J Korean Orthop Assoc.
2009 Aug;44(4):429-435.
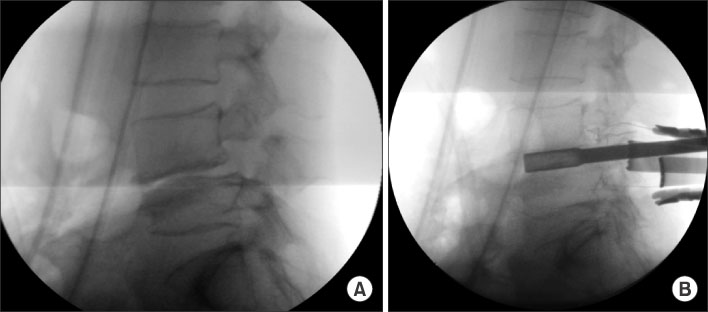
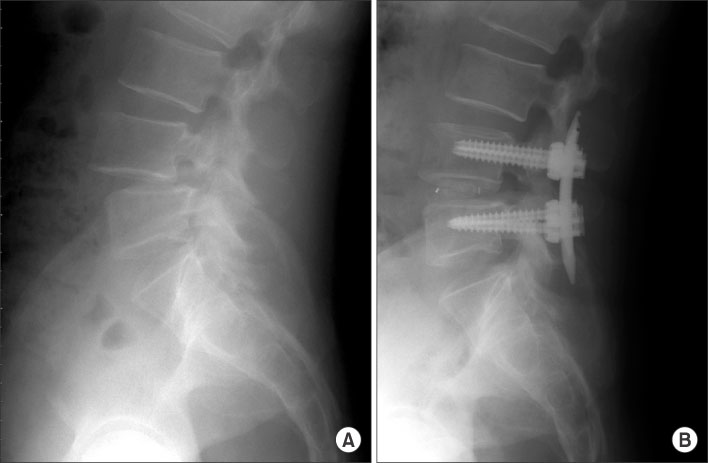
Minimally Invasive Transforaminal Lumbar Interbody Fusion in Patients with Low Grade Spondylolisthesis: Comparison of the Unilateral and Bilateral Approaches
- Affiliations
-
- 1Department of Orthopaedic Surgery, Dankook University College of Medicine, Cheonan, Korea. osmin71@naver.com
Abstract
- PURPOSE
We wanted to analyze the clinical and radiological results of minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) in patients with low grade spondylolisthesis, and we also compared the unilateral and bilateral approaches. MATERIALS AND METHODS: This study examined a consecutive series of 27 patients who underwent one-level MI-TLIF (16 cases of the unilateral approach and 11 cases of the bilateral approach) and the follow-up data was compared with a minimum 1-year follow-up. The amount of intraoperative blood loss, the postoperative drainage, the transfusion requirement and the surgery time were investigated. The clinical outcomes were analyzed using the visual analogue scale (VAS), the Oswestry disability index (ODI) and the SF-36 Physical Composite Score (SF-36). The preoperative, postoperative and last follow-up changes in the height of the disc, the degree of the slipping and the slip angle in the fused segments were radiologically analyzed. RESULTS: There were no significant differences between the two groups in terms of the clinical and radiological results at the last follow-up. But the unilateral approach-group was found to have less blood loss, less postoperative drainage, a lesser requirement for transfusion and a shorter duration of surgery. During the reduction process in 1 patient among the cases that had the unilateral approach used, the pedicle screw fixed to the vertebral body fell out. CONCLUSION: The unilateral MI-TLIF can shorten the operation time and reduce the blood loss as compared to the bilateral approa
Keyword
Figure
Reference
-
1. Kaneda K, Kazama H, Satoh S, Fujiya M. Follow-up study of medial facetectomies and posterolateral fusion with instrumentation in unstable degenerative spondylolisthesis. Clin Orthop Relat Res. 1986. 203:159–167.
Article2. Kim NH, Lee JW. Anterior interbody fusion versus posterolateral fusion with transpedicular fixation for isthmic spondylolisthesis in adults. A comparison of clinical results. Spine. 1999. 24:812–816.3. Cloward RB. Spondylolisthesis: treatment by laminectomy and posterior interbody fusion. Clin Orthop Relat Res. 1981. 154:74–82.4. Lin PM. Posterior lumbar interbody fusion technique: complications and pitfalls. Clin Orthop Relat Res. 1985. 193:90–102.5. Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine. 1997. 22:210–219.
Article6. Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine. 2003. 28:Suppl. 26–35.
Article7. Schwender J, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech. 2005. 18:Suppl. 1–6.8. Isaacs RE, Podichetty VK, Santiago P, et al. Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine. 2005. 3:98–105.
Article9. Min SH, Hwang SS. Minimal invasive unilateral transforaminal lumbar interbody fusion by sublaminar decompression -comparison to bilateral approach-. J Korean Orthop Assoc. 2009. 44:76–82.10. Wu CH, Kao YH, Yang SC, Fu TS, Lai PL, Chen WJ. Supplementary pedicle screw fixation in spinal fusion for degenerative spondylolisthesis in patients aged 65 and over: outcome after a minimum of 2 years follow-up in 82 patients. Acta Orthop. 2008. 79:67–73.
Article11. Sears W. Posterior lumbar interbody fusion for degenerative spondylolisthesis: restoration of sagittal balance using insert-and-rotate interbody spacers. Spine J. 2005. 5:170–179.
Article12. Park P, Foley KT. Minimally invasive transforaminal lumbar interbody fusion with reduction of spondylolisthesis: technique and outcomes after a minimum of 2 years' follow-up. Neurosurg Focus. 2008. 25:E16.
Article13. Yan DL, Pei FX, Li J, Soo CL. Comparative study of PLIF and TLIF treatment in adult degenerative spondylolisthesis. Eur Spine J. 2008. 17:1311–1316.14. Cho KJ, Moon KH, Lee DJ, Lee KY, Kim KH, Park SR. Factors affecting reduction of slippage in posterolateral fusion for spondylolytic spondylolisthesis. J Kor Soc Spine Surg. 2006. 13:177–183.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Can Unilateral Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF) Result in Sufficient Reduction in Spondylolisthesis?: A Comparison with Open TLIF and Bilateral MIS TLIF
- The Result of Minimally Invasive Transforaminal Lumbar Interbody Fusion in Low Grade Spondylolisthesis - Minimum 2 Years Follow Up -
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- Mini-invasive unilateral transforaminal lumbar interbody fusion and pedicle screw fixation
- Surgical Outcomes of Minimally Invasive Transforaminal Lumbar Interbody Fusion for the Treatment of Spondylolisthesis and Degenerative Segmental Instability