J Clin Neurol.
2013 Apr;9(2):133-137. 10.3988/jcn.2013.9.2.133.
A Case of Frontotemporal Dementia with Amyotrophic Lateral Sclerosis Presenting with Pathological Gambling
- Affiliations
-
- 1Department of Psychiatry, Ankara University School of Medicine, Ankara, Turkey. etozel@medicine.ankara.edu.tr
- 2Department of Neurology, Ankara University School of Medicine, Ankara, Turkey.
- KMID: 2179175
- DOI: http://doi.org/10.3988/jcn.2013.9.2.133
Abstract
- BACKGROUND
Pathological gambling (PG), which is characterized by consistent, repetitive gambling and unsuccessful quitting attempts, is classified as an impulse control disorder. PG has also been reported in patients with Parkinson's disease, frontotemporal dementia, and amyotrophic lateral sclerosis.
CASE REPORT
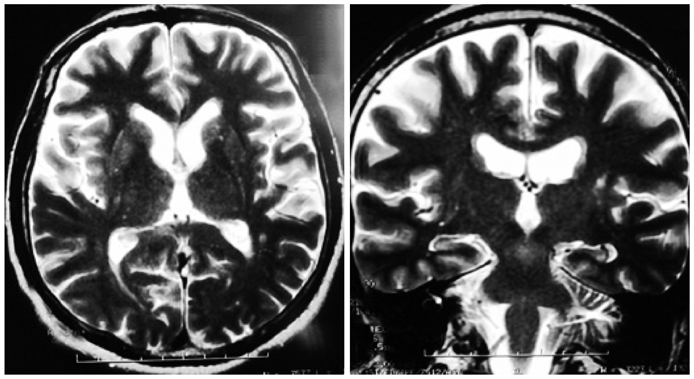
A 53-year-old male visited the outpatient clinic due to excessive gambling and personality changes. Based on electrophysiological findings and neuropsychiatric assessment, he was diagnosed as frontotemporal dementia-amyotrophic lateral sclerosis.
CONCLUSIONS
This case report underlines that PG can also be seen in patients with neurological disorders involving the orbitofrontal cortex.
MeSH Terms
Figure
Reference
-
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. 2000. 4th ed., text rev. Washington, D.C.: American Psychiatric Association.2. Black DW, Moyer T. Clinical features and psychiatric comorbidity of subjects with pathological gambling behavior. Psychiatr Serv. 1998. 49:1434–1439.
Article3. Dell'Osso B, Altamura AC, Allen A, Marazziti D, Hollander E. Epidemiologic and clinical updates on impulse control disorders: a critical review. Eur Arch Psychiatry Clin Neurosci. 2006. 256:464–475.4. Roy A, Adinoff B, Roehrich L, Lamparski D, Custer R, Lorenz V, et al. Pathological gambling. A psychobiological study. Arch Gen Psychiatry. 1988. 45:369–373.5. Cavedini P, Riboldi G, Keller R, D'Annucci A, Bellodi L. Frontal lobe dysfunction in pathological gambling patients. Biol Psychiatry. 2002. 51:334–341.
Article6. Voon V, Hassan K, Zurowski M, Duff-Canning S, de Souza M, Fox S, et al. Prospective prevalence of pathologic gambling and medication association in Parkinson disease. Neurology. 2006. 66:1750–1752.
Article7. Lo Coco D, Nacci P. Frontotemporal dementia presenting with pathological gambling. J Neuropsychiatry Clin Neurosci. 2004. 16:117–118.
Article8. Nakaaki S, Murata Y, Sato J, Shinagawa Y, Hongo J, Tatsumi H, et al. Impairment of decision-making cognition in a case of frontotemporal lobar degeneration (FTLD) presenting with pathologic gambling and hoarding as the initial symptoms. Cogn Behav Neurol. 2007. 20:121–125.
Article9. Manes FF, Torralva T, Roca M, Gleichgerrcht E, Bekinschtein TA, Hodges JR. Frontotemporal dementia presenting as pathological gambling. Nat Rev Neurol. 2010. 6:347–352.
Article10. McCullagh S, Moore M, Gawel M, Feinstein A. Pathological laughing and crying in amyotrophic lateral sclerosis: an association with prefrontal cognitive dysfunction. J Neurol Sci. 1999. 169:43–48.
Article11. Wicks P, MacPhee GJ. Pathological gambling amongst Parkinson's disease and ALS patients in an online community (PatientsLikeMe.com). Mov Disord. 2009. 24:1085–1088.
Article12. Irwin D, Lippa CF, Swearer JM. Cognition and amyotrophic lateral sclerosis (ALS). Am J Alzheimers Dis Other Demen. 2007. 22:300–312.
Article13. Gibbons ZC, Richardson A, Neary D, Snowden JS. Behaviour in amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2008. 9:67–74.
Article14. Brooks BR. Subcommittee on Motor Neuron Diseases/Amyotrophic Lateral Sclerosis of the World Federation of Neurology Research Group on Neuromuscular Diseases and the El Escorial "Clinical limits of amyotrophic lateral sclerosis" workshop contributors. El Escorial World Federation of Neurology criteria for the diagnosis of amyotrophic lateral sclerosis. J Neurol Sci. 1994. 124:Suppl. 96–107.
Article15. Güngen C, Ertan T, Eker E, Yaşar R, Engin F. Reliability and validity of the standardized Mini Mental State Examination in the diagnosis of mild dementia in Turkish population. Turk Psikiyatri Derg. 2002. 13:273–281.16. Can SS, Özel Kızıl ET, Varlı M, Turan E, Atlı T. Psychometric properties of the Turkish versions of three different clock drawing tests in patients with dementia. Arch Neuropsychiatry. 2010. 47:91–95.17. Dubois B, Slachevsky A, Litvan I, Pillon B. The FAB: a Frontal Assessment Battery at bedside. Neurology. 2000. 55:1621–1626.
Article18. Mavioglu H, Gedizlioglu M, Akyel S, Aslaner T, Eser E. The validity and reliability of the Turkish version of Alzheimer's Disease Assessment Scale-Cognitive Subscale (ADAS-Cog) in patients with mild and moderate Alzheimer's disease and normal subjects. Int J Geriatr Psychiatry. 2006. 21:259–265.
Article19. Cangöz B, Karakoç E, Selekler K. Trail Making Test: normative data for Turkish elderly population by age, sex and education. J Neurol Sci. 2009. 283:73–78.
Article20. Karakaş S. Handbook of BİLNOT Battery: Research and Development Studies for Neuropsychological Tests. 2006. 2nd ed. Ankara: Eryılmaz Ofset Matbaacılık Gazetecilik.21. Wechsler D. WAIS-R Manual: Wechsler Adult Intelligence Scale-Revised. 1981. New York: Psychological Corporation.22. Bechara A, Tranel D, Damasio H. Characterization of the decision-making deficit of patients with ventromedial prefrontal cortex lesions. Brain. 2000. 123:2189–2202.
Article23. Gregory C, Lough S, Stone V, Erzinclioglu S, Martin L, Baron-Cohen S, et al. Theory of mind in patients with frontal variant frontotemporal dementia and Alzheimer's disease: theoretical and practical implications. Brain. 2002. 125:752–764.
Article24. The ALS CNTF treatment study (ACTS) phase I-II Study Group. The Amyotrophic Lateral Sclerosis Functional Rating Scale. Assessment of activities of daily living in patients with amyotrophic lateral sclerosis. Arch Neurol. 1996. 53:141–147.25. Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998. 51:1546–1554.
Article26. Neary D, Snowden JS, Mann DM. Cognitive change in motor neurone disease/amyotrophic lateral sclerosis (MND/ALS). J Neurol Sci. 2000. 180:15–20.
Article27. Abrahams S, Leigh PN, Harvey A, Vythelingum GN, Grisé D, Goldstein LH. Verbal fluency and executive dysfunction in amyotrophic lateral sclerosis (ALS). Neuropsychologia. 2000. 38:734–747.
Article28. Strong MJ, Grace GM, Orange JB, Leeper HA, Menon RS, Aere C. A prospective study of cognitive impairment in ALS. Neurology. 1999. 53:1665–1670.
Article29. Grossman AB, Woolley-Levine S, Bradley WG, Miller RG. Detecting neurobehavioral changes in amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2007. 8:56–61.
Article30. Viskontas IV, Possin KL, Miller BL. Symptoms of frontotemporal dementia provide insights into orbitofrontal cortex function and social behavior. Ann N Y Acad Sci. 2007. 1121:528–545.
Article31. Perry RJ, Miller BL. Behavior and treatment in frontotemporal dementia. Neurology. 2001. 56:S46–S51.
Article32. Swartz JR, Miller BL, Lesser IM, Darby AL. Frontotemporal dementia: treatment response to serotonin selective reuptake inhibitors. J Clin Psychiatry. 1997. 58:212–216.33. Anneser JM, Jox RJ, Borasio GD. Inappropriate sexual behaviour in a case of ALS and FTD: successful treatment with sertraline. Amyotroph Lateral Scler. 2007. 8:189–190.
Article34. Blaszczynski A, Silove D. Pathological gambling: forensic issues. Aust N Z J Psychiatry. 1996. 30:358–369.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Pathogenetic Role of TAR DNA Binding Protein (TDP-43) in Amyotrophic Lateral Sclerosis and Frontotemporal Dementia
- Unstable Repeat Expansion in Neurodegenerative Dementias: Mechanisms of Disease
- Syndrome of Progressive Bulbar Palsy in Amyotrophic Lateral Sclerosis: A Case Report
- How predictive are temporal lobe changes of underlying TDP-43 pathology in the ALS-FTD continuum?
- Amyotrophic Lateral Sclerosis Associated With CADASIL