J Korean Orthop Assoc.
2009 Feb;44(1):76-82. 10.4055/jkoa.2009.44.1.76.
Minimal Invasive Unilateral Transforaminal Lumbar Interbody Fusion by Sublaminar Decompression: Comparison to Bilateral Approach
- Affiliations
-
- 1Department of Orthopeadic Surgery, Dankook University College of Medicine, Cheonan, Korea. osmin71@naver.com
- KMID: 2186381
- DOI: http://doi.org/10.4055/jkoa.2009.44.1.76
Abstract
-
PURPOSE: This is a comparison of the unilateral and bilateral approaches for minimal invasive transforaminal lumbar interbody fusion (TLIF), and we did so by measuring the clinical and radiological results.
MATERIALS AND METHODS
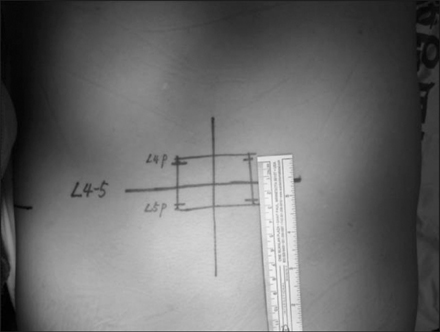
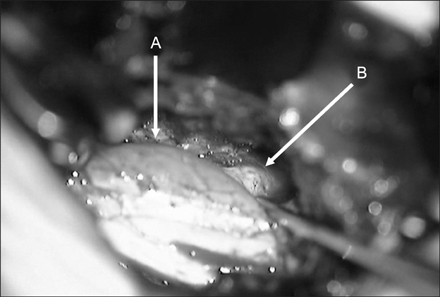
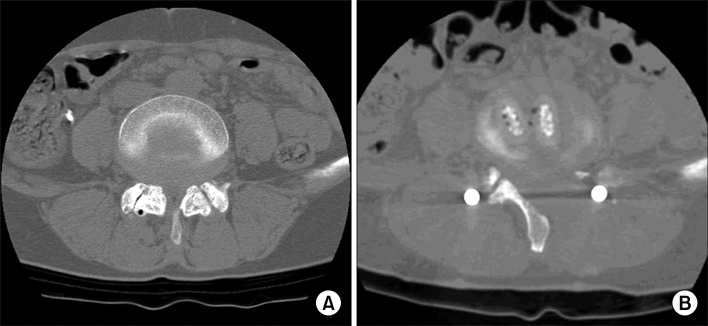
This study examined a consecutive series of 47 patients who underwent one-level TLIF (26 cases of the unilateral approach and 21 cases of the bilateral approach to the lumbar spine) and the follow-up data was compared with a minimum 1-year follow-up. Sublaminar decompression and contralateral foraminectomy were done in all the case of using the unilateral approach. The age of each patient, the amount of intraoperative blood loss, the postoperative drainage, the transfusion requirement and the surgery time were investigated. The clinical outcomes were analyzed using the visual analogue scale, the SF-36 Physical Composite Score (PCS) and the Oswestry disability index (ODI). The preoperative, postoperative & last follow-up changes in the height and angles of the disc in the fused segments and the lumbar lordotic angles were radiologically analyzed.
RESULTS
There was no statistical difference between the two groups in terms of the clinical and radiographic results at the last follow-up. But the unilateral approach-group was found to have a less blood loss, less postoperative drainage, a lesser requirement for transfusion and a shorter surgery time.
CONCLUSION
This study confirms that the unilateral approach can be the better way if the technical problems are solved.
MeSH Terms
Figure
Reference
-
1. Gejo R, Matsui H, Kawaguchi Y, Ishihara H, Tsuji H. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine. 1999. 24:1023–1028.
Article2. Guiot BH, Khoo LT, Fessler RG. A minimally invasive technique for decompression of the lumbar spine. Spine. 2002. 27:432–438.
Article3. Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine: preliminary clinical results. J Neurosurg. 2002. 97:Suppl 1. S7–S12.
Article4. Foley KT, Lefkowitz MA. Advances in minimally invasive spine surgery. Clin Neurosurg. 2002. 49:499–517.5. Foley KT, Smith MM, Rampersaud YR. Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg Focus. 1999. 7(5):e5.
Article6. Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine. 2003. 28:Suppl 15. S26–S35.
Article7. Glassman S, Gornet MF, Branch C, et al. MOS short form 36 and oswestry disability index outcomes in lumbar fusion: a multicenter experience. Spine J. 2006. 6:21–26.
Article8. Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. A histologic and enzymatic analysis. Spine. 1996. 21:941–944.9. Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. Part 2: histologic and histochemical analyses in humans. Spine. 1994. 19:2598–2602.10. Khoo LT, Palmer S, Laich DT, Fesseler RG. Minimally invasive percutaneous posterior lumbar interbody fusion. Neurosurgery. 2002. 51:Suppl 1. S166–S181.
Article11. Lee SH, Kim DJ, Oh JH, Han HS, Lee HK, Kim HS. Evaluation of functional outcomes and quality of life assessments in patients with malignant tumors of the musculoskeletal system. J Korean Orthop Assoc. 2001. 36:107–114.
Article12. Mayer TG, Vanharanta H, Gatchel RJ, et al. Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine. 1989. 14:33–36.
Article13. Park Y, Ha JW, Sung SY, Oh HC, Yoo JH, Lee YT. Minimally invasive posterior lumbar interbody fusion: comparison with traditional open surgery. J Korean Orthop Assoc. 2006. 41:288–296.
Article14. Rantanen J, Hurme M, Falck B, et al. The lumbar multifidus muscle five years after surgery for a lumbar intervertebral disc herniation. Spine. 1993. 18:568–574.
Article15. Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion TLIF technical feasibility and initial results. J Spinal Disord Tech. 2005. 18:Suppl 1. S1–S6.16. Sihvonen T, Herno A, Paljärvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine. 1993. 18:575–581.
Article17. Slover J, Abdu WA, Hanscom B, Weinstein JN. The impact of comorbidities on the change in short-form 36 and oswestry scores following lumbar spine surgery. Spine. 2006. 31:1974–1980.
Article18. Styf JR, Willén J. The effects of external compression by three different retractors on pressure in the erector spine muscles during and after posterior lumbar spine surgery in humans. Spine. 1998. 23:354–358.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mini-invasive unilateral transforaminal lumbar interbody fusion and pedicle screw fixation
- Biportal Endoscopic Transforaminal Lumbar Interbody Fusion with Percutaneous Instrumentation: A Technical Note
- Minimally Invasive Strategy for Uniportal Full-Endoscopic Transforaminal Lumbar Interbody Fusion Using a Large Cage Utilized in Oblique Lumbar Interbody Fusion
- Can Unilateral Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF) Result in Sufficient Reduction in Spondylolisthesis?: A Comparison with Open TLIF and Bilateral MIS TLIF
- Minimally Invasive Transforaminal Lumbar Interbody Fusion in Patients with Low Grade Spondylolisthesis: Comparison of the Unilateral and Bilateral Approaches