J Clin Neurol.
2014 Jul;10(3):229-235. 10.3988/jcn.2014.10.3.229.
Abnormal Brain Activity Changes in Patients with Migraine: A Short-Term Longitudinal Study
- Affiliations
-
- 1School of Life Science and Technology, Xidian University, Xi'an, PR China. liujixin@life.xidian.edu.cn
- 2The 3rd Teaching Hospital, Chengdu University of Traditional Chinese Medicine, Chengdu, PR China. lfr@cdutcm.edu.cn
- 3Department of Medical Imaging, First Affiliated Hospital, Xi'an Jiaotong University College of Medicine, Xi'an, PR China.
- 4Information Processing Laboratory, School of Information Engineering, Inner Mongolia University of Science and Technology, Baotou, Inner Mongolia, PR China.
- KMID: 2179450
- DOI: http://doi.org/10.3988/jcn.2014.10.3.229
Abstract
- BACKGROUND AND PURPOSE
Whether or not migraine can cause cumulative brain alterations due to frequent migraine-related nociceptive input in patients is largely unclear. The aim of this study was to characterize longitudinal changes in brain activity between repeated observations within a short time interval in a group of female migraine patients, using resting-state functional magnetic resonance imaging.
METHODS
Nineteen patients and 20 healthy controls (HC) participated in the study. Regional homogeneity (ReHo) and functional interregional connectivity were assessed to determine the focal and global features of brain dysfunction in migraine. The relationship between changes in headache parameters and longitudinal brain alterations were also investigated.
RESULTS
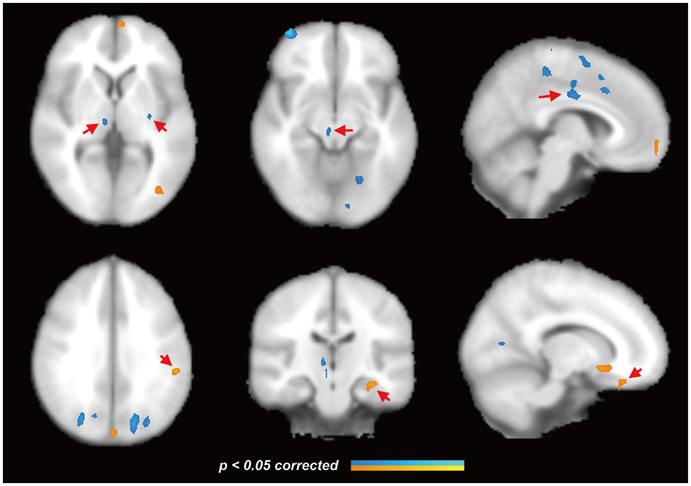
All patients reported that their headache activity increased over time. Abnormal ReHo changes in the patient group relative to the HC were found in the putamen, orbitofrontal cortex, secondary somatosensory cortex, brainstem, and thalamus. Moreover, these brain regions exhibited longitudinal ReHo changes at the 6-week follow-up examination. These headache activity changes were accompanied by disproportionately dysfunctional connectivity in the putamen in the migraine patients, as revealed by functional connectivity analysis, suggesting that the putamen plays an important role in integrating diverse information among other migraine-related brain regions.
CONCLUSIONS
The results obtained in this study suggest that progressive brain aberrations in migraine progress as a result of increased headache attacks.
MeSH Terms
Figure
Reference
-
1. May A. New insights into headache: an update on functional and structural imaging findings. Nat Rev Neurol. 2009; 5:199–209.
Article2. Bussone G. Pathophysiology of migraine. Neurol Sci. 2004; 25:Suppl 3. S239–S241.
Article3. Maleki N, Becerra L, Pendse G, Brawn J, Bigal M, et al. Migraine attacks the Basal Ganglia. Mol Pain. 2011; 7:71.
Article4. Liu J, Qin W, Nan J, Li J, Yuan K, Zhao L, et al. Gender-Related Differences in the Dysfunctional Resting Networks of Migraine Suffers. PLoS One. 2011; 6:e27049.
Article5. Liu J, Zhao L, Li G, Xiong S, Nan J, Li J, et al. Hierarchical Alteration of Brain Structural and Functional Networks in Female Migraine Sufferers. PloS One. 2012; 7:e51250.
Article6. Yu D, Yuan K, Zhao L, Zhao L, Dong M, Liu P, et al. Regional homogeneity abnormalities in patients with interictal migraine without aura: a resting-state study. NMR Biomed. 2012; 25:806–812.
Article7. Schmitz N, Admiraal F, Arkink EB, Kruit MC, Schoonman GG, Ferrari MD, et al. Attack frequency and disease duration as indicators for brain damage in migraine. Headache. 2008; 48:1044–1055.
Article8. Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004; 24:Suppl 1. 9–160.9. Detsky ME, McDonald DR, Baerlocher MO, Tomlinson GA, McCrory DC, Booth CM. Does this patient with headache have a migraine or need neuroimaging? JAMA. 2006; 296:1274–1283.
Article10. Zang Y, Jiang T, Lu Y, He Y, Tian L. Regional homogeneity approach to fMRI data analysis. Neuroimage. 2004; 22:394–400.
Article11. Zuo XN, Xu T, Jiang L, Yang Z, Cao XY, He Y, et al. Toward reliable characterization of functional homogeneity in the human brain: Preprocessing, scan duration, imaging resolution and computational space. Neuroimage. 2013; 65:374–386.
Article12. Kendall MG, Gibbons JD. Rank correlation methods. 5th ed. New York: Oxford University Press;1990.13. Bullmore ET, Suckling J, Overmeyer S, Rabe-Hesketh S, Taylor E, Brammer MJ. Global, voxel, and cluster tests, by theory and permutation, for a difference between two groups of structural MR images of the brain. IEEE Trans Med Imaging. 1999; 18:32–42.
Article14. Schwedt TJ, Dodick DW. Advanced neuroimaging of migraine. Lancet Neurol. 2009; 8:560–568.
Article15. Davis KD, Moayedi M. Central Mechanisms of Pain Revealed Through Functional and Structural MRI. J Neuroimmune Pharmacol. 2013; 8:518–534.
Article16. May A. Neuroimaging: visualising the brain in pain. Neurol Sci. 2007; 28:Suppl 2. S101–S107.
Article17. Wu T, Long X, Zang Y, Wang L, Hallett M, Li K, et al. Regional homogeneity changes in patient's with Parkinsons disease. Hum Brain Mapp. 2009; 30:1502–1510.
Article18. Baliki MN, Schnitzer TJ, Bauer WR, Apkarian AV. Brain morphological signatures for chronic pain. PLoS One. 2011; 6:e26010.
Article19. Akerman S, Holland PR, Goadsby PJ. Diencephalic and brainstem mechanisms in migraine. Nat Rev Neurosci. 2011; 12:570–584.
Article20. Goadsby PJ, Lipton RB, Ferrari MD. Migraine-current understanding and treatment. N Engl J Med. 2002; 346:257–270.21. May A, Goadsby PJ. The trigeminovascular system in humans: pathophysiologic implications for primary headache syndromes of the neural influences on the cerebral circulation. J Cereb Blood Flow Metab. 1999; 19:115–127.
Article22. Weiller C, Mav A, LlMmroth V, Jüptner M, Kaube H, Schayck RV, et al. Brain stem activation in spontaneous human migraine attacks. Nat Med. 1995; 1:658–660.
Article23. Afridi SK, Giffin NJ, Kaube H, Friston KJ, Ward NS, Frackowiak RS, et al. A positron emission tomographic study in spontaneous migraine. Arch Neurol. 2005; 62:1270–1275.
Article24. Tassorelli C, Joseph SA. Systemic nitroglycerin induces Fos immunoreactivity in brainstem and forebrain structures of the rat. Brain Res. 1995; 682:167–181.
Article25. Lambert GA, Donaldson C, Boers PM, Zagami AS. Activation of trigeminovascular neurons by glyceryl trinitrate1. Brain Res. 2000; 887:203–210.26. Afridi SK, Matharu MS, Lee L, Kaube H, Friston KJ, Frackowiak RS, et al. A PET study exploring the laterality of brainstem activation in migraine using glyceryl trinitrate. Brain. 2005; 128:932–939.
Article27. Bahra A, Matharu MS, Buchel C, Frackowiak RSJ, Goadsby PJ. Brainstem activation specific to migraine headache. Lancet. 2001; 357:1016–1017.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long Term Follow-up of Cyclic Vomiting Syndrome
- Clinical Characteristics of Memory Disturbance in Patients with Traumatic Brain Injury Referred for Mental Disabilitiy Evaluation
- Persistent Aura Without Infarction
- Vestibular migraine of childhood
- Alice in Wonderland Syndrome in a Child with an Electroencephalographic Abnormality: A Case Report