J Gynecol Oncol.
2008 Sep;19(3):191-194. 10.3802/jgo.2008.19.3.191.
Validation of a nomogram for predicting outcome of vulvar cancer patients, primarily treated by surgery, in Korean population: multicenter retrospective study through Korean Gynecologic Oncology Group (KGOG-1010)
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Seoul National University Hospital, Korea. kjwksh@snu.ac.kr
- 2Department of Obstetrics and Gynecology, East-West Neo Medical Center, Korea.
- 3Department of Obstetrics and Gynecology, Korea University Ansan Hospital, Korea.
- 4Department of Obstetrics and Gynecology, Dong-A University Medical Center, Korea.
- 5Department of Obstetrics and Gynecology, Samsung Seoul Hospital, Korea.
- 6Department of Obstetrics and Gynecology, College of Medicine, Kwandong University, Cheil General Hospital & Women's Healthcare Center, Korea.
- 7Department of Obstetrics and Gynecology, Severance Hospital, Korea.
- 8Department of Obstetrics and Gynecology, Yongdong Severance Hospital, Korea.
- 9Department of Obstetrics and Gynecology, Inha University Hospital, Korea.
- 10Department of Obstetrics and Gynecology, Korea Cancer Center Hospital, Korea.
- 11Department of Obstetrics and Gynecology, Kosin University Gospel Hospital, Korea.
- 12Department of Obstetrics and Gynecology, Asan Medical Center, Korea.
- 13Department of Obstetrics and Gynecology, Hanyang University Hospital, Korea.
- KMID: 2173401
- DOI: http://doi.org/10.3802/jgo.2008.19.3.191
Abstract
OBJECTIVE
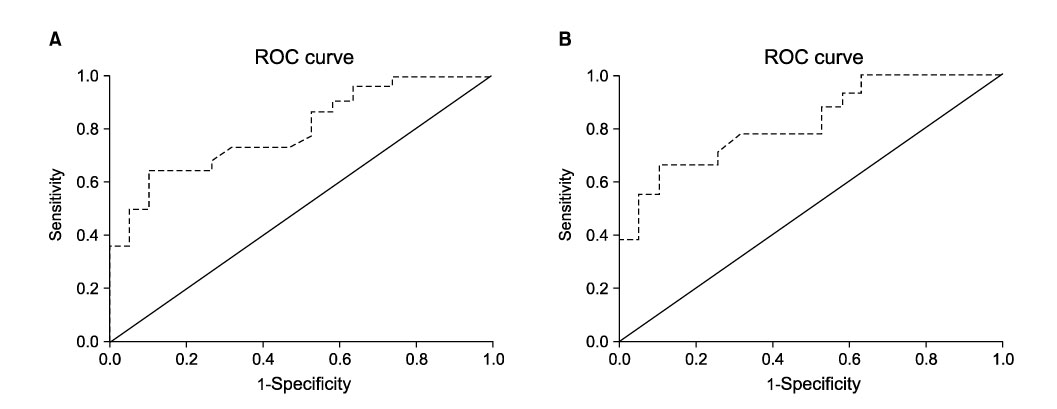
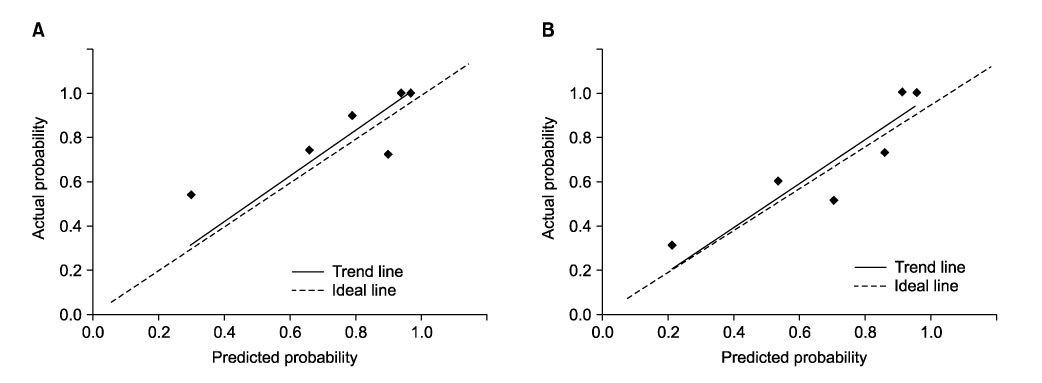
Regarding vulvar cancer, a nomogram has been suggested for the prediction of relapse-free survival (RFS). While the nomogram has been developed and validated in a Western study, there was no validation in Korean population. Thus, we have undertaken the study to assess the applicability of nomogram for predicting RFS in Korean patients with vulvar cancer. METHODS: A total of 204 cases newly diagnosed as vulvar cancer between 1982 and 2006 were identified. Among them 70 cases were not eligible due to inappropriate cell type (40 cases) and radiation as primary therapy (30 cases). Forty-four cases were not evaluable due to inadequate data and persistent disease. Finally a total of 90 patients primarily treated by surgery were included for analysis. Variables including age and the characteristics of primary tumor, nodal status, and surgical margin were collected for predicting RFS based on nomogram, which was compared with actual RFS. A calibration plot was drawn showing the actual versus predicted probability for 6 groups of patients segregated according to their predicted probabilities. In addition, discrimination of the nomogram was quantified with the concordance index. RESULTS: Patients' mean age was 58 years and mean follow-up period was 47.9 months. Observed 2y- and 5y-RFS rates were 81% and 68%, respectively, corresponding to 79% and 72% in the original cohort. The trend line in calibration plot showed comparable concordance with an ideal line, having a slope of 1.04 for 2y-RFS (R(2)=.35) and 0.98 for 5y-RFS (R2=.80), respectively. The concordance index was 0.79 in the KGOG data set, which was improved to 0.82 with the data set limited to squamous cell carcinoma. CONCLUSION: The nomogram provides the predictive capacity for relapse-free survival in Korean patients with vulvar cancer.
Keyword
MeSH Terms
Figure
Reference
-
1. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008. 58:71–96.2. Beller U, Quinn MA, Benedet JL, Creasman WT, Ngan HY, Maisonneuve P, et al. Carcinoma of the vulva. FIGO 6th annual report on the results of treatment in gynecological cancer. Int J Gynaecol Obstet. 2006. 95:Suppl 1. S7–S27.3. Eastham JA, Kattan MW, Scardino PT. Nomograms as predictive models. Semin Urol Oncol. 2002. 20:108–115.4. Stephenson AJ, Scardino PT, Eastham JA, Bianco FJ Jr, Dotan ZA, DiBlasio CJ, et al. Postoperative nomogram predicting the 10-year probability of prostate cancer recurrence after radical prostatectomy. J Clin Oncol. 2005. 23:7005–7012.5. Kattan MW, Leung DH, Brennan MF. Postoperative nomogram for 12-year sarcoma-specific death. J Clin Oncol. 2002. 20:791–796.6. Van Zee KJ, Manasseh DM, Bevilacqua JL, Boolbol SK, Fey JV, Tan LK, et al. A nomogram for predicting the likelihood of additional nodal metastases in breast cancer patients with a positive sentinel node biopsy. Ann Surg Oncol. 2003. 10:1140–1151.7. Rouzier R, Preti M, Haddad B, Martin M, Micheletti L, Paniel BJ. Development and validation of a nomogram for predicting outcome of patients with vulvar cancer. Obstet Gynecol. 2006. 107:672–677.8. Hopkins MP, Reid GC, Vettrano I, Morley GW. Squamous cell carcinoma of the vulva: prognostic factors influencing survival. Gynecol Oncol. 1991. 43:113–117.9. Homesley HD, Bundy BN, Sedlis A, Yordan E, Berek JS, Jahshan A, et al. Assessment of current International Federation of Gynecology and Obstetrics staging of vulvar carcinoma relative to prognostic factors for survival (a Gynecologic Oncology Group study). Am J Obstet Gynecol. 1991. 164:997–1003.10. Heaps JM, Fu YS, Montz FJ, Hacker NF, Berek JS. Surgical-pathologic variables predictive of local recurrence in squamous cell carcinoma of the vulva. Gynecol Oncol. 1990. 38:309–314.11. Ghurani GB, Penalver MA. An update on vulvar cancer. Am J Obstet Gynecol. 2001. 185:294–299.12. International Federation of Gynecology and Obstetrics (FIGO). Changes in gynecologic cancer staging by the International Federation of Gynecology and Obstetrics. Am J Obstet Gynecol. 1990. 162:610–611.13. Rouzier R, Preti M, Sideri M, Paniel BJ, Jones RW. A suggested modification to FIGO stage III vulvar cancer. Gynecol Oncol. 2008. 110:83–86.14. Homesley HD, Bundy BN, Sedlis A, Yordan E, Berek JS, Jahshan A, et al. Prognostic factors for groin node metastasis in squamous cell carcinoma of the vulva (a Gynecologic Oncology Group study). Gynecol Oncol. 1993. 49:279–283.15. Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008. 26:1364–1370.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hospital volume-outcome relationship in vulvar cancer treatment: a Japanese Gynecologic Oncology Group study
- Epidemiologic characteristics and a prognostic nomogram for patients with vulvar cancer: results from the Surveillance, Epidemiology, and End Results (SEER) program in the United States, 1975 to 2016
- Pregnancy following vulvar squamous cell carcinoma: a report of two cases
- The age-adjusted Charlson comorbidity index as a predictor of survival in surgically treated vulvar cancer patients
- A single-arm, phase II study of niraparib and bevacizumab maintenance therapy in platinum-sensitive, recurrent ovarian cancer patients previously treated with a PARP inhibitor: Korean Gynecologic Oncology Group (KGOG 3056)/NIRVANA-R trial