J Korean Orthop Assoc.
2010 Dec;45(6):440-447. 10.4055/jkoa.2010.45.6.440.
Analysis of Treatment Outcomes for Open Fractures of the Tibia in Children
- Affiliations
-
- 1Department of Orthopedic Surgery, Chonbuk National University, Medical School Research Institute of Clinical Science, Korea. jrkeem@chonbuk.ac.kr
- 2Department of Orthopaedic Surgery, Jeju National University College of Medicine, Jeju, Korea.
- KMID: 2185491
- DOI: http://doi.org/10.4055/jkoa.2010.45.6.440
Abstract
- PURPOSE
Our objective was to analyze outcomes of treatment for open fractures of the tibia in children according to the classification of Gustilo-Anderson type.
MATERIALS AND METHODS
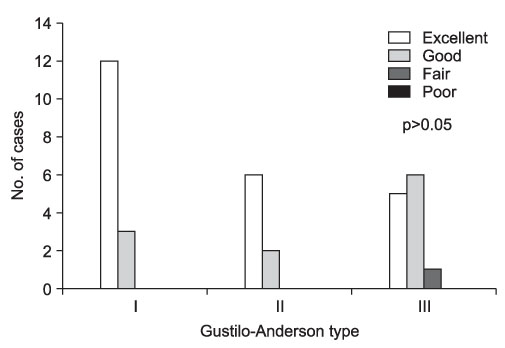
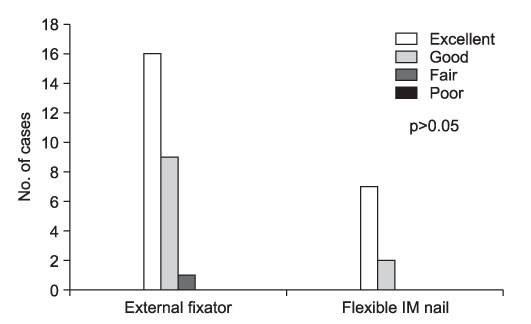
We reviewed thirty five pediatric patients who underwent surgery for open fractures of the tibia between June 1998 and June 2007. We followed up over more than 1 year. Fractures were grouped into three types according to Gustilo-Anderson classification (Types I, II, and III). External fixation or flexible intramedullary nailing was used as the surgical method. We analyzed the period required to achieve radiologic bony union, tibial alignment, leg length discrepancy and complications. Clinical outcomes were assessed using the Karlstrom-Olerud method.
RESULTS
Radiologically, bony union was achieved in 11.35+/-3.08 weeks, 10.50+/-2.20 weeks, and 21.62+/-7.19 weeks for types I, II, and III, respectively. Delayed union occurred in one case of type II and 3 cases of type III fractures. Complications such as nonunion, malunion and osteomyelitis were seen only in type III. Clinical outcomes showed excellent or good results in all cases except one (type III).
CONCLUSION
Excellent outcomes for open fractures of the tibia in children can be obtained regardless of Gustilo-Anderson type when adequate procedures are performed.
Keyword
Figure
Reference
-
1. Court-Brown C. Bucholz R, Heckman J, Court-Brown C, editors. Rockwood and Green's fractures in adults. 2006. 6th ed. Philadelphia: Lippincott Williams & Wilkins;2080–2146.2. Bartlett CS 3rd, Weiner LS, Yang EC. Treatment of type II and type III open tibia fractures in children. J Orthop Trauma. 1997. 11:357–362.
Article3. Buckley SL, Smith G, Sponseller PD, Thompson JD, Griffin PP. Open fractures of the tibia in children. J Bone Joint Surg Am. 1990. 72:1462–1469.
Article4. Cullen MC, Roy DR, Crawford AH, Assenmacher J, Levy MS, Wen D. Open fracture of the tibia in children. J Bone Joint Surg Am. 1996. 78:1039–1047.
Article5. Hope PG, Cole WG. Open fractures of the tibia in children. J Bone Joint Surg Br. 1992. 74:546–553.
Article6. Jones BG, Duncan RD. Open tibial fractures in children under 13 years of age--10 years experience. Injury. 2003. 34:776–780.
Article7. Kang CN, Kim JH, Kim DW, Gho YD, You JD, Chang J. The results and complications after treatment of open tibia fractures in children. J Korean Soc Fract. 1998. 11:464–470.
Article8. Yoon HK, Jeon KP, Oh KH, Jung DE, Km DJ, Kim HL. A clinical study of open fractures of the tibia in children. J Korean Soc Fract. 1993. 6:289–295.
Article9. Winquist RA, Hansen ST Jr, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am. 1984. 66:529–539.
Article10. Rosenthal RE, MacPhail JA, Oritz JE. Non-union in open tibial fractures. J Bone Joint Surg Am. 1977. 59:244–248.
Article11. Karlström G, Olerud S. Ipsilateral fracture of the femur and tibia. J Bone Joint Surg Am. 1977. 59:240–243.12. Myers SH, Spiegel D, Flynn JM. External fixation of high-energy tibia fractures. J Pediatr Orthop. 2007. 27:537–539.
Article13. Tolo VT. External fixation in multiply injured children. Orthop Clin North Am. 1990. 21:393–400.
Article14. Kubiak EN, Egol KA, Scher D, Wasserman B, Feldman D, Koval KJ. Operative treatment of tibial fractures in children: are elastic stable intramedullary nails an improvement over external fixation? J Bone Joint Surg Am. 2005. 87:1761–1768.
Article15. Sankar WN, Jones KJ, David Horn B, Wells L. Titanium elastic nails for pediatric tibial shaft fractures. J Child Orthop. 2007. 1:281–286.
Article16. Shannak AO. Tibial fractures in children: follow-up study. J Pediatr Orthop. 1988. 8:306–310.17. Gordon JE, Gregush RV, Schoenecker PL, Dobbs MB, Luhmann SJ. Complications after titanium elastic nailing of pediatric tibial fractures. J Pediatr Orthop. 2007. 27:442–446.
Article18. Blick SS, Brumback RJ, Poka A, Burgess AR, Ebraheim NA. Compartment syndrome in open tibial fractures. J Bone Joint Surg Am. 1986. 68:1348–1353.
Article19. Cole WG. Arterial injuries associated with fractures of the lower limbs in childhood. Injury. 1981. 12:460–463.
Article