J Korean Med Assoc.
2011 Jun;54(6):594-603. 10.5124/jkma.2011.54.6.594.
Wound coverage using advanced technology in Korea
- Affiliations
-
- 1Department of Plastic Surgery, Korea University College of Medicine, Seoul, Korea. pshan@kumc.or.kr
- KMID: 2190739
- DOI: http://doi.org/10.5124/jkma.2011.54.6.594
Abstract
- The purpose of this article is to outline a variety of wound coverage methods, so that general practitioners can modify their approach to wound healing and possibly incorporate this relevant information into their practice. The article starts with an update on the role of dressing materials in wound healing. It provides a balanced view of what is currently available in Korea. The use of dermal templates has helped in the coverage of wounds that in the past would have required complex surgical solutions. Growth factors and cell therapy provide many of the missing ingredients to jumpstart the wound so that it can go on to heal successfully. The negative pressure therapy, the hydrostatic pressure and/or ultrasonic therapy, and the hyperbaric oxygen therapy also help in healing wounds. Many of these products were introduced recently, and our understanding of how to use them with greater effectiveness has grown. According to the development of bioengineering techniques, advanced dressing materials, growth factors, cell therapy, etc has been introduced for clinical use. Using those materials, the wound coverage can more effective with better results.
Keyword
MeSH Terms
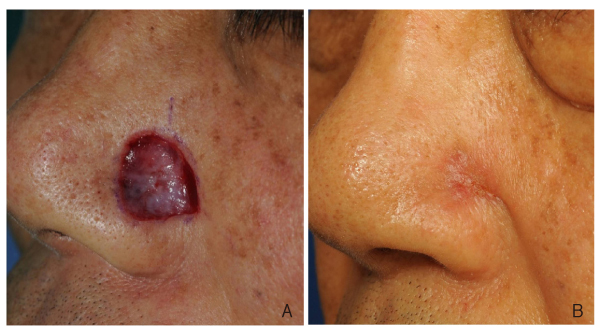
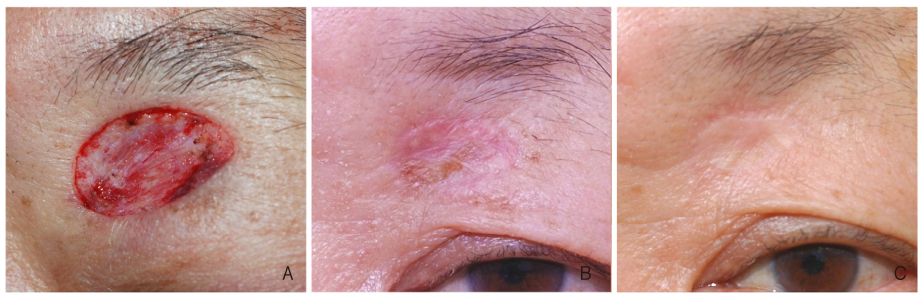
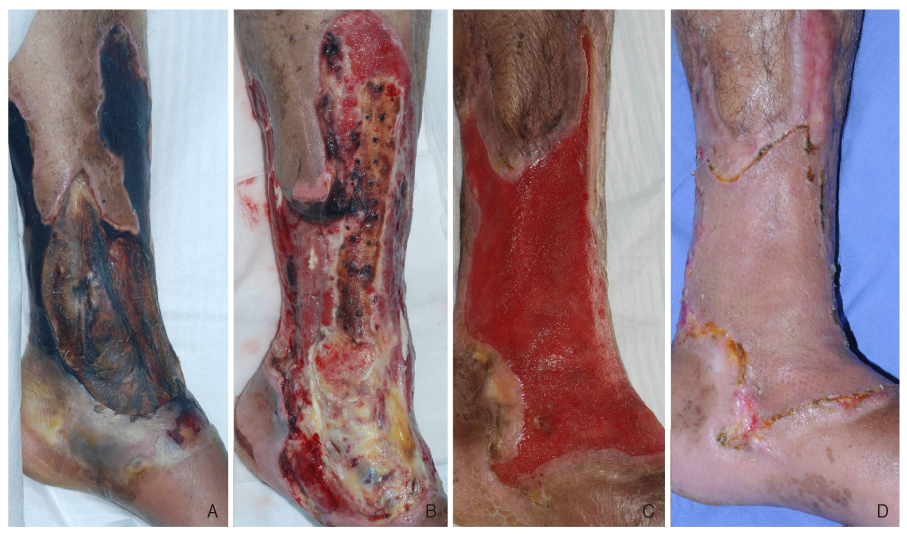
Figure
Cited by 1 articles
-
The Effects of Commodified Growth Factor Products on the Fibrovascularization of Porous Polyethylene Orbital Implants
Won Mo Gu, Joon Hyuk Choi, Jun Hyuk Son
J Korean Ophthalmol Soc. 2014;55(9):1366-1371. doi: 10.3341/jkos.2014.55.9.1366.
Reference
-
1. Han SK. Management of diabetic wound. 2008. Seoul: Kunja;332.2. Han SK, Yoon TH, Kim JB, Kim WK. Dermis graft for wound coverage. Plast Reconstr Surg. 2007. 120:166–172.
Article3. Han SK, Kim JB, Kim WK. Is the dermis graft a reliable and effective option for wound coverage? Reply. Plast Reconstr Surg. 2008. 121:684–685.4. Han SK, Kim HS, Kim WK. Efficacy and safety of fresh fibroblast allografts in the treatment of diabetic foot ulcers. Dermatol Surg. 2009. 35:1342–1348.
Article5. Han SK, Choi KJ, Kim WK. Clinical application of fresh fibroblast allografts for the treatment of diabetic foot ulcers: a pilot study. Plast Reconstr Surg. 2004. 114:1783–1789.
Article6. Eum SJ, Han SK, Gu JH, Jeong SH, Kim WK. Treatment of diabetic ulcer using autologous fibroblast-hyaluronic acid complex. J Korean Soc Plast Reconstr Surg. 2009. 36:548–554.7. Seo DL, Han SK, Chun KW, Kim WK. Clinical application of adipose derived stromal cell autograft for wound coverage. J Korean Soc Plast Reconstr Surg. 2008. 35:653–658.8. Han SK, Kim HR, Kim WK. The treatment of diabetic foot ulcers with uncultured, processed lipoaspirate cells: a pilot study. Wound Repair Regen. 2010. 18:342–348.
Article9. Han SK, Kim DW, Jeong SH, Hong YT, Woo HS, Kim WK, Gottrup F. Potential use of blood bank platelet concentrates to accelerate wound healing of diabetic ulcers. Ann Plast Surg. 2007. 59:532–537.
Article10. Jeong SH, Han SK, Kim WK. Treatment of diabetic foot ulcers using a blood bank platelet concentrate. Plast Reconstr Surg. 2010. 125:944–952.
Article11. Eum SJ, Han SK, Chun KW, Kim WK. Optimal concentration of thrombin to activate platelet for wound healing. J Korean Soc Plast Reconstr Surg. 2009. 36:19–23.12. Kim JB, Chun KW, Han SK, Kim WK. Effect of human bone marrow stromal cell allograft on proliferation and collagen synthesis of diabetic fibroblasts in vitro. J Plast Reconstr Aesthet Surg. 2010. 63:1030–1035.
Article13. Lee CH, Han SK, Choi WI, Kim WK. Effect of human bone marrow stromal cells and dermal fibroblasts on collagen synthesis and epithelization. Ann Plast Surg. 2007. 59:713–719.
Article14. Han SK, Chun KW, Gye MS, Kim WK. The effect of human bone marrow stromal cells and dermal fibroblasts on angiogenesis. Plast Reconstr Surg. 2006. 117:829–835.
Article15. Han SK, Yoon TH, Lee DG, Lee MA, Kim WK. Potential of human bone marrow stromal cells to accelerate wound healing in vitro. Ann Plast Surg. 2005. 55:414–419.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The process by which new health technology is listed for insurance coverage
- Coverage of the Hand and Forearm in Electrical Burn
- Delayed Soft Tissue Coverage after Negative Pressure Wound Therapy in Open Fractures of Lower Extremities
- Coverage of Midline Back Wounds with Perforator-Based Pedicled Fasciocutaneous Flaps
- Improvement Status and Development Direction of New Health Technology Assessment