Efficacy and Safety of Long-Term Thiopurine Maintenance Treatment in Japanese Patients With Ulcerative Colitis
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Graduate School of Medicine, Kyoto University, Kyoto, Japan. hiropy_n@kuhp.kyoto-u.ac.jp
- 2The Third Department of Internal Medicine, Kansai Medical University, Osaka, Japan.
- KMID: 2174476
- DOI: http://doi.org/10.5217/ir.2015.13.3.250
Abstract
- BACKGROUND/AIMS
The long-term clinical outcomes of patients with bio-naive ulcerative colitis (UC) who maintain remission with thiopurine are unclear. The aim of this study was to assess the long-term efficacy and safety of maintenance treatment with thiopurine in UC patients.
METHODS
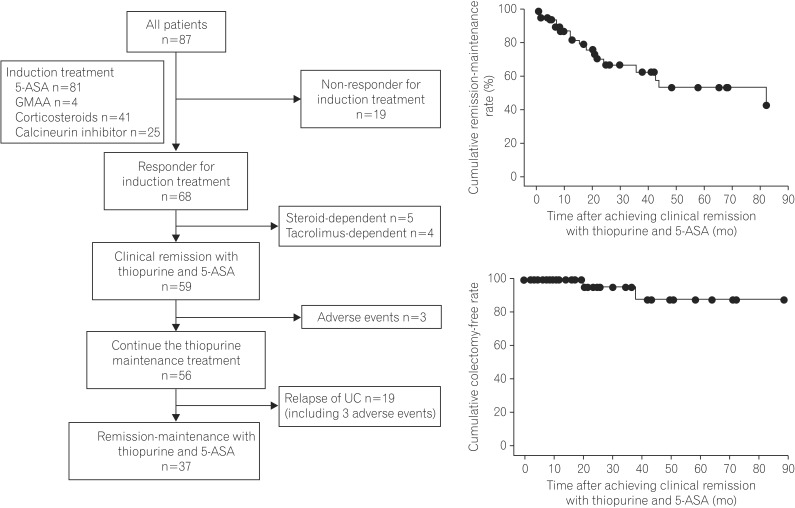
This was a retrospective observational cohort analysis conducted at a single center. Between December 1998 and August 2013, 59 of 87 patients with bio-naive UC who achieved remission after induction with treatments other than biologics were enrolled. Remission maintenance with thiopurine was defined as no concomitant treatment needed other than 5-aminosalicylate without relapse. We assessed the remission-maintenance rate, mucosal healing rate, colectomy-free rate, and treatment safety in UC patients who received thiopurine as maintenance treatment.
RESULTS
The 84-month cumulative remission-maintenance and colectomy-free survival rates in the UC patients who were receiving maintenance treatment with thiopurine and 5-aminosalicylate were 43.9% and 88.0%, respectively. Of the 38 patients who underwent colonoscopy during thiopurine maintenance treatment, 23 (60.5%) achieved mucosal healing. Of the 59 patients who achieved clinical remission with thiopurine, 6 patients (10.2%) discontinued the thiopurine therapy because of adverse events.
CONCLUSIONS
Our study demonstrates the long-term efficacy and safety of thiopurine treatment in patients with bio-naive UC.
MeSH Terms
Figure
Cited by 3 articles
-
Clinical Efficacy of Beclomethasone Dipropionate in Korean Patients with Ulcerative Colitis
Yoon Jee Lee, Jae Hee Cheon, Jae Hyun Kim, SunHo Yoo, Hyun Jung Lee, Soo Jung Park, Sung Pil Hong, Tae Il Kim, Won Ho Kim
Yonsei Med J. 2017;58(1):144-149. doi: 10.3349/ymj.2017.58.1.144.NUDT15 ,FTO , andRUNX1 genetic variants and thiopurine intolerance among Japanese patients with inflammatory bowel diseases
Toshiyuki Sato, Tetsuya Takagawa, Yoichi Kakuta, Akihiro Nishio, Mikio Kawai, Koji Kamikozuru, Yoko Yokoyama, Yuko Kita, Takako Miyazaki, Masaki Iimuro, Nobuyuki Hida, Kazutoshi Hori, Hiroki Ikeuchi, Shiro Nakamura
Intest Res. 2017;15(3):328-337. doi: 10.5217/ir.2017.15.3.328.Is Long-Term Therapy With Thiopurines Effective for Maintaining Remission in Patients With Moderate-To-Severe Ulcerative Colitis?
Seong Ran Jeon, Won Ho Kim
Intest Res. 2015;13(3):191-192. doi: 10.5217/ir.2015.13.3.191.
Reference
-
1. MacDermott RP, Stenson WF. Alterations of the immune system in ulcerative colitis and Crohn's disease. Adv Immunol. 1988; 42:285–328. PMID: 3284291.
Article2. Monteleone I, Vavassori P, Biancone L, Monteleone G, Pallone F. Immunoregulation in the gut: success and failures in human disease. Gut. 2002; 50(Suppl 3):III60–III64. PMID: 11953335.
Article3. Hanauer SB. Review article: evolving concepts in treatment and disease modification in ulcerative colitis. Aliment Pharmacol Ther. 2008; 27(Suppl 1):15–21. PMID: 18307645.
Article4. Sutherland LR, Martin F, Bailey RJ, et al. The Canadian Mesalamine for Remission of Crohn's Disease Study Group. A randomized, placebo-controlled, double-blind trial of mesalamine in the maintenance of remission of Crohn's disease. Gastroenterology. 1997; 112:1069–1077. PMID: 9097988.
Article5. Kozuch PL, Hanauer SB. Treatment of inflammatory bowel disease: a review of medical therapy. World J Gastroenterol. 2008; 14:354–377. PMID: 18200659.
Article6. Carter MJ, Lobo AJ, Travis SP. IBD Section, British Society of Gastroenterology. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004; 53(Suppl 5):V1–V16. PMID: 15306569.
Article7. Irving PM, Gearry RB, Sparrow MP, Gibson PR. Review article: appropriate use of corticosteroids in Crohn's disease. Aliment Pharmacol Ther. 2007; 26:313–329. PMID: 17635367.
Article8. Faubion WA Jr, Loftus EV Jr, Harmsen WS, Zinsmeister AR, Sandborn WJ. The natural history of corticosteroid therapy for inflammatory bowel disease: a population-based study. Gastroenterology. 2001; 121:255–260. PMID: 11487534.
Article9. Costantino G, Furfaro F, Belvedere A, Alibrandi A, Fries W. Thiopurine treatment in inflammatory bowel disease: response predictors, safety, and withdrawal in follow-up. J Crohns Colitis. 2012; 6:588–596. PMID: 22398045.
Article10. Chebli LA, Chaves LD, Pimentel FF, et al. Azathioprine maintains long-term steroid-free remission through 3 years in patients with steroid-dependent ulcerative colitis. Inflamm Bowel Dis. 2010; 16:613–619. PMID: 19705415.
Article11. Ardizzone S, Maconi G, Russo A, Imbesi V, Colombo E, Bianchi Porro G. Randomised controlled trial of azathioprine and 5-aminosalicylic acid for treatment of steroid dependent ulcerative colitis. Gut. 2006; 55:47–53. PMID: 15972298.
Article12. Timmer A, McDonald JW, Macdonald JK. Azathioprine and 6-mercaptopurine for maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev. 2007; CD000478. DOI: 10.1002/14651858.CD000478.pub2. Published online 24 January 2007. PMID: 17253451.
Article13. Rutgeerts P, Sandborn WJ, Feagan BG, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005; 353:2462–2476. PMID: 16339095.
Article14. Probert CS, Hearing SD, Schreiber S, et al. Infliximab in moderately severe glucocorticoid resistant ulcerative colitis: a randomised controlled trial. Gut. 2003; 52:998–1002. PMID: 12801957.
Article15. Reinisch W, Sandborn WJ, Hommes DW, et al. Adalimumab for induction of clinical remission in moderately to severely active ulcerative colitis: results of a randomised controlled trial. Gut. 2011; 60:780–787. PMID: 21209123.
Article16. Sandborn WJ, van Assche G, Reinisch W, et al. Adalimumab induces and maintains clinical remission in patients with moderate-to-severe ulcerative colitis. Gastroenterology. 2012; 142:257–265. PMID: 22062358.
Article17. Stidham RW, Lee TC, Higgins PD, et al. Systematic review with network meta-analysis: the efficacy of anti-tumour necrosis factor-alpha agents for the treatment of ulcerative colitis. Aliment Pharmacol Ther. 2014; 39:660–671. PMID: 24506179.
Article18. Sandborn WJ, Feagan BG, Marano C, et al. Subcutaneous golimumab induces clinical response and remission in patients with moderate-to-severe ulcerative colitis. Gastroenterology. 2014; 146:85–95. PMID: 23735746.
Article19. Sandborn WJ, Feagan BG, Marano C, et al. Subcutaneous golimumab maintains clinical response in patients with moderate-to-severe ulcerative colitis. Gastroenterology. 2014; 146:96–109. PMID: 23770005.
Article20. Dretzke J, Edlin R, Round J, et al. A systematic review and economic evaluation of the use of tumour necrosis factor-alpha (TNF-alpha) inhibitors, adalimumab and infliximab, for Crohn's disease. Health Technol Assess. 2011; 15:1–244. PMID: 21291629.21. Ford AC, Peyrin-Biroulet L. Opportunistic infections with anti-tumor necrosis factor-alpha therapy in inflammatory bowel disease: meta-analysis of randomized controlled trials. Am J Gastroenterol. 2013; 108:1268–1276. PMID: 23649185.
Article22. Lichtiger S, Present DH, Kornbluth A, et al. Cyclosporine in severe ulcerative colitis refractory to steroid therapy. N Engl J Med. 1994; 330:1841–1845. PMID: 8196726.
Article23. Yamamoto S, Nakase H, Mikami S, et al. Long-term effect of tacrolimus therapy in patients with refractory ulcerative colitis. Aliment Pharmacol Ther. 2008; 28:589–597. PMID: 18549460.
Article24. Laharie D, Bourreille A, Branche J, et al. Ciclosporin versus infliximab in patients with severe ulcerative colitis refractory to intravenous steroids: a parallel, open-label randomised controlled trial. Lancet. 2012; 380:1909–1915. PMID: 23063316.
Article25. Gisbert JP, Linares PM, McNicholl AG, Maté J, GomollÓn F. Meta-analysis: the efficacy of azathioprine and mercaptopurine in ulcerative colitis. Aliment Pharmacol Ther. 2009; 30:126–137. PMID: 19392869.
Article26. Khan KJ, Dubinsky MC, Ford AC, Ullman TA, Talley NJ, Moayyedi P. Efficacy of immunosuppressive therapy for inflammatory bowel disease: a systematic review and meta-analysis. Am J Gastroenterol. 2011; 106:630–642. PMID: 21407186.
Article27. Nguyen TV, Vu DH, Nguyen TM, Lachaux A, Boulieu R. Exploring associations of 6-thioguanine nucleotide levels and other predictive factors with therapeutic response to azathioprine in pediatric patients with IBD using multilevel analysis. Inflamm Bowel Dis. 2013; 19:2404–2410. PMID: 24013359.
Article28. LÓpez-Palacios N, Mendoza JL, Taxonera C, Lana R, LÓpez-Jamar JM, Díaz-Rubio M. Mucosal healing for predicting clinical outcome in patients with ulcerative colitis using thiopurines in monotherapy. Eur J Intern Med. 2011; 22:621–625. PMID: 22075292.
Article29. Dave M, Loftus EV Jr. Mucosal healing in inflammatory bowel disease-a true paradigm of success? Gastroenterol Hepatol (N Y). 2012; 8:29–38. PMID: 22347830.30. Rosenberg L, Nanda KS, Zenlea T, et al. Histologic markers of inflammation in patients with ulcerative colitis in clinical remission. Clin Gastroenterol Hepatol. 2013; 11:991–996. PMID: 23591275.
Article31. Solem CA, Loftus EV Jr, Tremaine WJ, Harmsen WS, Zinsmeister AR, Sandborn WJ. Correlation of C-reactive protein with clinical, endoscopic, histologic, and radiographic activity in inflammatory bowel disease. Inflamm Bowel Dis. 2005; 11:707–712. PMID: 16043984.
Article32. Schoepfer AM, Beglinger C, Straumann A, Trummler M, Renzulli P, Seibold F. Ulcerative colitis: correlation of the Rachmilewitz endoscopic activity index with fecal calprotectin, clinical activity, C-reactive protein, and blood leukocytes. Inflamm Bowel Dis. 2009; 15:1851–1858. PMID: 19462421.33. Schreiber S, Nikolaus S, Hampe J. Activation of nuclear factor kappa B inflammatory bowel disease. Gut. 1998; 42:477–484. PMID: 9616307.
Article34. Chaparro M, Ordás I, Cabré E, et al. Safety of thiopurine therapy in inflammatory bowel disease: long-term follow-up study of 3931 patients. Inflamm Bowel Dis. 2013; 19:1404–1410. PMID: 23665964.35. Qasim A, McDonald S, Sebastian S, et al. Efficacy and safety of 6-thioguanine in the management of inflammatory bowel disease. Scand J Gastroenterol. 2007; 42:194–199. PMID: 17327939.
Article36. Khan N, Abbas AM, Lichtenstein GR, Loftus EV Jr, Bazzano LA. Risk of lymphoma in patients with ulcerative colitis treated with thiopurines: a nationwide retrospective cohort study. Gastroenterology. 2013; 145:1007–1015. PMID: 23891975.
Article37. Beaugerie L, Brousse N, Bouvier AM, et al. Lymphoproliferative disorders in patients receiving thiopurines for inflammatory bowel disease: a prospective observational cohort study. Lancet. 2009; 374:1617–1625. PMID: 19837455.
Article38. Travis SP, Stange EF, Lémann M, et al. European evidence-based consensus on the management of ulcerative colitis: current management. J Crohns Colitis. 2008; 2:24–62. PMID: 21172195.
Article39. Roblin X, Peyrin-Biroulet L, Phelip JM, Nancey S, Flourie B. A 6-thioguanine nucleotide threshold level of 400 pmol/8 x 10(8) erythrocytes predicts azathioprine refractoriness in patients with inflammatory bowel disease and normal TPMT activity. Am J Gastroenterol. 2008; 103:3115–3122. PMID: 19086961.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Golimumab Therapy in Ulcerative Colitis
- Long-term efficacy and safety of tofacitinib in patients with ulcerative colitis: 3-year results from a real-world study
- Long-term efficacy and tolerability of dose-adjusted thiopurine treatment in maintaining remission in inflammatory bowel disease patients with NUDT15 heterozygosity
- Malignant change of chronic ulcerative colitis : report of a case
- Efficacy and safety of mirikizumab as induction and maintenance therapy for Japanese patients with moderately to severely active ulcerative colitis: a subgroup analysis of the global phase 3 LUCENT-1 and LUCENT-2 studies