J Clin Neurol.
2015 Jan;11(1):20-25. 10.3988/jcn.2015.11.1.20.
Cognitive Function in Childhood Epilepsy: Importance of Attention Deficit Hyperactivity Disorder
- Affiliations
-
- 1Department of Pediatrics, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea. tsko@amc.seoul.kr
- 2Department of Psychiatry, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2179568
- DOI: http://doi.org/10.3988/jcn.2015.11.1.20
Abstract
- BACKGROUND AND PURPOSE
To determine how cognitive function is related to epilepsy classification and comorbid attention deficit hyperactivity disorder (ADHD) in children with newly diagnosed epilepsy of genetic or unknown etiology.
METHODS
The medical records of children aged 6-16 years with newly diagnosed epilepsy of genetic or unknown etiology were reviewed retrospectively. The Korean Education Development Institute-Wechsler Intelligence Scale for Children and the Comprehensive Attention Test were used to evaluate intelligence and attention/executive function, respectively.
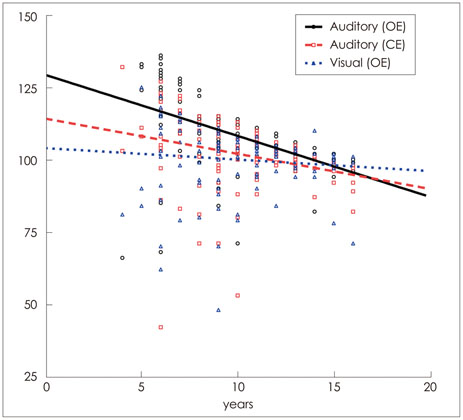
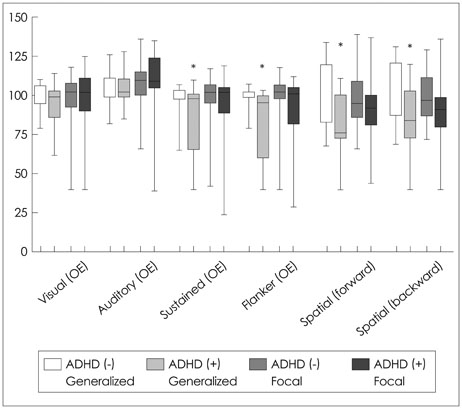
RESULTS
The data of a total of 149 children, 103 with focal seizures and 46 with generalized seizures, were reviewed. The prevalence of ADHD was 49.2% (59 out of 120 examined patients), and ADHD patients exhibited significantly worse auditory selective attention, flanker test results, and spatial working memory. Patients with generalized seizures exhibited significantly worse auditory selective and sustained attention than patients with focal seizures. In patients with generalized seizures, sustained attention, flanker test findings, and spatial working memory were found to be affected by ADHD, and auditory selective and sustained attention were significantly worse in patients with benign childhood epilepsy with centrotemporal spikes and ADHD than in their counterparts without ADHD.
CONCLUSIONS
Cognitive processes are affected by seizure type and comorbid ADHD. Proper characterization of these neuropsychiatric impairments may allow earlier intervention during the disease course.
MeSH Terms
Figure
Cited by 1 articles
-
Cognitive Function and Neuropsychological Comorbidities in Children with Newly Diagnosed Idiopathic Epilepsy
Seung Yun Lee, Jang-Ho Park, Sin-Jae Park, Yangho Kim, Kyung Yeon Lee
J Korean Med Sci. 2018;33(3):. doi: 10.3346/jkms.2018.33.e17.
Reference
-
1. Russ SA, Larson K, Halfon N. A national profile of childhood epilepsy and seizure disorder. Pediatrics. 2012; 129:256–264.
Article2. Elger CE, Helmstaedter C, Kurthen M. Chronic epilepsy and cognition. Lancet Neurol. 2004; 3:663–672.
Article3. Selassie GR, Viggedal G, Olsson I, Jennische M. Speech, language, and cognition in preschool children with epilepsy. Dev Med Child Neurol. 2008; 50:432–438.
Article4. Berg AT, Smith SN, Frobish D, Levy SR, Testa FM, Beckerman B, et al. Special education needs of children with newly diagnosed epilepsy. Dev Med Child Neurol. 2005; 47:749–753.
Article5. Helmstaedter C, Aldenkamp AP, Baker GA, Mazarati A, Ryvlin P, Sankar R. Disentangling the relationship between epilepsy and its behavioral comorbidities - the need for prospective studies in new-onset epilepsies. Epilepsy Behav. 2014; 31:43–47.
Article6. MacAllister WS, Schaffer SG. Neuropsychological deficits in childhood epilepsy syndromes. Neuropsychol Rev. 2007; 17:427–444.
Article7. Bhise VV, Burack GD, Mandelbaum DE. Baseline cognition, behavior, and motor skills in children with new-onset, idiopathic epilepsy. Dev Med Child Neurol. 2010; 52:22–26.
Article8. Jeong MH, Yum MS, Ko TS, You SJ, Lee EH, Yoo HK. Neuropsychological status of children with newly diagnosed idiopathic childhood epilepsy. Brain Dev. 2011; 33:666–671.
Article9. Mandelbaum DE, Burack GD. The effect of seizure type and medication on cognitive and behavioral functioning in children with idiopathic epilepsy. Dev Med Child Neurol. 1997; 39:731–735.
Article10. You SJ. Cognitive function of idiopathic childhood epilepsy. Korean J Pediatr. 2012; 55:159–163.
Article11. Hermann B, Jones J, Sheth R, Dow C, Koehn M, Seidenberg M. Children with new-onset epilepsy: neuropsychological status and brain structure. Brain. 2006; 129(Pt 10):2609–2619.
Article12. Rappley MD. Clinical practice. Attention deficit-hyperactivity disorder. N Engl J Med. 2005; 352:165–173.13. Chou IC, Chang YT, Chin ZN, Muo CH, Sung FC, Kuo HT, et al. Correlation between epilepsy and attention deficit hyperactivity disorder: a population-based cohort study. PLoS One. 2013; 8:e57926.
Article14. Gillis L, Kaye E. Diagnosis and management of mitochondrial diseases. Pediatr Clin North Am. 2002; 49:203–219.
Article15. Berg AT, Berkovic SF, Brodie MJ, Buchhalter J, Cross JH, van Emde Boas W, et al. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005-2009. Epilepsia. 2010; 51:676–685.
Article16. Park KS, Yoon JR, Park HJ, Park HJ, Kwon KO. Korean educational developmental institute-Wechsler intelligence scale for children (KEDI-WISC). Seoul: Korean Educational Development Institute;2002.17. Yoo HK, Lee J, Kang SH, Park EH, Jung J, Kim BN, et al. Standardization of the comprehensive attention test for the Korean children and adolescents. J Korean Acad Child Adolesc Psychiatry. 2009; 20:68–75.18. Socanski D, Aurlien D, Herigstad A, Thomsen PH, Larsen TK. Epilepsy in a large cohort of children diagnosed with attention deficit/hyperactivity disorders (ADHD). Seizure. 2013; 22:651–655.
Article19. Liu ST, Tsai FJ, Lee WT, Lee CM, Fan PC, Lin WS, et al. Attentional processes and ADHD-related symptoms in pediatric patients with epilepsy. Epilepsy Res. 2011; 93:53–65.
Article20. Dunn DW. Attention-deficit hyperactivity disorder, oppositional defiant disorder and conduct disorder. In : Ettinger AB, Kanner AM, editors. Psychiatric aspects of epilepsy: a practical guide to diagnosis and treatment. Baltimore: Lippincott/Williams & Wilkins;2001. p. 111–126.21. Semrud-Clikeman M, Wical B. Components of attention in children with complex partial seizures with and without ADHD. Epilepsia. 1999; 40:211–215.
Article22. Bechtel N, Kobel M, Penner IK, Specht K, Klarhöfer M, Scheffler K, et al. Attention-deficit/hyperactivity disorder in childhood epilepsy: a neuropsychological and functional imaging study. Epilepsia. 2012; 53:325–333.
Article23. MacAllister WS, Vasserman M, Vekaria P, Miles-Mason E, Hochsztein N, Bender HA. Neuropsychological endophenotypes in ADHD with and without epilepsy. Appl Neuropsychol Child. 2012; 1:121–128.
Article24. Lenartowicz A, Delorme A, Walshaw PD, Cho AL, Bilder RM, McGough JJ, et al. Electroencephalography correlates of spatial working memory deficits in attention-deficit/hyperactivity disorder: vigilance, encoding, and maintenance. J Neurosci. 2014; 34:1171–1182.
Article25. Kim S, Liu Z, Glizer D, Tannock R, Woltering S. Adult ADHD and working memory: neural evidence of impaired encoding. Clin Neurophysiol. 2014; 125:1596–1603.
Article26. Dafoulis V, Kalyva E. Factors associated with behavioral problems in children with idiopathic epilepsy. Epilepsy Res. 2012; 100:104–112.
Article27. Maneshi M, Moeller F, Fahoum F, Gotman J, Grova C. Resting-state connectivity of the sustained attention network correlates with disease duration in idiopathic generalized epilepsy. PLoS One. 2012; 7:e50359.
Article28. Giordani B, Berent S, Sackellares JC, Rourke D, Seidenberg M, O'Leary DS, et al. Intelligence test performance of patients with partial and generalized seizures. Epilepsia. 1985; 26:37–42.
Article29. Tian Y, Dong B, Ma J, Zhou S, Zhou N, Wang K. Attention networks in children with idiopathic generalized epilepsy. Epilepsy Behav. 2010; 19:513–517.
Article30. Nee DE, Jonides J, Berman MG. Neural mechanisms of proactive interference-resolution. Neuroimage. 2007; 38:740–751.
Article31. Smith EE, Jonides J. Storage and executive processes in the frontal lobes. Science. 1999; 283:1657–1661.
Article32. Purper-Ouakil D, Ramoz N, Lepagnol-Bestel AM, Gorwood P, Simonneau M. Neurobiology of attention deficit/hyperactivity disorder. Pediatr Res. 2011; 69(5 Pt 2):69R–76R.
Article33. Aghakhani Y, Bagshaw AP, Bénar CG, Hawco C, Andermann F, Dubeau F, et al. fMRI activation during spike and wave discharges in idiopathic generalized epilepsy. Brain. 2004; 127(Pt 5):1127–1144.
Article34. Stefan H, Paulini-Ruf A, Hopfengärtner R, Rampp S. Network characteristics of idiopathic generalized epilepsies in combined MEG/EEG. Epilepsy Res. 2009; 85:187–198.
Article35. Kwon S, Seo HE, Hwang SK. Cognitive and other neuropsychological profiles in children with newly diagnosed benign rolandic epilepsy. Korean J Pediatr. 2012; 55:383–387.
Article36. Chevalier H, Metz-Lutz MN, Segalowitz SJ. Impulsivity and control of inhibition in Benign Focal Childhood Epilepsy (BFCE). Brain Cogn. 2000; 43:86–90.37. Holtmann M, Becker K, Kentner-Figura B, Schmidt MH. Increased frequency of rolandic spikes in ADHD children. Epilepsia. 2003; 44:1241–1244.
Article38. Holtmann M, Matei A, Hellmann U, Becker K, Poustka F, Schmidt MH. Rolandic spikes increase impulsivity in ADHD - a neuropsychological pilot study. Brain Dev. 2006; 28:633–640.
Article39. Schneebaum-Sender N, Goldberg-Stern H, Fattal-Valevski A, Kramer U. Does a normalizing electroencephalogram in benign childhood epilepsy with centrotemporal spikes abort attention deficit hyperactivity disorder? Pediatr Neurol. 2012; 47:279–283.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Report of a Child who has Attention Deficit Hyperactivity Disorder, Mental Retardation, and Mania
- The Effect of Attention Level of Attention Deficit Hyperactivity Disorder on CPT and WCST
- Efficacy and Safety of Methylphenidate in Children with Epilepsy and Attention Deficit Hyperactivity Disorder
- Diagnosis and Comorbidity of Attention Deficit Hyperactivity Disorder in School-Aged Children
- Diagnosis and Management of Attention Deficit Hyperactivity Disorder