J Korean Med Assoc.
2007 Jun;50(6):482-493. 10.5124/jkma.2007.50.6.482.
Causes and Diagnostic Strategies for Chronic Low Back Pain
- Affiliations
-
- 1Department of Neurosurgery, Presbyterian Medical Center, Korea. hyoungihl@hotmail.com, sdh8262@hanmail.net
- KMID: 2184858
- DOI: http://doi.org/10.5124/jkma.2007.50.6.482
Abstract
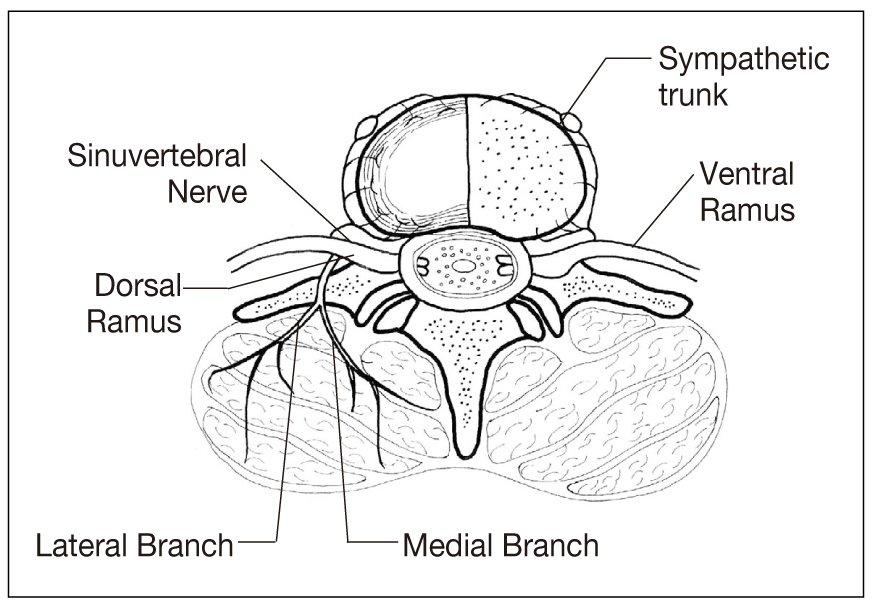
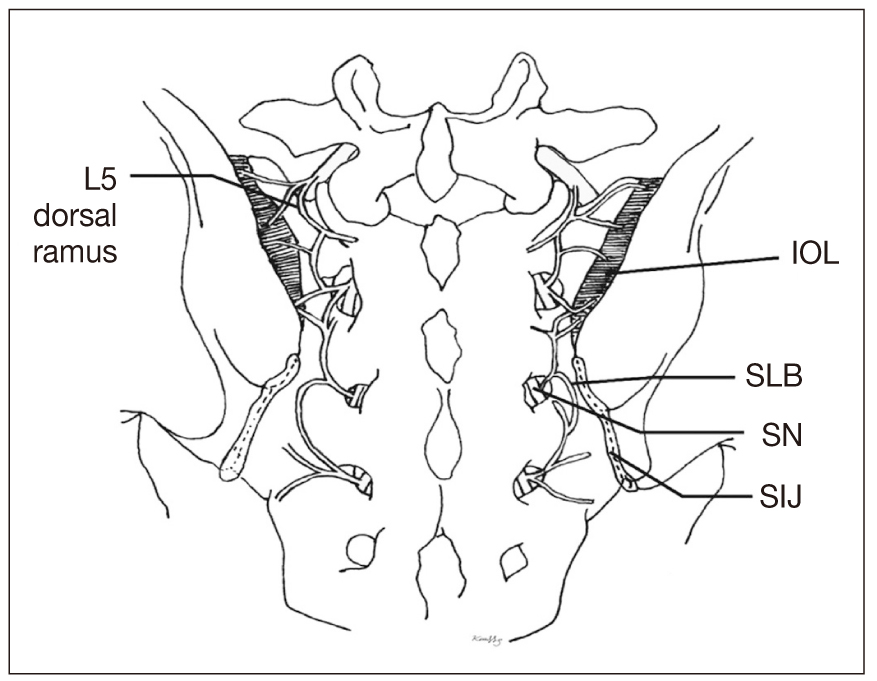
- Chronic low back pain (CLBP) has become more prominent with globally increasing life expectancy. Its cause is more attributable to degenerative changes than to traumatic lesions. Although the diagnosis of CLBP is recently on higher demand, lack of clinical features and non-informative imaging findings in patients with CLBP are challenging to clinicians to establish the diagnosis. Therefore, understanding of the new concept of pathogenesis, elimination of prejudice, and evidence-based diagnostic steps are required to resolve the question of pain source. Analysis of pain distribution patterns and careful history taking can be utilized as an initial guide to divide CLBP into somatic and radicular pain. Zygapophyseal joint pain and sacroiliac joint pain representing somatic pain can be further investigated using medial branch and sacroiliac joint blocks. However, comparative blocks are essential to decreased false positive rate. Infiltration of a small volume of local anesthetics can increase the specificity of the procedures. Discogenic pain stemming from internal disk derangement can be confirmed by pressure-controlled discography. Automated discography is recommended to provide the constant rate of dye injection with obviating the fluctuation of intradiscal pressure. Evidencebased concept and diagnostic procedures can provide more accurate and efficient methods to establish the diagnosis of CLBP.
MeSH Terms
Figure
Reference
-
1. Merskey H, Bogduk N, editors. Classification of chronic pain: description of chronic pain syndromes and definition of pain terms. 1994. 2nd ed. Seattle: IASP Press;40–43.2. Andersson GBJ. Epidemiological features of chronic low back pain. Lancet. 1999. 354:581–582.3. Haldeman S. Low back pain: current physiologic concepts. Neurol Clin. 1999. 17:1–15.4. Borenstein D. Epidemiology, etiology, diagnostic evaluation, and treatment of low back pain. Curr Opin Rheumatol. 1996. 8:124–129.
Article5. Adams MA, Bogduk N, Burton K, Dolan P. Epidemiology of low back trouble. The biomechanics of back pain. 2002. London: Churchill Livingstone;79–132.6. Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine. 1995. 20:31–37.
Article7. Schwarzer AC, Wang SC, Bogduk N. Prevalence and clinical feature of lumbar zygapophysial joint pain: A study in an Australian population with chronic low back pain. Ann Rheum Dis. 1995. 54:100–106.
Article8. Schwarzer AC, April CN, Derby R. The prevalence and clinical features of internal disc disruption in patients with chronic back pain. Spine. 1995. 20:1878–1883.
Article9. Bogduk N, Willson A, Tynan W. The human lumbar dorsal rami. J Anat. 1982. 134:383–397.10. Green G, Baljet B, Drukker J. Nerves and nerve plexuses of the human vertebral column. Am J Anat. 1990. 188:282–296.
Article11. Yin W, Willard F, Carreiro J, Drey fuss P HB, Pauza K, Joshi A, Mclarty J, Bogduk N. Sensory stimulation-guided sacroiliac joint radiofrequency neurotomy: Technique based on neuroanatomy of the dorsal sacral plexus. Spine. 2003. 28:2419–2425.
Article12. Nachemson A, Wadell G, Norlund A. Nachemson A, Jonsson E, editors. Epidemiology of neck and low back pain. Neck and back pain: the scientific evidence of causes, diagnosis, treatment. 2000. Philadelphia: Lippincott, Williams & Wilkins;165–188.13. Bogduk N, Govind J, editors. Medical management of acute lumbar radicular pain: an evidence-based approach. 1999. Newcastle: Newcastle Bone and Joint Institute;33–40.14. Osti OL, Fraser RD. MRI and discography of annular tears and intervertebral disc degeneration. A prospective clinical comparison. J Bone Joint Surg Br. 1992. 74:431–435.
Article15. Boos N, Rieder R, Schade V, Psych D, Spratt KF, Semmer N, Psych D, Aebi M. The diagnostic accuracy of magnetic resonance imaging, work perception and psychosocial factors in identifying symptomatic disk herniations. Spine. 1995. 20:2613–2625.
Article16. Grant PA. Electrodiagnostic medical consultation in lumbar spine problems. Occup Med. 1998. 13:197–120.17. Lomen-Hoerth C, Aminoff MJ. Clinical neurophysiologic studies: which test is useful and when? Neurol Clin. 1999. 17:65–74.18. Peng B, Wu W, Li Z, Guo J, Wang X. Chemical radiculitis. Pain. 2007. 127:11–16.
Article19. Piperno M, Graverand M, Reboul P, Mathieu P, Tron A, Perrin G, Peschard M, Richard M, Vignon E. Phospholipase A2 activity in herniated lumbar discs. Spine. 1997. 22:2061–2065.
Article20. Freemont AJ, Watkins A, Le Maitre C, Jeziorska M, Hoyland JA. Current understanding of cellular and molecular events in intervertebral disc degeneration: implications for therapy. J Pathol. 2002. 196:374–379.
Article21. Ozaktay AC, Kallakuri S, Cavanaugh JM. Phospholipase A2 sensitivity of the dorsal root and dorsal root ganglion. Spine. 1998. 23:1296–1306.
Article22. Bogduk N. Bogduk N, editor. Low back pain. Clinical anatomy of the lumbar spine and sacrum. 2002. London: Churchill Livingstone;187–213.23. Schwarzer AC, Aprill C, Derby R, Fortin J, Kine G, Bogduk N. Clinical features of patients with pain stemming from the lumbar zygapophysial joints. Is the lumbar facet syndrome a clinical entity? Spine. 1994. 19:1132–1137.
Article24. Kim HI, Shin DG, Shin DA, Lee JO. Pain evaluation for decision making for management of spinal pain. J of the Kor Soc of Ster and Func Neurosurg. 2005. 1:44–50.25. Kim HJ, Shin DG, Kim HI, Shin DA. Selective neurotomy of sacral lateral branches for pain of sacroiliac joint dysfunction. J Korean Neurosurg Soc. 2005. 38:338–343.26. Mixter WJ, Barr JS. Rupture of intervertebral disc with involvement of the spinal canal. New Engl J Med. 1934. 211:210–215.27. Shin DA, Kim HI, Jung JH, Shin DG, Lee JO. Diagnostic relevance of pressure-controlled discography. J Korean Med Sci. 2006. 21:911–916.
Article28. Derby R, Howard MW, Grant JM, Lettice JJ, Van Peteghem PK, Ryan DP. The ability of pressure-controlled discography to predict surgical and nonsurgical outcomes. Spine. 1999. 24:364–371.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oceupational Chronic Low Baek Pain: A Case Report
- Interventional therapy for chronic low back pain
- Treatment of Chronic Low Back and Leg Pain Using a Spinal Cord Stimulator: Two case reports
- The Potency of Platelet-Rich Plasma for Chronic Low Back Pain: A Systematic Review and Metaanalysis of Randomized Controlled Trial
- Effect of Topical Capsaicin in Chronic Low Back and Posterior Neck Pain