A Prospective, Long-Term Follow-Up Study of 1,444 nm Nd:YAG Laser: A New Modality for Treating Axillary Bromhidrosis
- Affiliations
-
- 1Department of Dermatology, Korea University College of Medicine, Seoul, Korea. kumcihk@korea.ac.kr
- KMID: 2171653
- DOI: http://doi.org/10.5021/ad.2014.26.2.184
Abstract
- BACKGROUND
Surgery for bromhidrosis has a high risk of complications such as hematoma and necrosis. New nonsurgical methods may reduce the burden on surgery and the risks for the patient.
OBJECTIVE
This study was performed to evaluate the efficacy and side-effects of the 1,444 nm Nd:YAG interstitial laser for treating axillary bromhidrosis.
METHODS
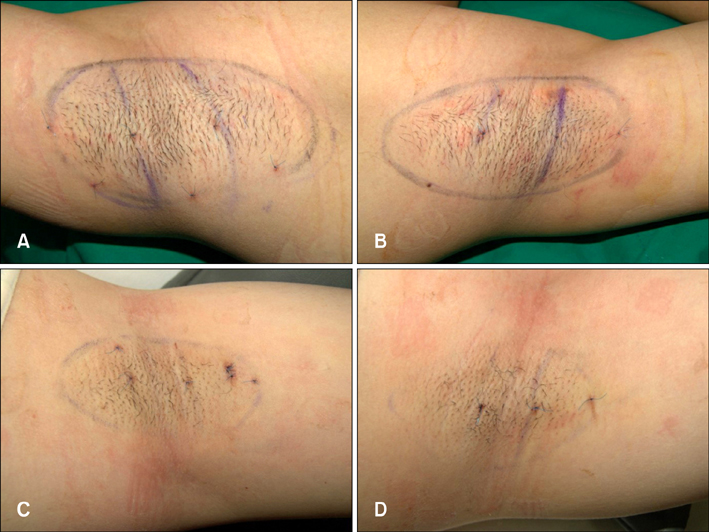
Eighteen bromhidrosis patients were treated with a 1,444 nm Nd:YAG laser at Korea University Ansan Hospital. The post-treatment follow-up was 6 months. After the procedure, we confirmed apocrine gland destruction through histopathological examination. At each follow-up, we measured the severity of the remaining odor, postoperative pain, degree of mobility restriction, and overall satisfaction.
RESULTS
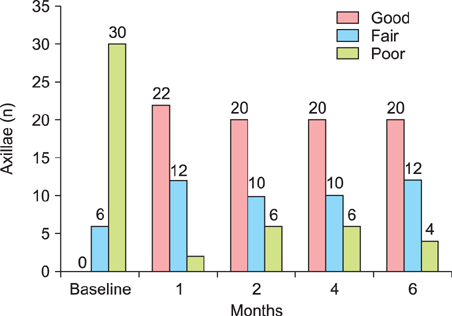
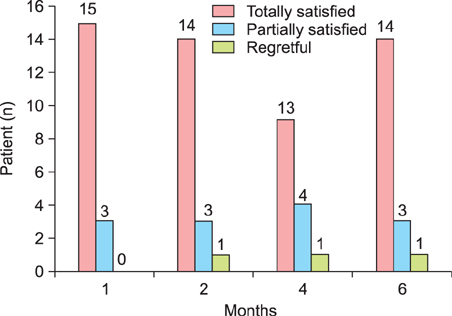
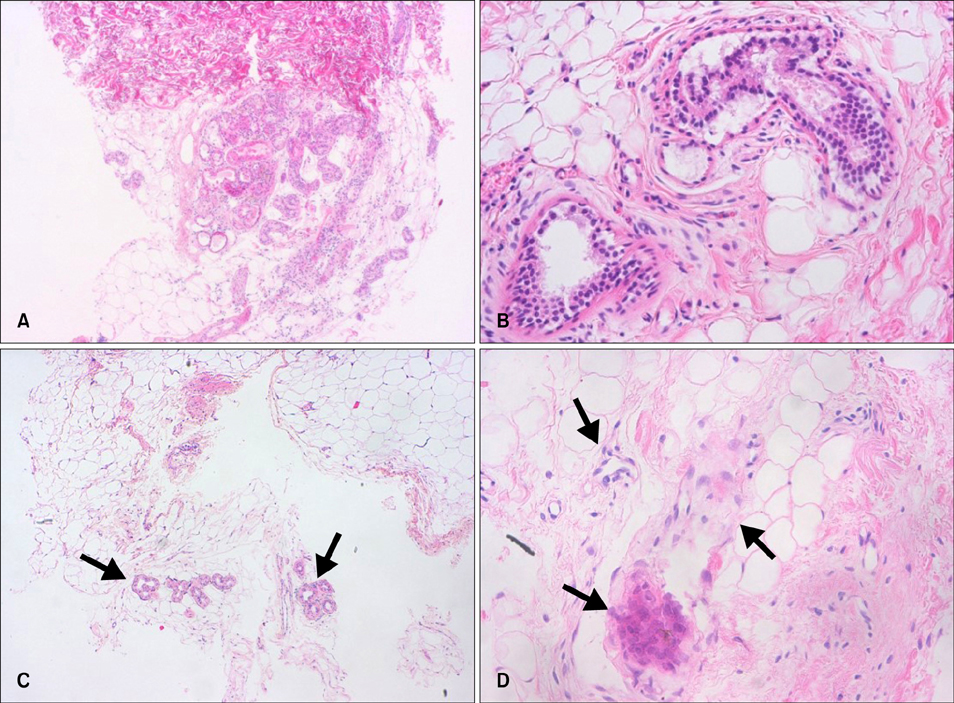
After 180 days of follow-up, malodor elimination was good in 20 axillae, fair in 12 axillae, and poor in four axillae. At the end point of the study, 14 patients were totally satisfied with the laser treatment, three patients were partially satisfied, and one patient was disatisfied. Pain and limitation of mobility were significantly reduced within 1 week post-operatively, and were almost resolved within 4 weeks post-operatively. A histopathological examination revealed decreased density and significant alterations to the apocrine glands.
CONCLUSION
Subdermal coagulation treatment with a 1,444 nm Nd:YAG interstitial laser may be a less invasive and effective therapy for axillary bromhidrosis.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Minimally Invasive Surgery for Axillary Osmidrosis Using a Combination of Subcutaneous Tissue Removal and a 1,444-nm Nd:YAG Laser
Sang Geun Lee, Hwa Jung Ryu, Il-Hwan Kim
Ann Dermatol. 2014;26(6):755-757. doi: 10.5021/ad.2014.26.6.755.Treatment of Diffuse Planar Xanthoma of the Face after One Session of 1,444-nm Neodymium-Doped Yttrium Aluminium Garnet Laser
Ji Min Lee, Seung Hyun Chun, Byoung Joon So, Min Gun Yoo, Sun Yae Kim, Il-Hwan Kim
Ann Dermatol. 2015;27(6):769-770. doi: 10.5021/ad.2015.27.6.769.Terminal Deoxynucleotidyl Transferase-Mediated Deoxyuridine Triphosphate Nick End Labeling (TUNEL) Assay to Characterize Histopathologic Changes Following Thermal Injury
Ji Min Lee, Ji Hyun Park, Bo Young Kim, Il-Hwan Kim
Ann Dermatol. 2018;30(1):41-46. doi: 10.5021/ad.2018.30.1.41.
Reference
-
1. Goldman A, Wollina U. Subdermal Nd-YAG laser for axillary hyperhidrosis. Dermatol Surg. 2008; 34:756–762.
Article2. Park YJ, Shin MS. What is the best method for treating osmidrosis? Ann Plast Surg. 2001; 47:303–309.
Article3. Khoury JG, Saluja R, Keel D, Detwiler S, Goldman MP. Histologic evaluation of interstitial lipolysis comparing a 1064, 1320 and 2100 nm laser in an ex vivo model. Lasers Surg Med. 2008; 40:402–406.
Article4. Tark KC, Jung JE, Song SY. Superior lipolytic effect of the 1,444 nm Nd:YAG laser: comparison with the 1,064 nm Nd:YAG laser. Lasers Surg Med. 2009; 41:721–727.
Article5. Ichikawa K, Miyasaka M, Aikawa Y. Subcutaneous laser treatment of axillary osmidrosis: a new technique. Plast Reconstr Surg. 2006; 118:170–174.
Article6. Qian JG, Wang XJ. Effectiveness and complications of subdermal excision of apocrine glands in 206 cases with axillary osmidrosis. J Plast Reconstr Aesthet Surg. 2010; 63:1003–1007.
Article7. Qian JG, Wang XJ. Radical treatment of axillary osmidrosis by subdermal excision of apocrine glands: a prospective study in 31 cases. J Plast Reconstr Aesthet Surg. 2006; 59:860–864.
Article8. Kim IH, Seo SL, Oh CH. Minimally invasive surgery for axillary osmidrosis: combined operation with CO2 laser and subcutaneous tissue remover. Dermatol Surg. 1999; 25:875–879.
Article9. Hong HC, Lupin M, O'Shaughnessy KF. Clinical evaluation of a microwave device for treating axillary hyperhidrosis. Dermatol Surg. 2012; 38:728–735.
Article10. Glaser DA, Coleman WP 3rd, Fan LK, Kaminer MS, Kilmer SL, Nossa R, et al. A randomized, blinded clinical evaluation of a novel microwave device for treating axillary hyperhidrosis: the dermatologic reduction in underarm perspiration study. Dermatol Surg. 2012; 38:185–191.
Article11. Perng CK, Yeh FL, Ma H, Lin JT, Hwang CH, Shen BH, et al. Is the treatment of axillary osmidrosis with liposuction better than open surgery? Plast Reconstr Surg. 2004; 114:93–97.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subdermal Coagulation Treatment of Axillary Bromhidrosis by 1,444 nm Nd:YAG Laser: A Comparison with Surgical Treatment
- Minimally Invasive Surgery for Axillary Osmidrosis Using a Combination of Subcutaneous Tissue Removal and a 1,444-nm Nd:YAG Laser
- Clinical Outcomes and Satisfaction with Laser Treatment and Surgery of Axillary Bromhidrosis Patients: A Retrospective Analysis
- 1,064 nm Long-Pulsed Nd:YAG Laser for the Treatment of Onychomycosis
- Post-acne Erythema Successfully Treated with 595-nm Picosecond-domain Neodymium:Yttrium-aluminum-garnet Laser