J Korean Med Assoc.
2007 Dec;50(12):1072-1080. 10.5124/jkma.2007.50.12.1072.
Neuromuscular Block and Reversal
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Hanyang University College of Medicine, Korea. kimks@hanyang.ac.kr
- KMID: 2184955
- DOI: http://doi.org/10.5124/jkma.2007.50.12.1072
Abstract
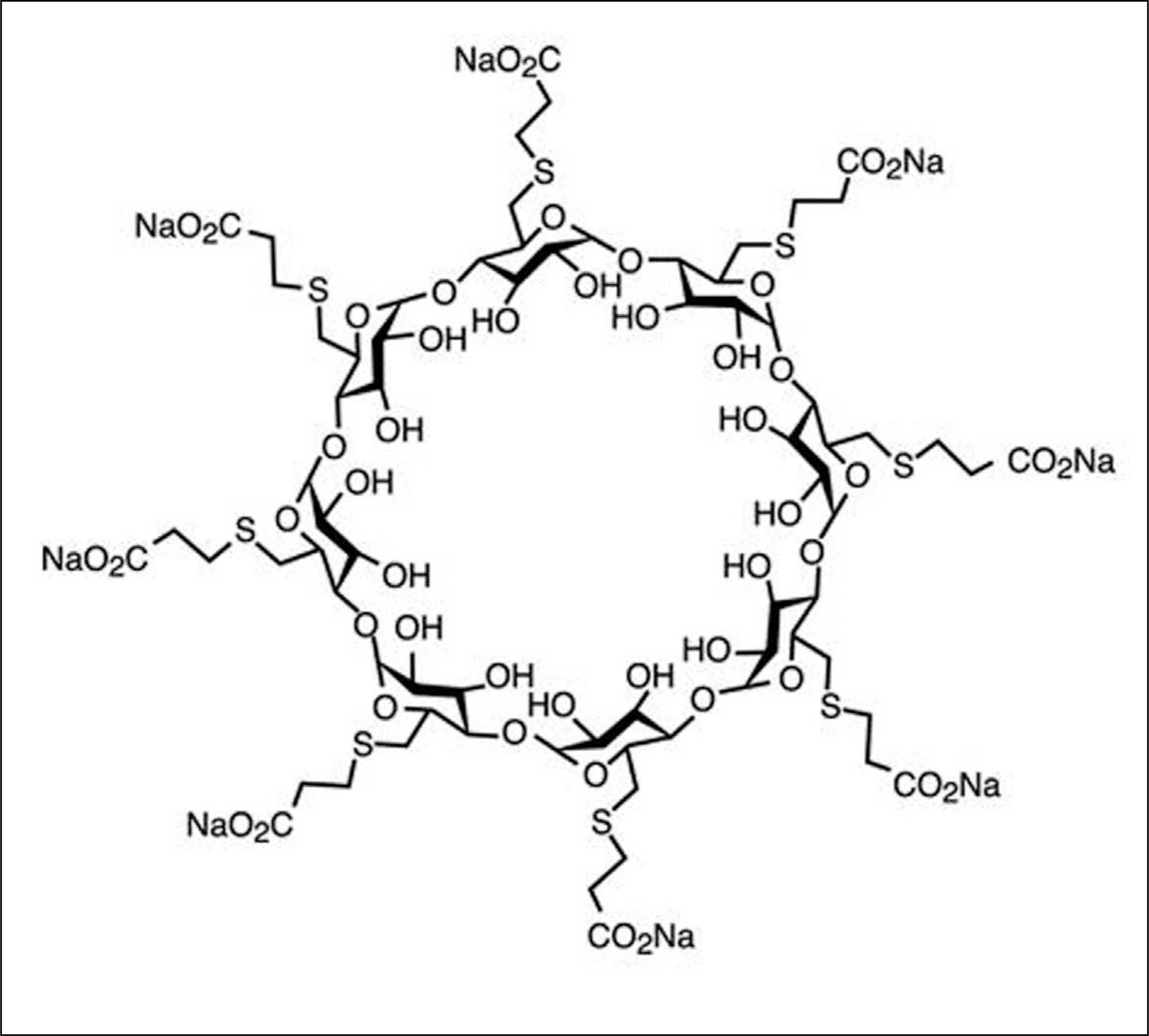
- The Griffith and Johnson's report of the successful use of curare in 1942 brought a revolution in anesthetic care. The only depolarizing agent still in use is succinylcholine due to its rapid onset of action and rapid recovery. However, its use is limited by serious side effects (hyperkalemia, malignant hyperthermia, arrhythmia, etc). New non-depolarizing neuromuscular blocking agents have been studied to replace succinylcholine, which are still at a preclinical level. Rocuronium is an aminosteroid compound and has an intermediate duration of action, but the onset is shorter. A new method of reversing neuromuscular blockade has been advocated by the introduction of a cyclodextrin, sugammadex (Org 25969), which is still at the investigational stage in humans. It has a high affinity for rocuronium, with which it forms a complex. Sugammadex has a lower affinity for other steroidal neuromuscular blocking agents such as vecuronium and pancuronium, and does not bind benzylisoquinoline-type neuromuscular blocking agents. The ability to produce a rapid return of twitch height even at deep levels of paralysis and the lack of side effects make this compound a promising new agent for anesthesia.
MeSH Terms
Figure
Cited by 1 articles
-
The Change of Severity of Epiblepharon after Induction of Total Intravenous Anesthesia without Muscle Relaxant
Young Jin Kim, Dong Geun Kim, Geun Mu Lee, Se Hun Lim, Jae Wook Yang
J Korean Ophthalmol Soc. 2016;57(4):540-545. doi: 10.3341/jkos.2016.57.4.540.
Reference
-
References
1. Griffith HR, Johnston GE. The use of curare in general anesthesia. Anesthesiology. 1942; 3:418–420.
Article2. Mayrhofer OK. Self? experiments with succinylcholine chloride; a new ultra?short?acting muscle relaxant. Br Med J. 1952; 21:1332–1334.3. Gronert GA, Theye RA. Pathophysiology of hyperkalemia induced by succinylcholine. Anesthesiology. 1975; 43:89–99.
Article4. Britt BA, Kalow W. Malignant hyperthermia: a statistical review. Can Anaesth Soc J. 1970; 17:293–315.
Article5. List WF. Succinylcholine?induced cardiac arrhythmias. Anesth Analg. 1971; 50:361–367.6. Adam JM, Bennett DJ, Bom A, Clark JK, Feilden H, Hutchinson EJ, Palin R, Prosser A, Rees DC, Rosair GM, Stevenson D, Tarver GJ, Zhang MQ. Cyclodextrin?derived host molecules as reversal agents for the neuromuscular blocker rocuronium bromide: synthesis and structure? activity relationships. J Med Chem. 2002; 45:1806–1816.7. Kim SY. Neuromuscular pharmacology in clinical anesthesia. 1st ed.Reston: Ryo Moon Gak;2000. p. 85–121.8. Savarese JJ, Ali HH, Basta SJ, Embree PB, Scott RP, Sunder N, Weakly JN, Wastila WB, el?Sayad HA. The clinical neuromuscular pharmacology of mivacurium chloride (BWB-1090U). A short?acting nondepolarizing ester neuromuscular blocking drug. Anesthesiology. 1988; 68:723–732.9. Basta SJ, Ali HH, Savarese JJ, Sunder N, Gionfriddo M, Cloutier G, Lineberry C, Cato AE. Clinical pharmacology of atracurium besylate (BW 33A): a new non?depolarizing muscle relaxant. Anesth Analg. 1982; 61:723–729.10. Belmont MR, Lien CA, Quessy S, Abou?Donia MM, Abalos A, Eppich L, Savarese JJ. The clinical neuromuscular pharmacology of 51W89 in patients receiving nitrous oxide/opioid/barbiturate anesthesia. Anesthesiology. 1995; 82:1139–1145.
Article11. Savage DS, Sleigh T, Carlyle I. The emergence of ORG NC 45, 1? [2 beta, 3 alpha, 5 alpha, 16 beta, 17 beta)?3, 17?bis (ace-tyloxy)?2?(1?piperidinyl)?androstan?16?yl]?1?methylpi-peridinium bromide, from the pancuronium series. Br J Anaesth. 1980; 52:3S–9S.12. Wierda JM, de Wit AP, Kuizenga K, Agoston S. Clinical observations on the neuromuscular blocking action of Org 9426, a new steroidal non?depolarizing agent. Br J Anaesth. 1990; 64:521–523.
Article13. Kahwaji R, Bevan DR, Bikhazi G, Shanks CA, Fragen RJ, Dyck JB, Angst MS, Matteo R. Dose?ranging study in younger adult and elderly patients of ORG 9487, a new, rapid?onset, short?duration muscle relaxant. Anesth Analg. 1997; 84:1011–1018.
Article14. Basta SJ, Savarese JJ, Ali HH, Embree PB, Schwartz AF, Rudd GD, Wastila WB. Clinical pharmacology of doxacurium chloride. A new long?acting nondepolarizing muscle relaxant. Anesthesiology. 1988; 69:478–486.15. McDowell SA, Clarke RS. A clinical comparison of pancuronium with d-tubocurarine. Anaesthesia. 1969; 24:581–590.
Article16. Ward S, Neill EA. Pharmacokinetics of atracurium in acute hepatic failure (with acute renal failure). Br J Anaesth. 1983; 55:1169–1172.
Article17. De Wolf AM, Freeman JA, Scott VL, Tullock W, Smith DA, Kisor DF, Kerls S, Cook DR. Pharmacokinetics and pharmacodynamics of cisatracurium in patients with end stage liver disease undergoing liver transplantation. Br J Anaesth. 1996; 76:624–628.18. Agoston S, Salt P, Newton D, Bencini A, Boomsma P, Erdmann W. The neuromuscular blocking action of ORG NC 45, a new pancuronium derivative, in anaesthetized patients. A pilot study. Br J Anaesth. 1980; 52:53S–59S.19. Huizinga AC, Vandenbrom RH, Wierda JM, Hommes FD, Hennis PJ. Intubating conditions and onset of neuromuscular block of rocuronium (Org 9426); a comparison with suxamethonium. Acta Anaesthesiol Scand. 1992; 36:463–468.
Article20. Kron SS. Severe bronchospasm and desaturation in a child associated with rapacuronium. Anesthesiology. 2001; 94:923–924.
Article21. Belmont MR, Lien CA, Tjan J, Bradley E, Stein B, Patel SS, Savarese JJ. Clinical pharmacology of GW280430A in humans. Anesthesiology. 2004; 100:768–773.
Article22. Gyermek L, Lee C, Nguyen N. Pharmacology of G?1?64, a new nondepolarizing neuromuscular blocking agent with rapid onset and short duration of action. Acta Anaesthesiol Scand. 1999; 43:651–657.
Article23. Gyermek L, Lee C, Cho YM, Nguyen N, Tsai SK. Neuromuscular pharmacology of TAAC3, a new nondepolarizing muscle relaxant with rapid onset and ultrashort duration of action. Anesth Analg. 2002; 94:879–885.
Article24. Michalek?Sauberer A, Nicolakis EM, Vizi ES, Gilly H. Effects of SZ1677, a new non?depolarizing steroidal neuromuscular blocking drug, and rocuronium on two laryngeal muscles and the anterior tibial muscle in guinea pigs. Acta Anaesthesiol Scand. 2006; 50:481–487.
Article25. Carroll MT, Mirakhur RK, Lowry DW, McCourt KC, Kerr C. Neuromuscular blocking effects and train?of?four fade with cisatracurium: comparison with other nondepolarising relaxants. Anaesthesia. 1998; 53:1169–1173.
Article26. Debaene B, Plaud B, Dilly MP, Donati F. Residual paralysis in the PACU after a single intubating dose of nondepolarizing muscle relaxant with an intermediate duration of action. Anesthesiology. 2003; 98:1042–1048.
Article27. Bradley PB, Dhawan BN, Wolstencroft JH. Pharmacological properties of cholinoceptive neurones in the medulla and pons of the cat. J Physiol. 1966; 183:658–674.
Article28. Stone TW. Cholinergic mechanisms in the rat somatosensory cerebral cortex. J Physiol. 1972; 225:485–499.
Article29. Bradley PB, Elkes J. The effect of atropine, hyoscyamine, physostigmine and neostigmine on the electrical activity of the brain of the conscious cat. J Physiol. 1953; 120:14P–15P.30. Katz RL. Neuromuscular effects of d?tubocurarine, edrophonium and neostigmine in man. Anesthesiology. 1967; 28:327–336.
Article31. McNall PG, Wolfson B, Tuazon JG, Siker ES. Use of pyridostigmine for the reversal of neuromuscular blockade. Anesth Analg. 1969; 48:1026–1032.
Article32. Mandel ID, Katz R, Zengo A, Kutscher AH, Greenberg RA, Katz S, Scharf R, Pintoff A. The effect of pharmacologic agents on salivary secretion and composition in man. I. Pilocarpine, atropine and anticholinesterases. J Oral Ther Pharmacol. 1967; 4:192–199.33. Klingenmaier CH, Bullard R, Thompson D, Watson R. Reversal of neuromuscular blockade with a mixture of neostigmine and glycopyrrolate. Anesth Analg. 1972; 51:468–472.
Article34. Wulf H, Ledowski T, Linstedt U, Proppe D, Sitzlack D. Neuromuscular blocking effects of rocuronium during desflurane, isoflurane, and sevoflurane anaesthesia. Can J Anaesth. 1998; 45:526–532.
Article35. Kim KS, Cheong MA, Lee HJ, Lee JM. Tactile assessment for the reversibility of rocuronium?induced neuromuscular blockade during propofol or sevoflurane anesthesia. Anesth Analg. 2004; 99:1080–1085.
Article36. Bevan DR, Donati F, Kopman AF. Reversal of neuromuscular blockade. Anesthesiology. 1992; 77:785–805.37. Kim KS, Lew SH, Cho HY, Cheong MA. Residual paralysis induced by either vecuronium or rocuronium after reversal with pyridostigmine. Anesth Analg. 2002; 95:1656–1660.
Article38. Rupp SM, McChristian JW, Miller RD, Taboada JA, Cronnelly R. Neostigmine and edrophonium antagonism of varying intensity neuromuscular blockade induced by atracurium, pancuronium, or vecuronium. Anesthesiology. 1986; 64:711–717.39. Murphy GS, Szokol JW, Marymont JH, Franklin M, Avram MJ, Vender JS. Residual paralysis at the time of tracheal extubation. Anesth Analg. 2005; 100:1840–1845.
Article40. Berg H, Roed J, Viby?Mogensen J, Mortensen CR, Engbaek J, Skovgaard LT, Krintel JJ. Residual neuromuscular block is a risk factor for postoperative pulmonary complications. A prospective, randomised, and blinded study of postoperative pulmonary complications after atracurium, vecuronium and pancuronium. Acta Anaesthesiol Scand. 1997; 41:1095–1103.
Article41. Naguib M. Sugammadex: another milestone in clinical neuromuscular pharmacology. Anesth Analg. 2007; 104:575–581.
Article42. Bom A, Bradley M, Cameron K, Clark JK, Van Egmond J, Feilden H, MacLean EJ, Muir AW, Palin R, Rees DC, Zhang MQ. A novel concept of reversing neuromuscular block: chemical encapsulation of rocuronium bromide by a cyclo-dextrin?based synthetic host. Angew Chem Int Ed Engl. 2002; 41:266–270.
Article43. Gijsenbergh F, Ramael S, Houwing N, van Iersel T. First human exposure of Org 25969, a novel agent to reverse the action of rocuronium bromide. Anesthesiology. 2005; 103:695–703.
Article44. de Boer HD, van Egmond J, van de Pol F, Bom A, Booij LH. Sugammadex, a new reversal agent for neuromuscular block induced by rocuronium in the anaesthetized Rhesus monkey. Br J Anaesth. 2006; 96:473–479.
Article45. Bom A, Hope F. Neuromuscular block induced by rocuronium and reversed by the encapsulating agent Org 25969 can be re?established using the non?steroidal neuromuscular blockers succinylcholine and cis?atracurium. Eur J Anaesthiol. 2005; 22(S34):): A457.
Article46. Paton WD, Waud DR. The margin of safety of neuromuscular transmission. J Physiol. 1967; 191:59–90.
Article47. Sorgenfrei IF, Norrild K, Larsen PB, Stensballe J, Ostergaard D, Prins ME, Viby?Mogensen J. Reversal of rocuronium? induced neuromuscular block by the selective relaxant binding agent sugammadex: a dose?finding and safety study. Anesthesiology. 2006; 104:667–674.48. de Boer HD, Driessen JJ, Marcus MA, Kerkkamp H, Heeringa M, Klimek M. Reversal of rocuronium?induced (1.2mg/kg) profound neuromuscular block by sugammadex: a multicenter, dose?finding and safety study. Anesthesiology. 2007; 107:239–244.49. Molina AL, de Boer HD, Klimek M, Heeringa M, Klein J. Reversal of rocuronium?induced (1.2mgkg?1) profound neuromuscular block by accidental high dose of sugammadex (40mg kg?1). Br J Anaesth. 2007; 98:624–627.50. Suresh D, Carter JA, Whitehead JP, Goldhill DR, Flynn PJ. Cardiovascular changes at antagonism of atracurium. Effects of different doses of premixed neostigmine and glycopyrro-nium in a ratio of 5: 1. Anaesthesia. 1991; 46:877–880.51. King MJ, Milazkiewicz R, Carli F, Deacock AR. Influence of neostigmine on postoperative vomiting. Br J Anaesth. 1988; 61:403–406.
Article52. Kopman AF. Sugammadex: a revolutionary approach to neuromuscular antagonism. Anesthesiology. 2006; 104:631–633.
Article53. Lenz A, Hill G, White PF. Emergency use of sugammadex after failure of standard reversal drugs. Anesth Analg. 2007; 104:585–586.
Article54. Hayes AH, Breslin DS, Mirakhur RK, Reid JE, O'Hare RA. Frequency of haemoglobin desaturation with the use of succinylcholine during rapid sequence induction of anaesthesia. Acta Anaesthesiol Scand. 2001; 45:746–749.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical use of sugammadex
- A survey of postoperative residual neuromuscular block and neuromuscular monitoring
- The Effect of Gentamicin of Magnesium on Mivacurium-induced Neuromuscular Block and its Reversal in Cats
- Choice of neuromuscular block reversal agent to reduce postoperative pulmonary complications
- Reversal of Neuromuscular Blockade with Neostigmine Does not Increase the Incidence of Postoperative Nausea and Vomiting