Ann Surg Treat Res.
2016 Feb;90(2):106-110. 10.4174/astr.2016.90.2.106.
Laparoscopic completion total gastrectomy for remnant gastric cancer following pancreaticoduodenectomy for bile duct cancer: a case report
- Affiliations
-
- 1Department of Surgery, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. kimwook@catholic.ac.kr
- KMID: 2166830
- DOI: http://doi.org/10.4174/astr.2016.90.2.106
Abstract
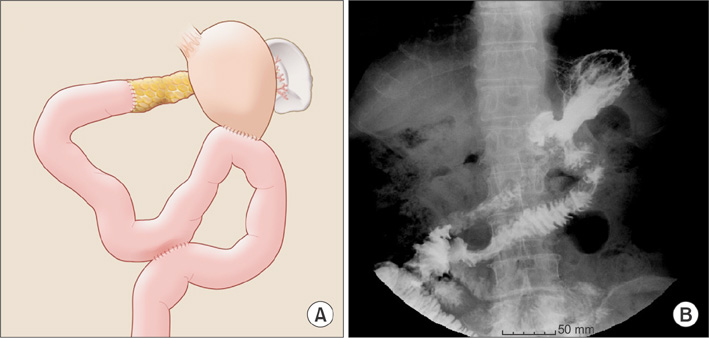
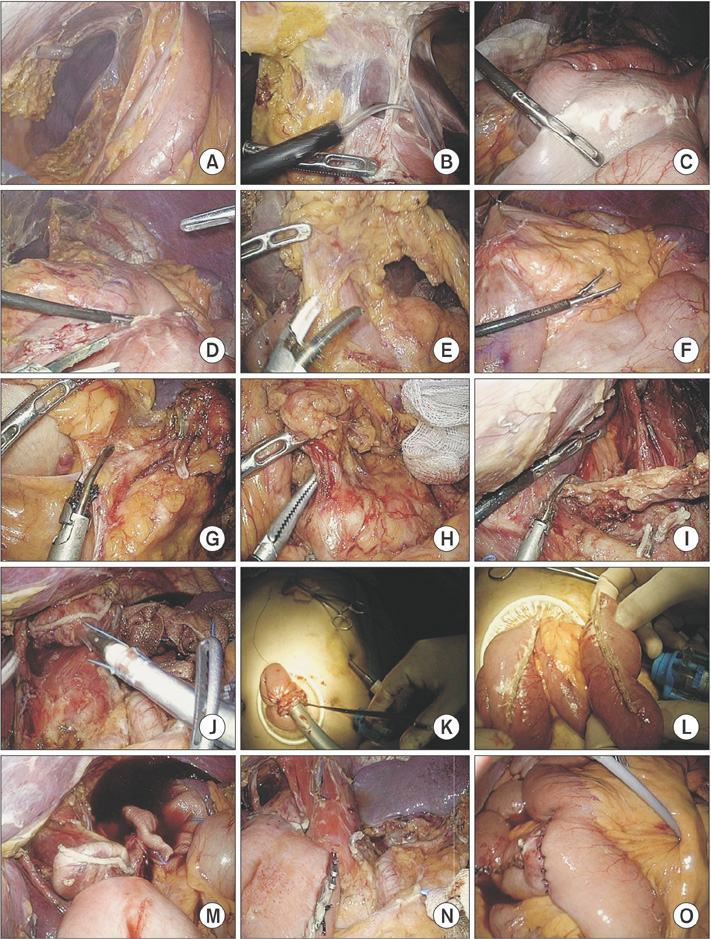
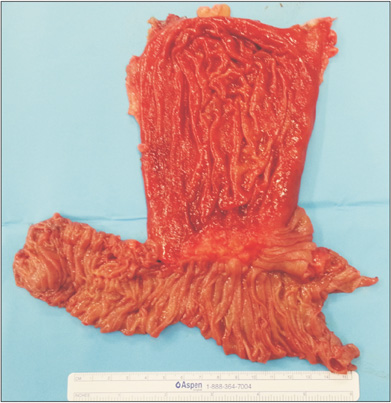
- Laparoscopic completion total gastrectomy following pancreaticoduodenectomy (PD) has not been reported. A 73-year-old male who underwent PD 25 years ago for distal common bile duct cancer visited a surgical department for remnant gastric cancer. A previous reconstruction was performed with pancreaticojejunostomy (PJ), gastrojejunostomy and Braun anastomosis, i.e., jejunojejunostomy (JJ), between the afferent and efferent jejunal limb to prevent bile reflux into the remnant stomach. Adhesiolysis was initially performed to secure the surgical view. Lymph node dissections around the splenic artery, splenic hilum, celiac axis, left gastric artery, and common hepatic artery were performed. The PJ site was well visualized and safely preserved. Esophagojejunostomy was performed with an OrVil system. Specimen retrieval, Roux-limb preparation and JJ were performed through an extended umbilicus trocar site. A final pathologic examination revealed a 5.5-cm serosa-exposed tumor (T4a) without lymph node metastasis. The patient was discharged on postoperative day 7 without any complications.
Keyword
MeSH Terms
-
Aged
Arteries
Axis, Cervical Vertebra
Bile Duct Neoplasms*
Bile Ducts*
Bile Reflux
Bile*
Common Bile Duct
Extremities
Gastrectomy*
Gastric Bypass
Gastric Stump
Hepatic Artery
Humans
Laparoscopy
Lymph Node Excision
Lymph Nodes
Male
Neoplasm Metastasis
Pancreaticoduodenectomy*
Pancreaticojejunostomy
Splenic Artery
Stomach Neoplasms*
Surgical Instruments
Umbilicus
Figure
Reference
-
1. Jung YJ, Kim DJ, Lee JH, Kim W. Safety of intracorporeal circular stapling esophagojejunostomy using trans-orally inserted anvil (OrVil) following laparoscopic total or proximal gastrectomy - comparison with extracorporeal anastomosis. World J Surg Oncol. 2013; 11:209.2. Kim DJ, Lee JH, Kim W. A comparison of total versus partial omentectomy for advanced gastric cancer in laparoscopic gastrectomy. World J Surg Oncol. 2014; 12:64.3. Son SY, Lee CM, Jung DH, Lee JH, Ahn SH, Park do J, et al. Laparoscopic completion total gastrectomy for remnant gastric cancer: a single-institution experience. Gastric Cancer. 2015; 18:177–182.4. Song J, Kim JY, Kim S, Choi WH, Cheong JH, Hyung WJ, et al. Laparoscopic completion total gastrectomy in remnant gastric cancer: technical detail and experience of two cases. Hepatogastroenterology. 2009; 56:1249–1252.5. Kim HH, Han SU, Kim MC, Hyung WJ, Kim W, Lee HJ, et al. Long-term results of laparoscopic gastrectomy for gastric cancer: a large-scale case-control and case-matched Korean multicenter study. J Clin Oncol. 2014; 32:627–633.6. Jeong O, Jung MR, Kim GY, Kim HS, Ryu SY, Park YK. Comparison of short-term surgical outcomes between laparoscopic and open total gastrectomy for gastric carcinoma: case-control study using propensity score matching method. J Am Coll Surg. 2013; 216:184–191.7. Yamada H, Kojima K, Yamashita T, Kawano T, Sugihara K, Nihei Z. Laparoscopy-assisted resection of gastric remnant cancer. Surg Laparosc Endosc Percutan Tech. 2005; 15:226–229.8. Cho HJ, Kim W, Hur H, Jeon HM. Laparoscopy-assisted completion total gastrectomy for gastric cancer in remnant stomach: report of 2 cases. Surg Laparosc Endosc Percutan Tech. 2009; 19:e57–e60.9. Kim W, Lee JH, Kim JJ, Chin HM, Jeon HM, Park CH, et al. Clinical analysis of the gastric stump cancer-classification proposed by the Korean Gastric Cancer Association-. J Korean Surg Soc. 2004; 66:177–182.10. Wiggins T, Markar SR, Harris A. Laparoscopic adhesiolysis for acute small bowel obstruction: systematic review and pooled analysis. Surg Endosc. 2015; 29:3432–3442.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Entirely Laparoscopic Gastrectomy and Colectomy for Remnant Gastric Cancer with Gastric Outlet Obstruction and Transverse Colon Invasion
- Bile Duct Cancer afterSubtotal Gastrectomy for Early Gastric Cancer: Report of 2 Cases
- Prognostic significance of splenectomy during completion total gastrectomy in patients with remnant gastric cancer: propensity score matching analysis
- Is Laparoscopic Approach Also Safe for the Treatment of Remnant Gastric Cancer?
- Single-Port Laparoscopic Proximal Gastrectomy with Double Tract Reconstruction for Early Gastric Cancer: Report of a Case