J Korean Neurosurg Soc.
2012 Oct;52(4):417-419. 10.3340/jkns.2012.52.4.417.
Intradural Extramedullary and Subcutaneous Tumors in Neonate : Atypical Myxoid Spindle Cell Neoplasm
- Affiliations
-
- 1Department of Neurosurgery, College of Medicine, Yeungnam University, Daegu, Korea. shkim@med.yu.ac.kr
- 2Department of Pathology, College of Medicine, Yeungnam University, Daegu, Korea.
- 3Department of Pediatircs, College of Medicine, Yeungnam University, Daegu, Korea.
- KMID: 2190664
- DOI: http://doi.org/10.3340/jkns.2012.52.4.417
Abstract
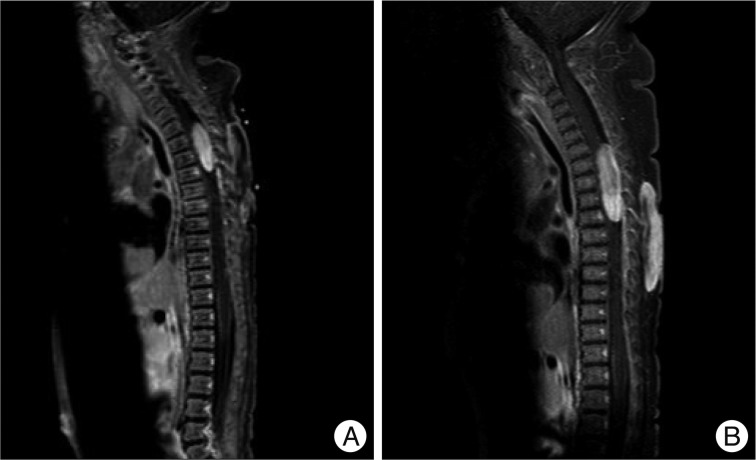
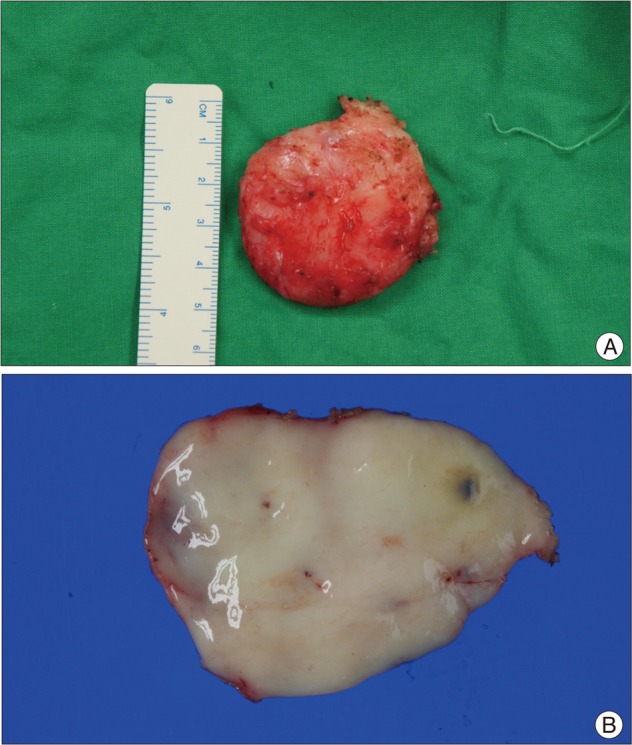
- Tumors of the central nervous system are common in the pediatric population and constitute the second most prevalent tumor type in children. Within this group, spinal cord tumors are relatively rare and account for 1 to 10% of all pediatric central nervous system tumors. We describe a very rare case of an intradural extramedullary spinal cord tumor with a subcutaneous mass and discuss its clinical presentation, pathogenesis, and treatment. A male infant was delivered normally, with uneventful development. At 16 days post-delivery, his family took him to a pediatrician because of a mass on his upper back. Magnetic resonance imaging of the thoracic spine revealed a well-demarcated soft-tissue mass with central cystic change or necrosis at the subcutaneous layer of the posterior back (T2-7 level). Another mass was found with a fat component at the spinal canal of the T1-3 level, which was intradural extramedullary space. After six weeks, the spinal cord tumor and subcutaneous mass were grossly total resected; pathologic findings indicated an atypical myxoid spindle cell neoplasm, possibly nerve sheath in type. The final diagnosis of the mass was an atypical myxoid spindle cell neoplasm. The postoperative course was uneventful, and the patient was discharged after nine days without any neurological deficit. We report a rare case of an intradural extramedullary spinal tumor with subcutaneous mass in a neonate. It is necessary to monitor the patient's status by examining consecutive radiologic images, and the symptoms and neurological changes should be observed strictly during long-term follow-up.
MeSH Terms
Figure
Reference
-
1. Ackerman LL, Menezes AH. Spinal congenital dermal sinuses : a 30-year experience. Pediatrics. 2003; 112:641–647. PMID: 12949296.2. Baysefer A, Akay KM, Izci Y, Kayali H, Timurkaynak E. The clinical and surgical aspects of spinal tumors in children. Pediatr Neurol. 2004; 31:261–266. PMID: 15464638.
Article3. Chadduck WM, Boop FA. Use of full-thickness calvarial bone grafts for cervical spinal fusions in pediatric patients. Pediatr Neurosurg. 1994; 20:107–112. PMID: 8142276.
Article4. Crawford JR, Zaninovic A, Santi M, Rushing EJ, Olsen CH, Keating RF, et al. Primary spinal cord tumors of childhood : effects of clinical presentation, radiographic features, and pathology on survival. J Neurooncol. 2009; 95:259–269. PMID: 19521666.
Article5. Di Lorenzo N, Giuffre R, Fortuna A. Primary spinal neoplasms in childhood : analysis of 1234 published cases (including 56 personal cases) by pathology, sex, age and site. Differences from the situation in adults. Neurochirurgia (Stuttg). 1982; 25:153–164. PMID: 7155253.6. Fassett DR, Clark R, Brockmeyer DL, Schmidt MH. Cervical spine deformity associated with resection of spinal cord tumors. Neurosurg Focus. 2006; 20:E2. PMID: 16512653.
Article7. Gowers WR, Horsley V. A case of tumour of the spinal cord. Removal; recovery. Med Chir Trans. 1888; 71:377–430.11.
Article8. Hardison HH, Packer RJ, Rorke LB, Schut L, Sutton LN, Bruce DA. Outcome of children with primary intramedullary spinal cord tumors. Childs Nerv Syst. 1987; 3:89–92. PMID: 3040249.
Article9. Kumar R, Singh V. Benign intradural extramedullary masses in children of northern India. Pediatr Neurosurg. 2005; 41:22–28. PMID: 15886509.
Article10. Nadkarni TD, Rekate HL. Pediatric intramedullary spinal cord tumors. Critical review of the literature. Childs Nerv Syst. 1999; 15:17–28. PMID: 10066016.11. Prevedello DM, Koerbel A, Tatsui CE, Truite L, Grande CV, Ditzel LF, et al. [Prognostic factors in the treatment of the intradural extramedullary tumors : a study of 44 cases]. Arq Neuropsiquiatr. 2003; 61:241–247. PMID: 12806503.12. Russell DS, Rubinstein LJ. Pathology of tumours of the nervous system. 1989. ed 5. Baltimore: Williams & Wilkins;p. xiiip. 1012–1018.13. Saito T, Yamamuro T, Shikata J, Oka M, Tsutsumi S. Analysis and prevention of spinal column deformity following cervical laminectomy. I. Pathogenetic analysis of postlaminectomy deformities. Spine (Phila Pa 1976). 1991; 16:494–502. PMID: 2052990.
Article14. Shubha AM, Mohanty S, Das K, Garg I. Congenital inclusion tumours in spinal dysraphism. Indian J Pediatr. 2010; 77:167–170. PMID: 20091381.
Article15. Stiller CA, Nectoux J. International incidence of childhood brain and spinal tumours. Int J Epidemiol. 1994; 23:458–464. PMID: 7960369.
Article