J Korean Neurosurg Soc.
2015 Sep;58(3):242-247. 10.3340/jkns.2015.58.3.242.
Brain Activation Evoked by Sensory Stimulation in Patients with Spinal Cord Injury : Functional Magnetic Resonance Imaging Correlations with Clinical Features
- Affiliations
-
- 1Department of Neurosurgery, College of Medicine, Inha University, Incheon, Korea. nsyoon@gmail.com
- 2Department of Neurosurgery, Guro Cham Teun Teun Hospital, Seoul, Korea.
- KMID: 2191374
- DOI: http://doi.org/10.3340/jkns.2015.58.3.242
Abstract
OBJECTIVE
The purpose of this study is to determine whether the changes of contralateral sensorimotor cortical activation on functional magnetic resonance imaging (fMRI) can predict the neurological outcome among spinal cord injury (SCI) patients when the great toes are stimulated without notice.
METHODS
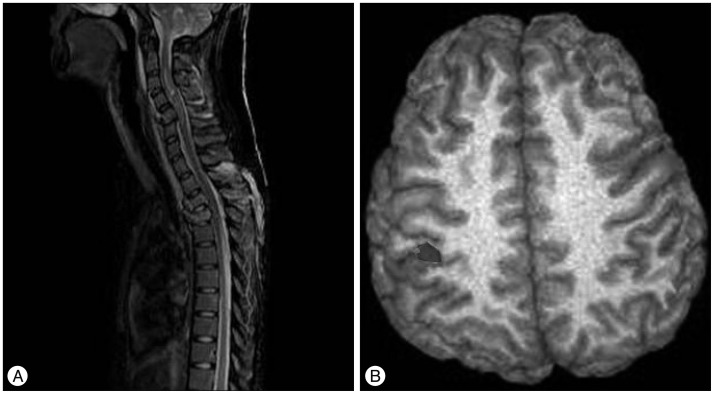
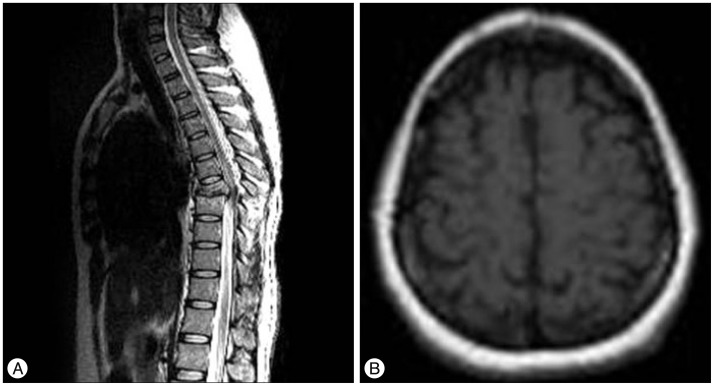
This study enrolled a total of 49 patients with SCI and investigated each patient's preoperative fMRI, postoperative fMRI, American Spinal Injury Association (ASIA) score, and neuropathic pain occurrence. Patients were classified into 3 groups according to the change of blood oxygenation level dependent (BOLD) response on perioperative fMRI during proprioceptive stimulation with repetitive passive toe movements : 1) patients with a response of contralateral sensorimotor cortical activation in fMRI were categorized; 2) patients with a response in other regions; and 3) patients with no response. Correlation between the result of fMRI and each parameter was analyzed.
RESULTS
In fMRI data, ASIA score was likely to show greater improvement in patients in group A compared to those belonging to group B or C (p<0.001). No statistical significance was observed between the result of fMRI and neuropathic pain (p=0.709). However, increase in neuropathic pain in response to the signal change of the ipsilateral frontal lobe on fMRI was statistically significant (p=0.030).
CONCLUSION
When there was change of BOLD response at the contralateral sensorimotor cortex on perioperative fMRI after surgery, relief of neurological symptoms was highly likely for traumatic SCI patients. In addition, development of neuropathic pain was likely to occur when there was change of BOLD response at ipsilateral frontal lobe.
MeSH Terms
Figure
Reference
-
1. Bazley FA, Hu C, Maybhate A, Pourmorteza A, Pashai N, Thakor NV, et al. Electrophysiological evaluation of sensory and motor pathways after incomplete unilateral spinal cord contusion. J Neurosurg Spine. 2012; 16:414–423. PMID: 22303873.
Article2. Curt A, Bruehlmeier M, Leenders KL, Roelcke U, Dietz V. Differential effect of spinal cord injury and functional impairment on human brain activation. J Neurotrauma. 2002; 19:43–51. PMID: 11852977.
Article3. Curt A, Dietz V. Electrophysiological recordings in patients with spinal cord injury : significance for predicting outcome. Spinal Cord. 1999; 37:157–165. PMID: 10213324.
Article4. Duggal N, Rabin D, Bartha R, Barry RL, Gati JS, Kowalczyk I, et al. Brain reorganization in patients with spinal cord compression evaluated using fMRI. Neurology. 2010; 74:1048–1054. PMID: 20200344.
Article5. Freund P, Weiskopf N, Ashburner J, Wolf K, Sutter R, Altmann DR, et al. MRI investigation of the sensorimotor cortex and the corticospinal tract after acute spinal cord injury : a prospective longitudinal study. Lancet Neurol. 2013; 12:873–881. PMID: 23827394.
Article6. Haanpää M, Attal N, Backonja M, Baron R, Bennett M, Bouhassira D, et al. NeuPSIG guidelines on neuropathic pain assessment. Pain. 2011; 152:14–27. PMID: 20851519.
Article7. Henwood P, Ellis JA. Chronic neuropathic pain in spinal cord injury : the patient's perspective. Pain Res Manag. 2004; 9:39–45. PMID: 15007402.
Article8. Jacobs SR, Yeaney NK, Herbison GJ, Ditunno JF Jr. Future ambulation prognosis as predicted by somatosensory evoked potentials in motor complete and incomplete quadriplegia. Arch Phys Med Rehabil. 1995; 76:635–641. PMID: 7605182.
Article9. Jung JK, Oh CH, Yoon SH, Ha Y, Park S, Choi B. Outcome evaluation with signal activation of functional MRI in spinal cord injury. J Korean Neurosurg Soc. 2011; 50:209–215. PMID: 22102951.
Article10. Lotze M, Laubis-Herrmann U, Topka H, Erb M, Grodd W. Reorganization in the primary motor cortex after spinal cord injury - a functional Magnetic Resonance (fMRI) study. Restor Neurol Neurosci. 1999; 14:183–187.11. Masri R, Keller A. Chronic pain following spinal cord injury. Adv Exp Med Biol. 2012; 760:74–88. PMID: 23281514.
Article12. McDonald JW, Becker D, Holekamp TF, Howard M, Liu S, Lu A, et al. Repair of the injured spinal cord and the potential of embryonic stem cell transplantation. J Neurotrauma. 2004; 21:383–393. PMID: 15115588.
Article13. Rocca MA, Agosta F, Martinelli V, Falini A, Comi G, Filippi M. The level of spinal cord involvement influences the pattern of movement-associated cortical recruitment in patients with isolated myelitis. Neuroimage. 2006; 30:879–884. PMID: 16307896.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Traumatic Atypical Tetraplegia Without Radiologic Abnormalities Including Magnetic Resonance Imaging in an Adult: A Case Report
- Effects of Functional Magnetic Stimulation on the Functional Recovery in a Rat Model of Spinal Cord Injury
- Comparative Study of Functional Magnetic Resonance Imaging by Global Scaling Analysis
- Features of the Myelopathy in Patients with Electrical Burn
- Motor Evoked Potentials in Transverse Myelitis