J Cardiovasc Ultrasound.
2014 Mar;22(1):1-5. 10.4250/jcu.2014.22.1.1.
Exercise Echocardiography in Asymptomatic Patients with Severe Aortic Stenosis and Preserved Left Ventricular Ejection Fraction
- Affiliations
-
- 1Department of Cardiology and Heart Valve Clinic, GIGA Cardiovascular Sciences, University of Liege, CHU Sart Tilman, Liege, Belgium. plancellotti@chu.ulg.ac.be
- KMID: 2177448
- DOI: http://doi.org/10.4250/jcu.2014.22.1.1
Abstract
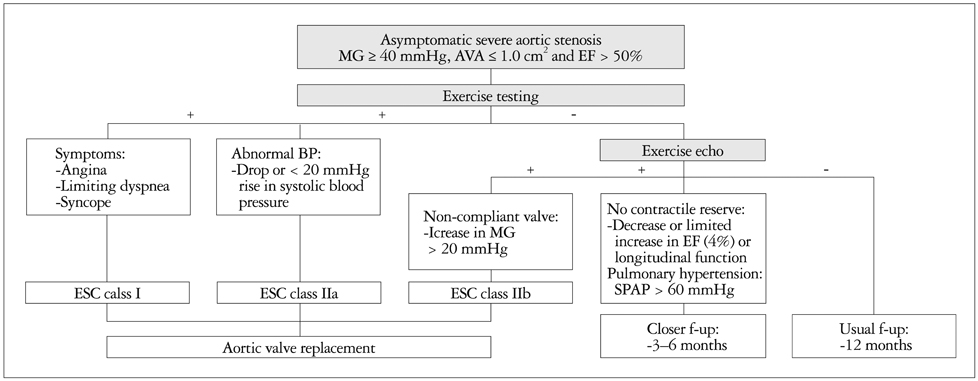
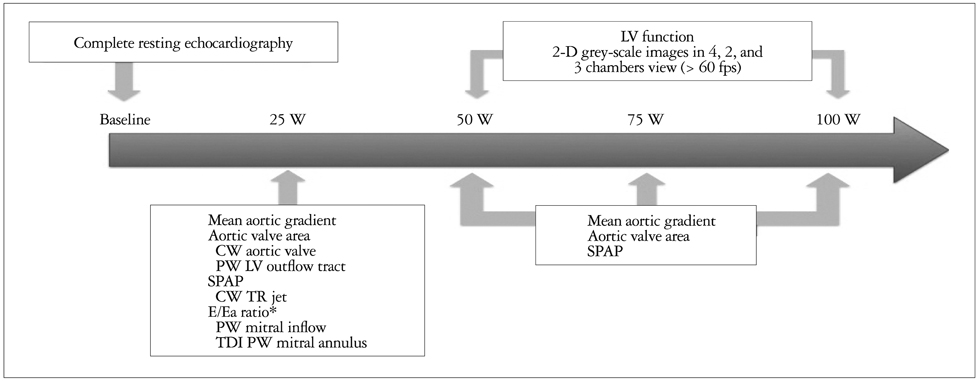
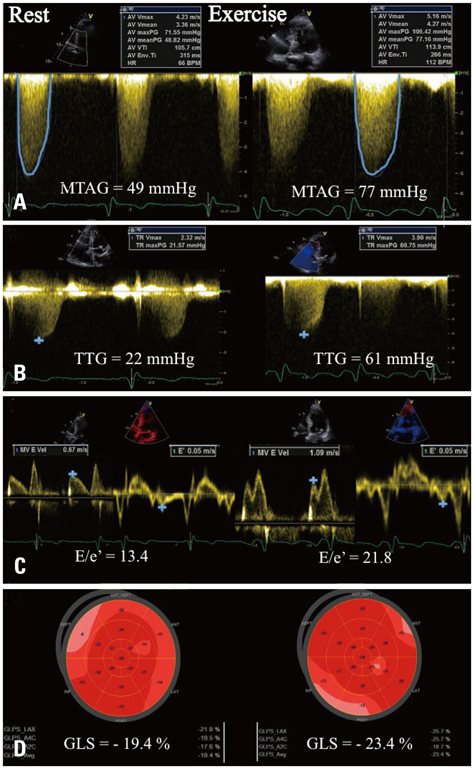
- The management of asymptomatic patients with severe aortic stenosis (AS) remains controversial. Recent series reported that early aortic valve replacement might be associated with improved clinical outcomes. However, the risk-benefit ratio should be carefully evaluated and early surgery only be proposed to a subset of asymptomatic patients considered at higher risk. Exercise echocardiography can help unmask symptomatic patients combined with assessment of the hemodynamic consequences of AS. Recent studies have demonstrated that exercise echocardiography can provide incremental prognostic value to identify patients who may benefit most from early surgery. In "truly" asymptomatic patients, an increase in mean aortic gradient > or = 18-20 mmHg, a limited left ventricular contractile reserve or a pulmonary hypertension during exercise are predictive parameters of adverse cardiac events. Exercise echocardiography is low-cost, safe and available in many referral centers, and does not expose patients to radiation. The purpose of this article is to describe the role of exercise testing and echocardiography in the management of asymptomatic patients with severe AS and preserved left ventricular ejection fraction.
MeSH Terms
Figure
Reference
-
1. Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, Tornos P, Vanoverschelde JL, Vermeer F, Boersma E, Ravaud P, Vahanian A. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J. 2003; 24:1231–1243.
Article2. Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC). European Association for Cardio-Thoracic Surgery (EACTS). Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, Borger MA, Carrel TP, De Bonis M, Evangelista A, Falk V, Iung B, Lancellotti P, Pierard L, Price S, Schäfers HJ, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppell UO, Windecker S, Zamorano JL, Zembala M. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012; 33:2451–2496.
Article3. Brown ML, Pellikka PA, Schaff HV, Scott CG, Mullany CJ, Sundt TM, Dearani JA, Daly RC, Orszulak TA. The benefits of early valve replacement in asymptomatic patients with severe aortic stenosis. J Thorac Cardiovasc Surg. 2008; 135:308–315.
Article4. Lancellotti P, Lebois F, Simon M, Tombeux C, Chauvel C, Pierard LA. Prognostic importance of quantitative exercise Doppler echocardiography in asymptomatic valvular aortic stenosis. Circulation. 2005; 112:9 Suppl. I377–I382.
Article5. Lancellotti P, Magne J, Donal E, O'Connor K, Dulgheru R, Rosca M, Pierard LA. Determinants and prognostic significance of exercise pulmonary hypertension in asymptomatic severe aortic stenosis. Circulation. 2012; 126:851–859.
Article6. Maréchaux S, Hachicha Z, Bellouin A, Dumesnil JG, Meimoun P, Pasquet A, Bergeron S, Arsenault M, Le Tourneau T, Ennezat PV, Pibarot P. Usefulness of exercise-stress echocardiography for risk stratification of true asymptomatic patients with aortic valve stenosis. Eur Heart J. 2010; 31:1390–1397.
Article7. Lancellotti P, Magne J, Piérard LA. The role of stress testing in evaluation of asymptomatic patients with aortic stenosis. Curr Opin Cardiol. 2013; 28:531–539.
Article8. Sicari R, Nihoyannopoulos P, Evangelista A, Kasprzak J, Lancellotti P, Poldermans D, Voigt JU, Zamorano JL. European Association of Echocardiography. Stress Echocardiography Expert Consensus Statement--Executive Summary: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur Heart J. 2009; 30:278–289.
Article9. Pellikka PA, Nagueh SF, Elhendy AA, Kuehl CA, Sawada SG. American Society of Echocardiography. American Society of Echocardiography recommendations for performance, interpretation, and application of stress echocardiography. J Am Soc Echocardiogr. 2007; 20:1021–1041.
Article10. Gibbons RJ, Balady GJ, Bricker JT, Chaitman BR, Fletcher GF, Froelicher VF, Mark DB, McCallister BD, Mooss AN, O'Reilly MG, Winters WL Jr, Gibbons RJ, Antman EM, Alpert JS, Faxon DP, Fuster V, Gregoratos G, Hiratzka LF, Jacobs AK, Russell RO, Smith SC Jr. American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation. 2002; 106:1883–1892.11. Picano E, Pibarot P, Lancellotti P, Monin JL, Bonow RO. The emerging role of exercise testing and stress echocardiography in valvular heart disease. J Am Coll Cardiol. 2009; 54:2251–2260.
Article12. Amato MC, Moffa PJ, Werner KE, Ramires JA. Treatment decision in asymptomatic aortic valve stenosis: role of exercise testing. Heart. 2001; 86:381–386.
Article13. Das P, Rimington H, Chambers J. Exercise testing to stratify risk in aortic stenosis. Eur Heart J. 2005; 26:1309–1313.
Article14. Rafique AM, Biner S, Ray I, Forrester JS, Tolstrup K, Siegel RJ. Meta-analysis of prognostic value of stress testing in patients with asymptomatic severe aortic stenosis. Am J Cardiol. 2009; 104:972–977.
Article15. Leurent G, Donal E, de Place C, Chabanne C, Gervais R, Fougerou C, le Helloco A, Daubert JC, Mabo P, Laurent M. Argument for a Doppler echocardiography during exercise in assessing asymptomatic patients with severe aortic stenosis. Eur J Echocardiogr. 2009; 10:69–73.
Article16. Lancellotti P, Karsera D, Tumminello G, Lebois F, Piérard LA. Determinants of an abnormal response to exercise in patients with asymptomatic valvular aortic stenosis. Eur J Echocardiogr. 2008; 9:338–343.
Article17. Maréchaux S, Ennezat PV, LeJemtel TH, Polge AS, de Groote P, Asseman P, Nevière R, Le Tourneau T, Deklunder G. Left ventricular response to exercise in aortic stenosis: an exercise echocardiographic study. Echocardiography. 2007; 24:955–959.
Article18. Lancellotti P, Donal E, Magne J, Moonen M, O'Connor K, Daubert JC, Pierard LA. Risk stratification in asymptomatic moderate to severe aortic stenosis: the importance of the valvular, arterial and ventricular interplay. Heart. 2010; 96:1364–1371.
Article19. Lafitte S, Perlant M, Reant P, Serri K, Douard H, DeMaria A, Roudaut R. Impact of impaired myocardial deformations on exercise tolerance and prognosis in patients with asymptomatic aortic stenosis. Eur J Echocardiogr. 2009; 10:414–419.
Article20. Lancellotti P, Moonen M, Magne J, O'Connor K, Cosyns B, Attena E, Donal E, Pierard L. Prognostic effect of long-axis left ventricular dysfunction and B-type natriuretic peptide levels in asymptomatic aortic stenosis. Am J Cardiol. 2010; 105:383–388.
Article21. Van Pelt NC, Stewart RA, Legget ME, Whalley GA, Wong SP, Zeng I, Oldfield M, Kerr AJ. Longitudinal left ventricular contractile dysfunction after exercise in aortic stenosis. Heart. 2007; 93:732–738.
Article22. Donal E, Thebault C, O'Connor K, Veillard D, Rosca M, Pierard L, Lancellotti P. Impact of aortic stenosis on longitudinal myocardial deformation during exercise. Eur J Echocardiogr. 2011; 12:235–241.
Article23. Bruch C, Stypmann J, Grude M, Gradaus R, Breithardt G, Wichter T. Tissue Doppler imaging in patients with moderate to severe aortic valve stenosis: clinical usefulness and diagnostic accuracy. Am Heart J. 2004; 148:696–702.
Article24. Burgess MI, Jenkins C, Sharman JE, Marwick TH. Diastolic stress echocardiography: hemodynamic validation and clinical significance of estimation of ventricular filling pressure with exercise. J Am Coll Cardiol. 2006; 47:1891–1900.
Article25. Grewal J, McCully RB, Kane GC, Lam C, Pellikka PA. Left ventricular function and exercise capacity. JAMA. 2009; 301:286–294.
Article26. Lancellotti P, Rosenhek R, Pibarot P, Iung B, Otto CM, Tornos P, Donal E, Prendergast B, Magne J, La Canna G, Piérard LA, Maurer G. ESC Working Group on Valvular Heart Disease position paper--heart valve clinics: organization, structure, and experiences. Eur Heart J. 2013; 34:1597–1606.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Transesophageal Echocardiography in the Diagnosis of Paradoxical Low Flow, Low Gradient Severe Aortic Stenosis
- Evaluation of Ejection Fraction Obtained by Echocardiography and Radionuclide Ventriculography
- Evaluation of Diastolic Dysfunction and the Role Thereof in Heart Failure with Preserved Ejection Fraction
- Exercise Echocardiography in Patients with Chronic Aortic Regurgitation: A Serial Echocardiographic and Clinical Follow-up Study
- Correlation of Left Ventricular Ejection Fraction Measured by Echocardiography and Contrast Cineangiography