J Korean Neurosurg Soc.
2012 Jan;51(1):14-19. 10.3340/jkns.2012.51.1.14.
Direct Pars Repair Surgery Using Two Different Surgical Methods : Pedicle Screw with Universal Hook System and Direct Pars Screw Fixation in Symptomatic Lumbar Spondylosis Patients
- Affiliations
-
- 1Department of Neurosurgery, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. nsdoc35@catholic.ac.kr
- KMID: 2190462
- DOI: http://doi.org/10.3340/jkns.2012.51.1.14
Abstract
OBJECTIVE
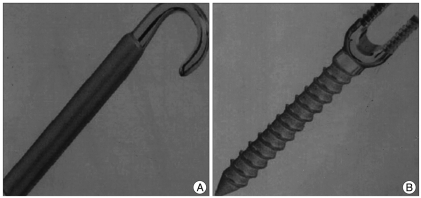
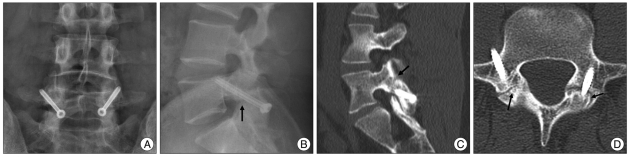
The authors performed a retrospective study to assess the clinical and radiological outcome in symptomatic lumbar spondylolysis patients who underwent a direct pars repair surgery using two different surgical methods; pedicle screw with universal hook system (PSUH) and direct pars screw fixation (DPSF), and compared the results between two different treated groups.
METHODS
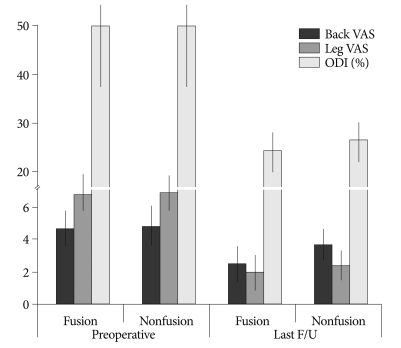
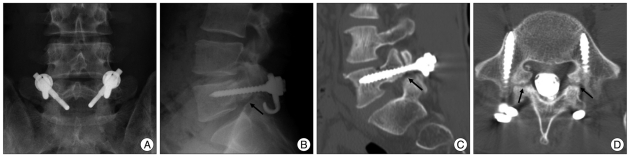
Forty-seven consecutive patients (PSUH; 23, DPSF; 15) with symptomatic lumbar spondylolysis who underwent a direct pars repair surgery were included. The average follow-up period was 37 months in the PSUH group, and 28 months in the DPSF group. The clinical outcome was measured using visual analogue pain scale (VAS) and Oswestry disability index (ODI). The length of operation time, the amount of blood loss, the duration of hospital stay, surgical complications, and fusion status were also assessed.
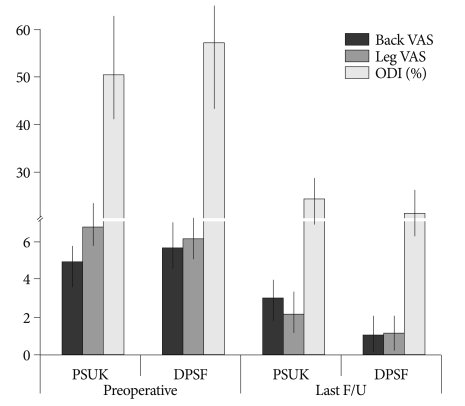
RESULTS
When compared to the DPSF group, the average preoperative VAS and ODI score of the PSUH group were less decreased at the last follow-up; (the PSUH group; back VAS : 4.9 vs. 3.0, leg VAS : 6.8 vs. 2.2, ODI : 50.6% vs. 24.6%, the DPSF group; back VAS : 5.7 vs. 1.1, leg VAS : 6.1 vs. 1.2, ODI : 57.4% vs. 18.2%). The average operation time was 174.9 minutes in the PSUH group, and 141.7 minutes in the DPSF group. The average blood loss during operation was 468.8 cc in the PSUH group, and 298.8 cc in the DPSF group. The average hospital stay after operation was 8.9 days in the PSUH group, and 7 days in the DPSF group. In the PSUH group, there was one case of a screw misplacement requiring revision surgery. In the DPSF group, one patient suffered from transient leg pain. The successful bone fusion rate was 78.3% in the PSUH group, and 93.3% in the DPSF group.
CONCLUSION
The present study suggests that the technique using direct pars screw would be more effective than the method using pedicle screw with lamina hook system, in terms of decreased operation time, amount of blood loss, hospital stay, and increased fusion success rate, as well as better clinical outcome.
MeSH Terms
Figure
Reference
-
1. Askar Z, Wardlaw D, Koti M. Scott wiring for direct repair of lumbar spondylolysis. Spine (Phila Pa 1976). 2003; 28:354–357. PMID: 12590209.
Article2. Beutler WJ, Fredrickson BE, Murtland A, Sweeney CA, Grant WD, Baker D. The natural history of spondylolysis and spondylolisthesis : 45-year follow-up evaluation. Spine (Phila Pa 1976). 2003; 28:1027–1035. discussion 1035. PMID: 12768144.3. Buck JE. Direct repair of the defect in spondylolisthesis. Preliminary report. J Bone Joint Surg Br. 1970; 52:432–437. PMID: 4916960.5. Cheh G, Bridwell KH, Lenke LG, Buchowski JM, Daubs MD, Kim Y, et al. Adjacent segment disease followinglumbar/thoracolumbar fusion with pedicle screw instrumentation : a minimum 5-year follow-up. Spine (Phila Pa 1976). 2007; 32:2253–2257. PMID: 17873819.
Article6. Chung CH, Chiu HM, Wang SJ, Hsu SY, Wei YS. Direct repair of multiple levels lumbar spondylolysis by pedicle screw laminar hook and bone grafting : clinical, CT, and MRI-assessed study. J Spinal Disord Tech. 2007; 20:399–402. PMID: 17607107.
Article7. Dai LY, Jia LS, Yuan W, Ni B, Zhu HB. Direct repair of defect in lumbar spondylolysis and mild isthmic spondylolisthesis by bone grafting, with or without facet joint fusion. Eur Spine J. 2001; 10:78–83. PMID: 11276840.
Article8. Debusscher F, Troussel S. Direct repair of defects in lumbar spondylolysis with a new pedicle screw hook fixation : clinical, functional and Ct-assessed study. Eur Spine J. 2007; 16:1650–1658. PMID: 17520298.
Article9. Fan J, Yu GR, Liu F, Zhao J, Zhao WD. Direct repair of spondylolysis by TSRH's hook plus screw fixation and bone grafting : biomechanical study and clinical report. Arch Orthop Trauma Surg. 2010; 130:209–215. PMID: 19440723.
Article10. Fredrickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am. 1984; 66:699–707. PMID: 6373773.
Article11. Gillet P, Petit M. Direct repair of spondylolysis without spondylolisthesis, using a rod-screw construct and bone grafting of the pars defect. Spine (Phila Pa 1976). 1999; 24:1252–1256. PMID: 10382254.
Article12. Harrop JS, Youssef JA, Maltenfort M, Vorwald P, Jabbour P, Bono CM, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976). 2008; 33:1701–1707. PMID: 18594464.
Article13. Hefti F. [Direct screw repair of spondylolysis with the hooked screw.]. Orthopade. 1997; 26:769–773. PMID: 9432661.14. Ivanic GM, Pink TP, Achatz W, Ward JC, Homann NC, May M. Direct stabilization of lumbar spondylolysis with a hook screw : mean 11-year follow-up period for 113 patients. Spine (Phila Pa 1976). 2003; 28:255–259. PMID: 12567027.15. Jeanneret B. Direct repair of spondylolysis. Acta Orthop Scand Suppl. 1993; 251:111–115. PMID: 8451965.
Article16. Kakiuchi M. Repair of the defect in spondylolysis. Durable fixation with pedicle screws and laminar hooks. J Bone Joint Surg Am. 1997; 79:818–825. PMID: 9199377.
Article17. Kawaguchi Y, Ishihara H, Kanamori M, Yasuda T, Abe Y, Nogami S, et al. Adjacent segment disease following expansive lumbar laminoplasty. Spine J. 2007; 7:273–279. PMID: 17482109.
Article18. Kimura M. [My method of filing the lesion with spongy bone in spondylolysis and spondylolistesis]. Seikei Geka. 1968; 19:285–296. PMID: 5693611.19. Kimura M. [Radiological follow-up of spondylolysis--in 4 cases from the view point of postnatal development]. Seikei Geka. 1971; 22:31–38. PMID: 5105549.20. Klopfenstein JD, Kim LJ, Feiz-Erfan I, Dickman CA. Retroperitoneal approach for lumbar interbody fusion with anterolateral instrumentation for treatment of spondylolisthesis and degenerative foraminal stenosis. Surg Neurol. 2006; 65:111–116. discussion 116. PMID: 16427396.
Article21. Lee CS, Hwang CJ, Lee SW, Ahn YJ, Kim YT, Lee DH, et al. Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J. 2009; 18:1637–1643. PMID: 19533182.
Article22. Levin DA, Hale JJ, Bendo JA. Adjacent segment degeneration following spinal fusion for degenerative disc disease. Bull NYU Hosp Jt Dis. 2007; 65:29–36. PMID: 17539759.23. Mihara H, Onari K, Cheng BC, David SM, Zdeblick TA. The biomechanical effects of spondylolysis and its treatment. Spine (Phila Pa 1976). 2003; 28:235–238. PMID: 12567023.
Article24. Morscher E, Gerber B, Fasel J. Surgical treatment of spondylolisthesis by bone grafting and direct stabilization of spondylolysis by means of a hook screw. Arch Orthop Trauma Surg. 1984; 103:175–178. PMID: 6497607.
Article25. Nicol RO, Scott JH. Lytic spondylolysis. Repair by wiring. Spine (Phila Pa 1976). 1986; 11:1027–1030. PMID: 3554554.26. Noggle JC, Sciubba DM, Samdani AF, Anderson DG, Betz RR, Asghar J. Minimally invasive direct repair of lumbar spondylolysis with a pedicle screw and hook construct. Neurosurg Focus. 2008; 25:E15. PMID: 18673044.
Article27. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion : review of the literature. Spine (Phila Pa 1976). 2004; 29:1938–1944. PMID: 15534420.
Article28. Pavlovcic V. Surgical treatment of spondylolysis and spondylolisthesis with a hook screw. Int Orthop. 1994; 18:6–9. PMID: 8021074.
Article29. Qian Z, Tang T, Yang H. [The direct repair of the defect and grafting with single segment reduction fixation system in the treatment of lumbar spondylolysis and spondylolisthesis]. Zhonghua Wai Ke Za Zhi. 1995; 33:711–714. PMID: 8762547.30. Salib RM, Pettine KA. Modified repair of a defect in spondylolysis or minimal spondylolisthesis by pedicle screw, segmental wire fixation, and bone grafting. Spine (Phila Pa 1976). 1993; 18:440–443. PMID: 8470004.
Article31. Schlenzka D, Remes V, Helenius I, Lamberg T, Tervahartiala P, Yrjönen T, et al. Direct repair for treatment of symptomatic spondylolysis and low-grade isthmic spondylolisthesis in young patients : no benefit in comparison to segmental fusion after a mean follow-up of 14.8 years. Eur Spine J. 2006; 15:1437–1447. PMID: 16463195.
Article32. Schlenzka D, Seitsalo S, Poussa M, Osterman K. Operative treatment of symptomatic lumbar spondylolysis and mild isthmic spondylolisthesis in young patients : direct repair of the defect or segmental spinal fusion? Eur Spine J. 1993; 2:104–112. PMID: 20058460.
Article33. Shim JH, Kim WS, Kim JH, Kim DH, Hwang JH, Park CK. Comparison of instrumented posterolateral fusion versus percutaneous pedicle screw fixation combined with anterior lumbar interbody fusion in elderly patients with L5-S1 isthmic spondylolisthesis and foraminal stenosis. J Neurosurg Spine. 2011; 15:311–319. PMID: 21599444.
Article34. Sys J, Michielsen J, Bracke P, Martens M, Verstreken J. Nonoperative treatment of active spondylolysis in elite athletes with normal X-ray findings : literature review and results of conservative treatment. Eur Spine J. 2001; 10:498–504. PMID: 11806390.
Article35. Ulibarri JA, Anderson PA, Escarcega T, Mann D, Noonan KJ. Biomechanical and clinical evaluation of a novel technique for surgical repair of spondylolysis in adolescents. Spine (Phila Pa 1976). 2006; 31:2067–2072. PMID: 16915090.
Article36. Winter RB. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am. 1985; 67:823. PMID: 3997936.
Article37. Zhao J, Liu F, Shi HG, Fan J, Zhao WD, Wang YH, et al. Biomechanical and clinical study on screw hook fixation after direct repair of lumbar spondylolysis. Chin J Traumatol. 2006; 9:288–292. PMID: 17026861.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Direct Repair of Pars Defects in Symptomatic Lumbar Spondylolysis Using Pedicle Screws and Universal Hooks : Preliminary Report
- Direct Repair of the Pars Interarticularis Defect in Lumbar Spondylolysis
- Biomechanical Evaluation of Supplemental Hook or Screw Fixation in Short Segment Spinal Instrumentation
- Morphometric Study of the Pedicle of Lumbar and Selected Thoracic Vertebrae for Surgical Spinal Fixation
- Atlantoaxial Stabilization Using C1 Lateral Mass and C2 Pedicle/Translaminar Screw Fixation by Intraoperative C1- and C2-Direct-Captured Navigation with Preoperative Computed Tomography Images