Imaging Sci Dent.
2012 Sep;42(3):169-174. 10.5624/isd.2012.42.3.169.
Osteoarthritic changes and condylar positioning of the temporomandibular joint in Korean children and adolescents
- Affiliations
-
- 1Department of Oral and Maxillofacial Radiology, School of Dentistry, Pusan National University, Yangsan, Korea. yhjung@pusan.ac.kr
- KMID: 2167435
- DOI: http://doi.org/10.5624/isd.2012.42.3.169
Abstract
- PURPOSE
To investigate the prevalence of osteoarthritic changes and condylar positioning of the temporomandibular joint (TMJ) in Korean children and adolescents with or without temporomandibular disorders (TMDs).
MATERIALS AND METHODS
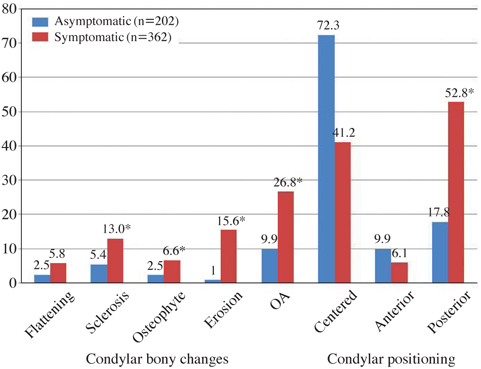
A total of 101 asymptomatic and 181 symptomatic children and adolescents aged 10 to 18 years old were included in the study. Osteoarthritic changes such as flattening, sclerosis, osteophytes, or erosion, and the parasagittal positioning of the condyle were assessed using cone-beam computed tomography (CBCT) images.
RESULTS
The overall prevalence of osteoarthritic changes was higher in symptomatic (26.8%) than in asymptomatic adolescents (9.9%) (p<0.05). In the symptomatic group, the frequency was higher in males (33.3%) than in females (23.0%) (p<0.05). Erosion was the most common change for the symptomatic group (15.6%), whereas sclerosis was the most common change for the asymptomatic group (5.4%). Posterior condylar position was more frequently observed in the symptomatic group (p<0.05). Erosion was more common in the samples with TMJ pain or mouth opening limitations as compared to those without them (p<0.05).
CONCLUSION
This study showed that osteoarthritic changes in TMJ were common in children and adolescents, with a much higher prevalence in symptomatic patients.
MeSH Terms
Figure
Cited by 1 articles
-
Nontraumatic bifid mandibular condyles in asymptomatic and symptomatic temporomandibular joint subjects
Bong-Hae Cho, Yun-Hoa Jung
Imaging Sci Dent. 2013;43(1):25-30. doi: 10.5624/isd.2013.43.1.25.
Reference
-
1. Poveda Roda R, Bagan JV, Díaz Fernández JM, Hernández Bazán S, Jiménez Soriano Y. Review of temporomandibular joint pathology. Part I: classification, epidemiology and risk factors. Med Oral Patol Oral Cir Bucal. 2007. 12:E292–E298.2. Dibbets JM, van der Weele LT. Prevalence of structural bony change in the mandibular condyle. J Craniomandib Disord. 1992. 6:254–259.3. Vanderas AP. Prevalence of craniomandibular dysfunction in children and adolescents: a review. Pediatr Dent. 1987. 9:312–316.4. Magnusson T, Egermark-Eriksson I, Carlsson GE. Four-year longitudinal study of mandibular dysfunction in children. Community Dent Oral Epidemiol. 1985. 13:117–120.
Article5. Gazit E, Lieberman M, Eini R, Hirsch N, Serfaty V, Fuchs C, et al. Prevalence of mandibular dysfunction in 10-18 year old Israeli schoolchildren. J Oral Rehabil. 1984. 11:307–317.
Article6. Ishibashi H, Takenoshita Y, Ishibashi K, Oka M. Age-related changes in the human mandibular condyle: a morphologic, radiologic, and histologic study. J Oral Maxillofac Surg. 1995. 53:1016–1024.7. Widmalm SE, Westesson PL, Kim IK, Pereira FJ Jr, Lundh H, Tasaki MM. Temporomandibular joint pathosis related to sex, age, and dentition in autopsy material. Oral Surg Oral Med Oral Pathol. 1994. 78:416–425.
Article8. Sanchez-Woodworth RE, Katzberg RW, Tallents RH, Guay JA. Radiographic assessment of temporomandibular joint pain and dysfunction in the pediatric age-group. ASDC J Dent Child. 1988. 55:278–281.9. Yamada K, Saito I, Hanada K, Hayashi T. Observation of three cases of temporomandibular joint osteoarthritis and mandibular morphology during adolescence using helical CT. J Oral Rehabil. 2004. 31:298–305.
Article10. Pullinger AG, Solberg WK, Hollender L, Guichet D. Tomographic analysis of mandibular condyle position in diagnostic subgroups of temporomandibular disorders. J Prosthet Dent. 1986. 55:723–729.
Article11. Pereira LJ, Gavião MB, Bonjardim LR, Castelo PM. Ultrasound and tomographic evaluation of temporomandibular joints in adolescents with and without signs and symptoms of temporomandibular disorders: a pilot study. Dentomaxillofac Radiol. 2007. 36:402–408.
Article12. Gateno J, Anderson PB, Xia JJ, Horng JC, Teichgraeber JF, Liebschner MA. A comparative assessment of mandibular condylar position in patients with anterior disc displacement of the temporomandibular joint. J Oral Maxillofac Surg. 2004. 62:39–43.
Article13. Bonilla-Aragon H, Tallents RH, Katzberg RW, Kyrkanides S, Moss ME. Condyle position as a predictor of temporomandibular joint internal derangement. J Prosthet Dent. 1999. 82:205–208.
Article14. Wiese M, Svensson P, Bakke M, List T, Hintze H, Petersson A, et al. Association between temporomandibular joint symptoms, signs, and clinical diagnosis using the RDC/TMD and radiographic findings in temporomandibular joint tomograms. J Orofac Pain. 2008. 22:239–251.15. Abdel-Fattah RA. Optimum temporomandibular joint (TMJ) condylar position. Todays FDA. 1989. 1:1C–3C.16. Robinson de Senna B, Marques LS, França JP, Ramos-Jorge ML, Pereira LJ. Condyle-disk-fossa position and relationship to clinical signs and symptoms of temporomandibular disorders in women. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009. 108:e117–e124.
Article17. Vasconcelos Filho JO, Menezes AV, Freitas DQ, Manzi FR, Bóscolo FN, de Almeida SM. Condylar and disk position and signs and symptoms of temporomandibular disorders in stress-free subjects. J Am Dent Assoc. 2007. 138:1251–1255.18. Katzberg RW, Keith DA, Ten Eick WR, Guralnick WC. Internal derangements of the temporomandibular joint: an assessment of condylar position in centric occlusion. J Prosthet Dent. 1983. 49:250–254.
Article19. Pullinger A, Hollender L. Variation in condyle-fossa relationships according to different methods of evaluation in tomograms. Oral Surg Oral Med Oral Pathol. 1986. 62:719–727.
Article20. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960. 20:37–46.
Article21. Alexiou K, Stamatakis H, Tsiklakis K. Evaluation of the severity of temporomandibular joint osteoarthritic changes related to age using cone beam computed tomography. Dentomaxillofac Radiol. 2009. 38:141–147.
Article22. Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol. 2004. 33:196–201.
Article23. Honey OB, Scarfe WC, Hilgers MJ, Klueber K, Silveira AM, Haskell BS, et al. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: comparisons with panoramic radiology and linear tomography. Am J Orthod Dentofacial Orthop. 2007. 132:429–438.
Article24. Takayama Y, Miura E, Yuasa M, Kobayashi K, Hosoi T. Comparison of occlusal condition and prevalence of bone change in the condyle of patients with and without temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008. 105:104–112.
Article25. Zhao YP, Zhang ZY, Wu YT, Zhang WL, Ma XC. Investigation of the clinical and radiographic features of osteoarthrosis of the temporomandibular joints in adolescents and young adults. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011. 111:e27–e34.
Article26. Petrikowski CG, Grace MG. Age and gender differences in temporomandibular joint radiographic findings before orthodontic treatment in adolescents. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999. 87:380–385.
Article27. Wiese M, Wenzel A, Hintze H, Petersson A, Knutsson K, Bakke M, et al. Osseous changes and condyle position in TMJ tomograms: impact of RDC/TMD clinical diagnoses on agreement between expected and actual findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008. 106:e52–e63.
Article28. Wiberg B, Wänman A. Signs of osteoarthrosis of the temporomandibular joints in young patients: a clinical and radiographic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998. 86:158–164.29. Hiltunen K, Peltola JS, Vehkalahti MM, Närhi T, Ainamo A. A 5-year follow-up of signs and symptoms of TMD and radiographic findings in the elderly. Int J Prosthodont. 2003. 16:631–634.30. Kurita H, Kojima Y, Nakatsuka A, Koike T, Kobayashi H, Kurashina K. Relationship between temporomandibular joint (TMJ)-related pain and morphological changes of the TMJ condyle in patients with temporomandibular disorders. Dentomaxillofac Radiol. 2004. 33:329–333.
Article31. Lee JU, Kim HS, Song JS, Kim KA, Koh KJ. Bone change of mandibular condyle using cone beam computed tomography. Korean J Oral Maxillofac Radiol. 2007. 37:139–147.32. Ren YF, Isberg A, Westesson PL. Condyle position in the temporomandibular joint. Comparison between asymptomatic volunteers with normal disk position and patients with disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995. 80:101–107.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The positional change of condylar head after orthognathic surgery using simplified condyle positioning device
- Condylar Hyperplasia with Long-standing Temporomandibular Joint Dislocation
- A comparative study on the standard and individually corrected radiographs in TMJ transcranial radiography
- Magnetic resonance imaging-based temporomandibular joint space evaluation in temporomandibular disorders
- Condylar position on the lateral individualized corrected tomography in internal derangement of temporomandibular joint