a novel approach for its management. J Opioid Manag. 2009. 5:145–151.
Article21. Stone P, Minton O. European Palliative Care Research collaborative pain guidelines. Central side-effects management: what is the evidence to support best practice in the management of sedation, cognitive impairment and myoclonus? Palliat Med. 2011. 25:431–441.
Article22. Tassinari D, Drudi F, Carloni F, Possenti C, Santelmo C, Castellani C. Neuropathic pain in oncology. Novel evidence for clinical practice. Recenti Prog Med. 2011. 102:220–227.23. Saarto T, Wiffen PJ. Antidepressants for neuropathic pain: a Cochrane review. J Neurol Neurosurg Psychiatry. 2010. 81:1372–1373.
Article24. Wiffen P, Collins S, McQuay H, Carroll D, Jadad A, Moore A. Anticonvulsant drugs for acute and chronic pain. Cochrane Database Syst Rev. 2005. (3):CD001133.
Article25. Mercadante SL, Berchovich M, Casuccio A, Fulfaro F, Mangione S. A prospective randomized study of corticosteroids as adjuvant drugs to opioids in advanced cancer patients. Am J Hosp Palliat Care. 2007. 24:13–19.
Article26. Vasudev NS, Brown JE. Medical management of metastatic bone disease. Curr Opin Support Palliat Care. 2010. 4:189–194.
Article27. Slatkin NE, Rhiner M. Ketamine in the treatment of refractory cancer pain: case report, rationale, and methodology. J Support Oncol. 2003. 1:287–293.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Cancer Pain: Epidemiology and Pharmacologic Treatment
- Practical issues and research trends of oncofertility in gynecologic cancer
- THE MANAGEMENT OF ORAL CANCER PAIN
- A Case Report of Traumatic neuropathic Pain Patient
- Identifying Trends in Oncology Research through a Bibliographic Analysis of Cancer Research and Treatment