Observed Trends for an Earlier Onset of Puberty: When is the Need for Treatment Indicated?
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Korea. chshinpd@snu.ac.kr
- 2Department of Pediatrics, Boramae Medical Center, Korea.
- KMID: 2188132
- DOI: http://doi.org/10.5124/jkma.2009.52.12.1189
Abstract
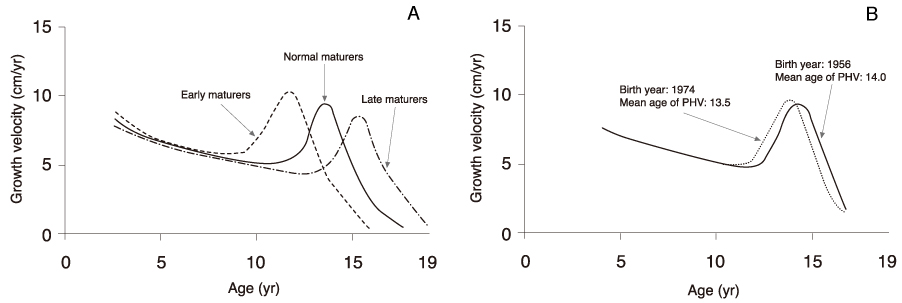
- Globally, there is a secular trend toward earlier puberty and an increased final height at adulthood. In Korea, there is a trend toward an earlier menarche in girls but insufficient data to evaluate secular trends in boys. A significant increase in height was observed in Koreans aged 0~20 years during 1965~2005. This trend has diminished, but growth maturation has accelerated in infants and young children. Genetic and environmental factors including nutritional status (e.g., obesity) contribute to these changes. Central precocious puberty results from the accelerated activation of the hypothalamic-pituitary-gonadal axis. Although the cut-off age is controversial, clinical evaluations should be conducted on girls with pubertal onset occurring younger than 8 years, and on boys younger than 9 years at least until further prospective studies define the norms for Korea. Management of precocious puberty depends on the underlying etiology, as accelerated puberty can lead to a reduced final adult height. Depot forms of GnRH agonists (GnRHas) are the standard treatment for some patients with central precocious puberty. These agents can help restore the normal adult height in both girls and boys when it might be compromised by rapidly progressive precocious puberty. However, in girls with slowly progressive precocious puberty or with the onset of puberty at 8~9.9 years of age (early normal puberty), GnRHa treatment might offer no benefit for attaining normal height. There is little evidence on whether psychosocial problems are associated with precocious puberty or are improved by GnRHa treatment.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Adult height in girls with central precocious puberty without gonadotropin-releasing hormone agonist treatment: a retrospective case-control study
Hyun Ji Jang, Min Jung Kwak, Young Mi Kim, Soo-Han Choi, Kyung Hee Park, Hye Won Yoo, Su Jeong Park, Yoon Hee Jo, Ha Young Jo
J Yeungnam Med Sci. 2023;40(Suppl):S81-S86. doi: 10.12701/jyms.2023.00801.Depression and self-concept in girls with perception of pubertal onset
Ji Hyeon Yang, Sang Woo Han, Chan Woo Yeom, Yong Jun Park, Wha Su Choi, Ji Young Seo, Young Jin Koo
Ann Pediatr Endocrinol Metab. 2013;18(3):135-140. doi: 10.6065/apem.2013.18.3.135.Effects of gonadotropin-releasing hormone agonist treatment on final adult height in boys with idiopathic central precocious puberty
Ah Young Cho, Su Yeong Ko, Jae Hee Lee, Eun Young Kim
Ann Pediatr Endocrinol Metab. 2021;26(4):259-265. doi: 10.6065/apem.2040268.134.
Reference
-
1. Parent AS, Teilmann G, Juul A, Skakkebaek NE, Toppari J, Bourguignon JP. The timing of normal puberty and the age limits of sexual precocity: variations around the world, secular trends, and changes after migration. Endocr Rev. 2003. 24:668–693.
Article2. Karlberg J. Secular trends in pubertal development. Horm Res. 2002. 57:Suppl 2. 19–30.
Article3. Herman-Giddens ME, Slora EJ, Wasserman RC, Bourdony CJ, Bhapkar MV, Koch GG, Hasemeier CM. Secondary sexual characteristics and menses in young girls seen in office practice: a study from the Pediatric Research in Office Settings network. Pediatrics. 1997. 99:505–512.
Article4. Kaplowitz PB, Oberfield SE. Drug and Therapeutics and Executive Committees of the Lawson Wilkins Pediatric Endocrine Society. Reexamination of the age limit for defining when puberty is precocious in girls in the United States: implications for evaluation and treatment. Pediatrics. 1999. 104:936–941.
Article5. Midyett LK, Moore WV, Jacobson JD. Are pubertal changes in girls before age 8 benign? Pediatrics. 2003. 111:47–51.
Article6. Mul D, Hughes IA. The use of GnRH agonists in precocious puberty. Eur J Endocrinol. 2008. 159:Suppl 1. 3–8.
Article7. Suh BK. Endocrine diseases in adolescence. J Korean Med Assoc. 2009. 52:758–767.
Article8. De Sanctis V, Corrias A, Rizzo V, Bertelloni S, Urso L, Galluzzi F, Pasquino AM, Pozzan G, Guarneri MP, Cisternino M, De Luca F, Gargantini L, Pilotta A, Sposito M, Tonini G. Etiology of central precocious puberty in males: the results of the Italian Study Group for Physiopathology of Puberty. J Pediatr Endocrinol Metab. 2000. 13:Suppl 1. 687–693.
Article9. Chalumeau M, Chemaitilly W, Trivin C, Adan L, Bréart G, Brauner R. Central precocious puberty in girls: an evidence-based diagnosis tree to predict central nervous system abnormalities. Pediatrics. 2002. 109:61–67.
Article10. Carel JC, Léger J. Clinical practice. Precocious puberty. N Engl J Med. 2008. 358:2366–2377.11. Neely EK, Wilson DM, Lee PA, Stene M, Hintz RL. Spontaneous serum gonadotropin concentrations in the evaluation of precocious puberty. J Pediatr. 1995. 127:47–52.
Article12. Teilmann G, Pedersen CB, Jensen TK, Skakkebaek NE, Juul A. Prevalence and incidence of precocious pubertal development in Denmark: an epidemiologic study based on national registries. Pediatrics. 2005. 116:1323–1328.
Article13. Na JM, Lee YJ, Kim MS, Lee DY, Yeo CY, Kim CJ, Kim JD, Kim EY. Causes of precocious puberty: multicenter study in honam area. J Korean Soc Pediatr Endocrinol. 2009. 14:30–37.14. Kim TH, Coe HJ, Kim S, Lee SW, Chae HW, Kim YS, Park MJ, Chung SC, Yu EK, Kim DH, Kim HS. Clinical and endocrinologic characteristics of children referred for precocious puberty. J Korean Soc Pediatr Endocrinol. 2007. 12:119–126.15. Aksglaede L, Sørensen K, Petersen JH, Skakkebaek NE, Juul A. Recent decline in age at breast development: the Copenhagen Puberty Study. Pediatrics. 2009. 123:e932–e939.
Article16. Euling SY, Herman-Giddens ME, Lee PA, Selevan SG, Juul A, Sørensen TI, Dunkel L, Himes JH, Teilmann G, Swan SH. Examination of US puberty-timing data from 1940 to 1994 for secular trends: panel findings. Pediatrics. 2008. 121:Suppl 3. 172–191.
Article17. de Muinich Keizer SM, Mul D. Trends in pubertal development in Europe. Hum Reprod Update. 2001. 7:287–291.
Article18. Hong CH, Rho HO, Song SH. The sexual maturity rating of adolescent boys and girls in Korea. J Korean Pediatr Soc. 1994. 37:193–198.19. Kim HS, Kim JY, Shin YK, Park SH, Tockgo YC. A Study on menarchel age and monthly incidence of school girls in Ansan. J Korean Pediatr Soc. 1997. 40:458–463.20. Park MJ, Lee IS, Shin EK, Joung H, Cho SI. The timing of sexual maturation and secular trends of menarchial age in Korean adolescents. Korean J Pediatr. 2006. 49:610–616.
Article21. The Third Korea National Health and Nutrition Examination Survey (KNHANES III). Available form http://knhanes.cdc.go.kr/.22. Frisch RE, Revelle R, Cook S. Components of weight at menarche and the initiation of the adolescent growth spurt in girls: estimated total water, lean body weight and fat. Hum Biol. 1973. 45:469–483.23. Kaplowitz PB, Slora EJ, Wasserman RC, Pedlow SE, Herman-Giddens ME. Earlier onset of puberty in girls: relation to increased body mass index and race. Pediatrics. 2001. 108:347–353.
Article24. He Q, Karlberg J. BMI in childhood and its association with height gain, timing of puberty, and final height. Pediatr Res. 2001. 49:244–251.
Article25. Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, Hauser R, Prins GS, Soto AM, Zoeller RT, Gore AC. Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocr Rev. 2009. 30:293–342.
Article26. Luo ZC, Cheung YB, He Q, Albertsson-Wikland K, Karlberg J. Growth in early life and its relation to pubertal growth. Epidemiology. 2003. 14:65–73.
Article27. Cooper C, Kuh D, Egger P, Wadsworth M, Barker D. Childhood growth and age at menarche. Br J Obstet Gynaecol. 1996. 103:814–817.
Article28. Ibáñez L, Ferrer A, Marcos MV, Hierro FR, de Zegher F. Early puberty: rapid progression and reduced final height in girls with low birth weight. Pediatrics. 2000. 106:e72.29. Lienhardt A, Carel JC, Preux PM, Coutant R, Chaussain JL. Amplitude of pubertal growth in short stature children with intrauterine growth retardation. Horm Res. 2002. 57:Suppl 2. 88–94.
Article30. Ibáñez L, Potau N, Francois I, de Zegher F. Precocious pubarche, hyperinsulinism, and ovarian hyperandrogenism in girls: relation to reduced fetal growth. J Clin Endocrinol Metab. 1998. 83:3558–3562.
Article31. Hernández MI, Mericq V. Impact of being born small for gestational age on onset and progression of puberty. Best Pract Res Clin Endocrinol Metab. 2008. 22:463–476.
Article32. Nield LS, Cakan N, Kamat D. A practical approach to precocious puberty. Clin Pediatr (Phila). 2007. 46:299–306.
Article33. Gohlke B, Woelfle J. Growth and puberty in German children: is there still a positive secular trend? Dtsch Arztebl Int. 2009. 106:377–382.34. Kim JY, Oh IH, Lee EY, Choi KS, Choe BK, Yoon TY, Lee CG, Moon JS, Shin SH, Choi JM. Anthropometric changes in children and adolescents from 1965 to 2005 in Korea. Am J Phys Anthropol. 2008. 136:230–236.
Article35. Cole TJ. Secular trends in growth. Proc Nutr Soc. 2000. 59:317–324.
Article36. Tanner JM, Davies PS. Clinical longitudinal standards for height and height velocity for North American children. J Pediatr. 1985. 107:317–329.
Article37. Carel JC, Lahlou N, Roger M, Chaussain JL. Precocious puberty and statural growth. Hum Reprod Update. 2004. 10:135–147.
Article38. Kauli R, Galatzer A, Kornreich L, Lazar L, Pertzelan A, Laron Z. Final height of girls with central precocious puberty, untreated versus treated with cyproterone acetate or GnRH analogue. A comparative study with re-evaluation of predictions by the Bayley-Pinneau method. Horm Res. 1997. 47:54–61.
Article39. Palmert MR, Malin HV, Boepple PA. Unsustained or slowly progressive puberty in young girls: initial presentation and long-term follow-up of 20 untreated patients. J Clin Endocrinol Metab. 1999. 84:415–423.
Article40. Léger J, Reynaud R, Czernichow P. Do all girls with apparent idiopathic precocious puberty require gonadotropin-releasing hormone agonist treatment? J Pediatr. 2000. 137:819–825.
Article41. Lazar L, Kauli R, Pertzelan A, Phillip M. Gonadotropin-suppressive therapy in girls with early and fast puberty affects the pace of puberty but not total pubertal growth or final height. J Clin Endocrinol Metab. 2002. 87:2090–2094.
Article42. Ritzén EM. Early puberty: what is normal and when is treatment indicated? Horm Res. 2003. 60:Suppl 3. 31–34.
Article43. Xhrouet-Heinrichs D, Lagrou K, Heinrichs C, Craen M, Dooms L, Malvaux P, Kanen F, Bourguignon JP. Longitudinal study of behavioral and affective patterns in girls with central precocious puberty during long-acting triptorelin therapy. Acta Paediatr. 1997. 86:808–815.
Article44. Johansson T, Ritzén EM. Very long-term follow-up of girls with early and late menarche. Endocr Dev. 2005. 8:126–136.
Article45. Tremblay L, Frigon JY. The interaction role of obesity and pubertal timing on the psychosocial adjustment of adolescent girls: longitudinal data. Int J Obes (Lond). 2005. 29:1204–1211.
Article46. Tremblay L, Frigon JY. Precocious puberty in adolescent girls: a biomarker of later psychosocial adjustment problems. Child Psychiatry Hum Dev. 2005. 36:73–94.
Article47. Bar A, Linder B, Sobel EH, Saenger P, DiMartino-Nardi J. Bayley-Pinneau method of height prediction in girls with central precocious puberty: correlation with adult height. J Pediatr. 1995. 126:955–958.
Article48. Carel JC, Roger M, Ispas S, Tondu F, Lahlou N, Blumberg J, Chaussain JL. French study group of Decapeptyl in Precocious Puberty. Final height after long-term treatment with triptorelin slow release for central precocious puberty: importance of statural growth after interruption of treatment. J Clin Endocrinol Metab. 1999. 84:1973–1978.
Article49. Arrigo T, Cisternino M, Galluzzi F, Bertelloni S, Pasquino AM, Antoniazzi F, Borrelli P, Crisafulli G, Wasniewska M, De Luca F. Analysis of the factors affecting auxological response to GnRH agonist treatment and final height outcome in girls with idiopathic central precocious puberty. Eur J Endocrinol. 1999. 141:140–144.
Article50. Klein KO, Barnes KM, Jones JV, Feuillan PP, Cutler GB Jr. Increased final height in precocious puberty after long-term treatment with LHRH agonists: the National Institutes of Health experience. J Clin Endocrinol Metab. 2001. 86:4711–4716.
Article51. Ahn SY, Yoo JH, Shin CH, Yang SW. The effects of gonadotropin-releasing hormone agonists on final height and its related factors in patients with true precocious puberty. Korean J Pediatr. 2004. 47:647–655.52. Mul D, Oostdijk W, Otten BJ, Rouwé C, Jansen M, Dele-marre-van de Waal HA, Waelkens JJ, Drop SL. Final height after gonadotrophin releasing hormone agonist treatment for central precocious puberty: the Dutch experience. J Pediatr Endocrinol Metab. 2000. 13:Suppl 1. 765–772.
Article53. Massart F, Federico G, Harrell JC, Saggese G. Growth outcome during GnRH agonist treatments for slowly progressive central precocious puberty. Neuroendocrinology. 2009. 90:307–314.
Article54. Bouvattier C, Coste J, Rodrigue D, Teinturier C, Carel JC, Chaussain JL, Bougnéres PF. Lack of effect of GnRH agonists on final height in girls with advanced puberty: a randomized long-term pilot study. J Clin Endocrinol Metab. 1999. 84:3575–3578.
Article55. Carel JC, Eugster EA, Rogol A, Ghizzoni L, Palmert MR, Antoniazzi F, Berenbaum S, Bourguignon JP, Chrousos GP, Coste J, Deal S, de Vries L, Foster C, Heger S, Holland J, Jahnukainen K, Juul A, Kaplowitz P, Lahlou N, Lee MM, Lee P, Merke DP, Neely EK, Oostdijk W, Phillip M, Rosenfield RL, Shulman D, Styne D, Tauber M, Wit JM. ESPELWPES GnRH Analogs Consensus Conference Group. Consensus statement on the use of gonadotropin-releasing hormone analogs in children. Pediatrics. 2009. 123:e752–e762.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Childhood Obesity and Pubertal Development
- Etiology and treatment of central precocious puberty
- Diagnosis and Treatment of Central Precocious Puberty
- Etiological trends in male central precocious puberty
- Genetic and epigenetic aspects of the KISS1 and KISS1R genes in pubertal development and central precocious puberty: A review