Ann Dermatol.
2011 Dec;23(Suppl 3):S375-S379. 10.5021/ad.2011.23.S3.S375.
The Co-Existence of Vulvar Lichen Sclerosus, Ulcerated Calcinosis Cutis, and Dermatomyositis: Coincidence or Immunological Mechanism?
- Affiliations
-
- 1Department of Dermatology, Faculty of Medicine, Mustafa Kemal University, Antakya-Hatay, Turkey. didemaltiner@yahoo.com
- 2Department of Pathology, Faculty of Medicine, Mustafa Kemal University, Antakya-Hatay, Turkey.
- KMID: 2171876
- DOI: http://doi.org/10.5021/ad.2011.23.S3.S375
Abstract
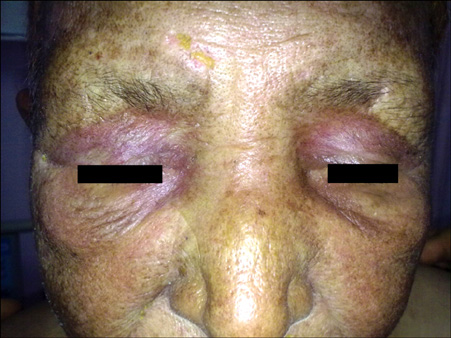
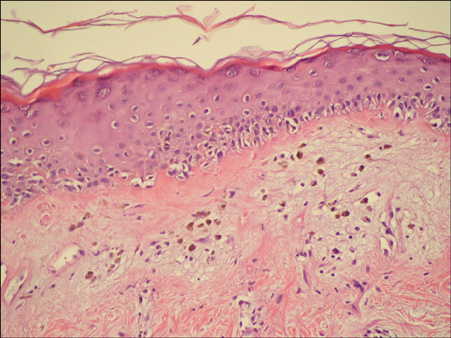
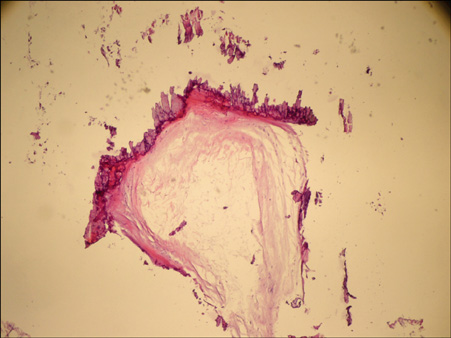
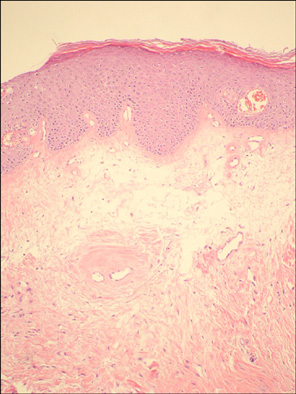
- Calcinosis cutis is a condition characterized by the deposition of calcium salts in the skin and subcutaneous tissues, and patients suffering from it encounter various connective tissue disorders, such as dermatomyositis (DM), scleroderma, and systemic lupus erythematosus. Although calcinosis cutis is frequently accompanied by juvenile dermatomyositis, rare cases have been reported in adult patients with DM. On the other hand, lichen sclerosus (LS) is a chronic inflammatory disease of the skin and mucosal surfaces. In the present report, we present a rare case of a 71-year-old patient with DM accompanied by ulcerated calcinosis cutis and vulvar LS.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Tumoral Calcinosis as an Initial Complaint of Juvenile-Onset Amyopathic Dermatomyositis
Eun Jin Doh, Jungyoon Moon, Sue Shin, Soo Hyun Seo, Hyun Sun Park, Hyun-Sun Yoon, Soyun Cho
Ann Dermatol. 2016;28(3):375-380. doi: 10.5021/ad.2016.28.3.375.
Reference
-
1. Jorizzo JL, Carroll CL, Sangueza OP. Bolognia JL, Jorizzo JL, Rapine RP, editors. Dermatomyositis. Dermatology. 2008. 2nd ed. Spain: Mosby Elsevier;575–583.
Article2. Sontheimer RD, Costner MI. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Dermatomyositis. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw Hill;1536–1553.3. Dalakas MC. Polymyositis, dermatomyositis and inclusion-body myositis. N Engl J Med. 1991. 325:1487–1498.
Article4. Callen JP. Dermatomyositis. Lancet. 2000. 355:53–57.
Article5. Hill CL, Zhang Y, Sigurgeirsson B, Pukkala E, Mellemkjaer L, Airio A, et al. Frequency of specific cancer types in dermatomyositis and polymyositis: a population-based study. Lancet. 2001. 357:96–100.
Article6. Smith YR, Haefner HK. Vulvar lichen sclerosus : pathophysiology and treatment. Am J Clin Dermatol. 2004. 5:105–125.7. Hengge UR. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Lichen sclerosus. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw Hill;546–550.8. Touart DM, Sau P. Cutaneous deposition diseases. Part II. J Am Acad Dermatol. 1998. 39:527–544.
Article9. Boulman N, Slobodin G, Rozenbaum M, Rosner I. Calcinosis in rheumatic diseases. Semin Arthritis Rheum. 2005. 34:805–812.
Article10. Lobo IM, Machado S, Teixeira M, Selores M. Calcinosis cutis: a rare feature of adult dermatomyositis. Dermatol Online J. 2008. 14:10.
Article11. Muller SA, Winkelmann RK, Brunsting LA. Calcinosis in dermatomyositis; observations on course of disease in children and adults. AMA Arch Derm. 1959. 79:669–673.12. Kavala M, Sudogan S, Can B, Zindanci I, Kuru I, Beyhan S, et al. An extremely severe case of cutaneous calcinosis complicating adult dermatomyositis. Clin Exp Dermatol. 2009. 34:115–116.
Article13. Abdallah-Lotf M, Grasland A, Vinceneux P, Sigal-Grinberg M. Regression of cutis calcinosis with diltiazem in adult dermatomyositis. Eur J Dermatol. 2005. 15:102–104.14. Olhoffer IH, Carroll C, Watsky K. Dermatomyositis sine myositis presenting with calcinosis universalis. Br J Dermatol. 1999. 141:365–366.
Article15. Eddy MC, Leelawattana R, McAlister WH, Whyte MP. Calcinosis universalis complicating juvenile dermatomyositis: resolution during probenecid therapy. J Clin Endocrinol Metab. 1997. 82:3536–3542.
Article16. Bowyer SL, Blane CE, Sullivan DB, Cassidy JT. Childhood dermatomyositis: factors predicting functional outcome and development of dystrophic calcification. J Pediatr. 1983. 103:882–888.
Article17. Matsuoka Y, Miyajima S, Okada N. A case of calcinosis universalis successfully treated with low-dose warfarin. J Dermatol. 1998. 25:716–720.
Article18. Nakagawa T, Takaiwa T. Calcinosis cutis in juvenile dermatomyositis responsive to aluminum hydroxide treatment. J Dermatol. 1993. 20:558–560.
Article19. Vereecken P, Stallenberg B, Tas S, de Dobbeleer G, Heenen M. Ulcerated dystrophic calcinosis cutis secondary to localised linear scleroderma. Int J Clin Pract. 1998. 52:593–594.20. Vinen CS, Patel S, Bruckner FE. Regression of calcinosis associated with adult dermatomyositis following diltiazem therapy. Rheumatology (Oxford). 2000. 39:333–334.
Article21. Park JH, Lee CW. Concurrent development of dermatomyositis and morphoea profunda. Clin Exp Dermatol. 2002. 27:324–327.
Article22. Röcken M, Ghoreschi K. Bolognia JL, Jorizzo JL, Rapini RP, editors. Morphea and lichen sclerosus. Dermatology. 2008. 2nd ed. Spain: Mosby Elsevier;1469–1483.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Calcinosis Cutis Associated with Juvenile Dermatomyositis
- Three Cases of Vulvar Squamous Cell Carcinoma Arising from Lichen Sclerosus
- The Role of Nanofat Grafting in Vulvar Lichen Sclerosus: A Preliminary Report
- A Clinical and Histopathological Study of 25 Cases of Vulvar Lichen Sclerosus et Atrophicus
- A Case of Nodular Lichen Sclerosus