Ann Surg Treat Res.
2016 Feb;90(2):79-88. 10.4174/astr.2016.90.2.79.
Effects of intensive nutrition education on nutritional status and quality of life among postgastrectomy patients
- Affiliations
-
- 1Nutrition Team, Kyung Hee University Hospital at Gangdong, Seoul, Korea.
- 2Department of Food and Nutrition, Sungshin Women's University, Seoul, Korea.
- 3Department of Surgery, Kyung Hee University Hospital at Gangdong, Seoul, Korea.
- 4Department of Medical Nutrition, Graduate School of East-West Medical Science, Kyung Hee University, Yongin, Korea. hjlim@khu.ac.kr
- 5Institute of Medical Nutrition, Kyung Hee University, Seoul, Korea.
- KMID: 2166826
- DOI: http://doi.org/10.4174/astr.2016.90.2.79
Abstract
- PURPOSE
We examined the effects of 3 months of intensive education (IE) after hospital discharge compared to conventional education (CE) on nutritional status and quality of diet and life among South Korean gastrectomy patients.
METHODS
The study was conducted among 53 hospitalized gastrectomy in-patients (IE group, n = 28; CE group, n = 25) at Kyung Hee University Hospital at Gangdong. Baseline data were collected from electronic medical records and additional information was gathered via anthropometric measurements, assessment of nutritional status through a patient-generated, subjective global assessment (PG-SGA), diet assessment, and measures of self-efficacy and satisfaction with meals for 3 months following hospital discharge.
RESULTS
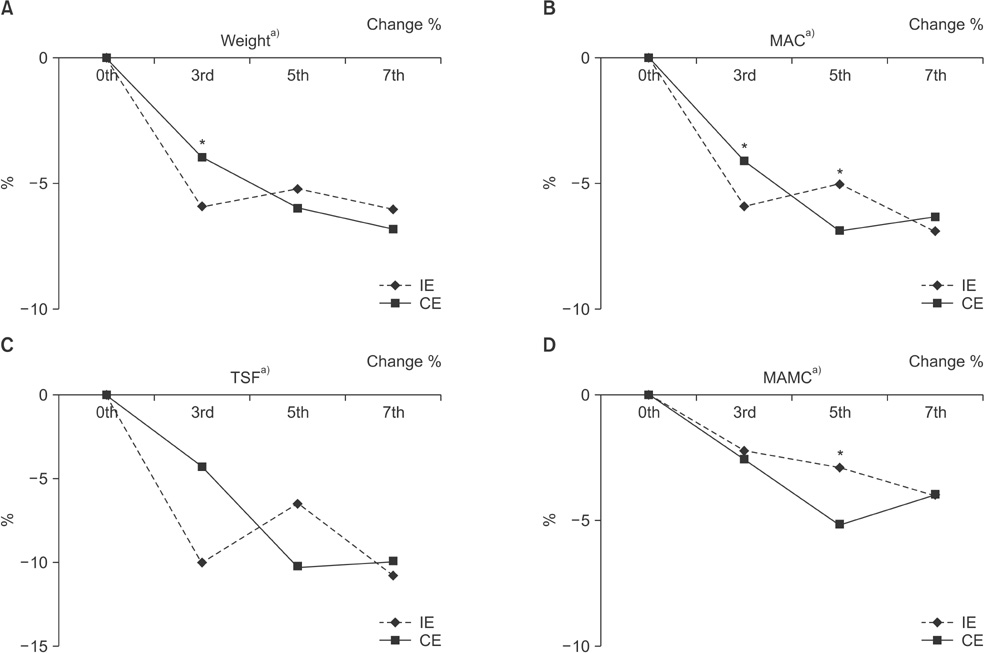
Total PG-SGA scores were significantly higher in the CE group than in the IE group at 3-week post-discharge (5.2 in the IE group vs. 10.4 in the CE group, P < 0.001), with higher scores indicating a greater severity of malnutrition. Energy intake over the 3 months increased in both the IE group (from 1,390 to 1,726 kcal/day) and the CE group (from 1,227 to 1,540 kcal/day). At 3-week post-discharge, the IE group had significantly higher daily protein and fat intake (P < 0.05). Self-efficacy improved in each category (P < 0.001), except for 'difficulty eating adequate food'. When assessing satisfaction with meals, there was a difference in the 'satisfaction with the current meal size' (P < 0.001) and 'satisfaction with the menu content' (P < 0.001).
CONCLUSION
Nutritional status among gastrectomy patients in the IE group improved. Relative to the CE control, the IE group demonstrated improved self-efficacy and meal satisfaction 3-week post-discharge.
MeSH Terms
Figure
Reference
-
1. International Agency for Research on Cancer. Globocan 2012: estimated cancer incidence, mortality and prevalence worldwide in 2012 – all cancers (excluding non-melanoma skin cancer) [Internet]. Lyon: International Agency for Research on Cancer;c2015. cited 2015 May 12. Available from: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx.2. International Agency for Research on Cancer. Globocan 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012: Stomach cancer [Internet]. Lyon: International Agency for Research on Cancer;c2015. cited 2015 May 12. Available from: http://globocan.iarc.fr/old/FactSheets/cancers/stomachnew.asp.3. Statistics Korea [Internet]. Daejeon: Statistics Korea;c1996. cited 2015 May 12. Available from: http://kostat.go.kr/portal/korea/index.action.4. National Cancer Information Center [Internet]. Korea: National Cancer Information Center;c2005. cited 2015 May 12. Available from: http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_040102000000.5. Yim JY, Kim N, Choi SH, Kim YS, Cho KR, Kim SS, et al. Seroprevalence of Helicobacter pylori in South Korea. Helicobacter. 2007; 12:333–340.6. Jee SH, Samet JM, Ohrr H, Kim JH, Kim IS. Smoking and cancer risk in Korean men and women. Cancer Causes Control. 2004; 15:341–348.7. Shin A, Kim J, Park S. Gastric cancer epidemiology in Korea. J Gastric Cancer. 2011; 11:135–140.8. Kim HJ, Chang WK, Kim MK, Lee SS, Choi BY. Dietary factors and gastric cancer in Korea: a case-control study. Int J Cancer. 2002; 97:531–535.9. Lee JK, Park BJ, Yoo KY, Ahn YO. Dietary factors and stomach cancer: a case-control study in Korea. Int J Epidemiol. 1995; 24:33–41.10. American Cancer Society [Internet]. Atlanta (GA): American Cancer Society;c2009. cited 2015 May 12. Available from: http://www.cancer.org/cancer/stomachcancer/detailedguide/stomachcancer-treating-general-info.11. Ryu SW, Kim IH. Comparison of different nutritional assessments in detecting malnutrition among gastric cancer patients. World J Gastroenterol. 2010; 16:3310–3317.12. Oh CA, Kim DH, Oh SJ, Choi MG, Noh JH, Sohn TS, et al. Nutritional risk index as a predictor of postoperative wound complications after gastrectomy. World J Gastroenterol. 2012; 18:673–678.13. Carey S, Storey D, Biankin AV, Martin D, Young J, Allman-Farinelli M. Long term nutritional status and quality of life following major upper gastrointestinal surgery: a cross-sectional study. Clin Nutr. 2011; 30:774–779.14. Hirao M, Tsujinaka T, Takeno A, Fujitani K, Kurata M. Patient-controlled dietary schedule improves clinical outcome after gastrectomy for gastric cancer. World J Surg. 2005; 29:853–857.15. Liu H, Ling W, Shen ZY, Jin X, Cao H. Clinical application of immune-enhanced enteral nutrition in patients with advanced gastric cancer after total gastrectomy. J Dig Dis. 2012; 13:401–406.16. Kim H, Suh EE, Lee HJ, Yang HK. The effects of patient participation-based dietary intervention on nutritional and functional status for patients with gastrectomy: a randomized controlled trial. Cancer Nurs. 2014; 37:E10–E20.17. Ottery FD. Definition of standardized nutritional assessment and interventional pathways in oncology. Nutrition. 1996; 12:S15–S19.18. Ryan AM, Healy LA, Power DG, Rowley SP, Reynolds JV. Short-term nutritional implications of total gastrectomy for malignancy, and the impact of parenteral nutritional support. Clin Nutr. 2007; 26:718–727.19. Park JY, Kim YJ. Successful laparoscopic reversal of gastric bypass in a patient with malnutrition. Ann Surg Treat Res. 2014; 87:217–221.20. Yu EJ, Kang JH, Yoon S, Chung HK. Changes in nutritional status according to biochemical assay, body weight, and nutrient intake levels in gastrectomy patients. J Korean Diet Assoc. 2012; 18:16–29.21. Carey S, Ferrie S, Ryan R, Beaton J, Young J, Allman-Farinelli M. Long-term nutrition intervention following major upper gastrointestinal surgery: a prospective randomized controlled trial. Eur J Clin Nutr. 2013; 67:324–329.22. Jeong MJ, Kim CY, Kim SB. A study on nutritional status after gastrectomy of gastric cancer patients in Jeonbuk province. Korean J Community Nutr. 2006; 11:785–792.23. Beattie AH, Prach AT, Baxter JP, Pennington CR. A randomised controlled trial evaluating the use of enteral nutritional supplements postoperatively in malnourished surgical patients. Gut. 2000; 46:813–818.24. Na JR, Suh YS, Kong SH, Lim JH, Ju DL, Yang HK, et al. A prospective observational study evaluating the change of nutritional status and the incidence of dumping syndrome after gastrectomy. J Clin Nutr. 2014; 6:59–70.25. Chen W, Zhang Z, Xiong M, Meng X, Dai F, Fang J, et al. Early enteral nutrition after total gastrectomy for gastric cancer. Asia Pac J Clin Nutr. 2014; 23:607–611.26. Sun V, Kim J, Kim JY, Raz DJ, Merchant S, Chao J, et al. Dietary alterations and restrictions following surgery for upper gastrointestinal cancers: key components of a health-related quality of life intervention. Eur J Oncol Nurs. 2015; 19:343–348.27. Carey S, Laws R, Ferrie S, Young J, Allman-Farinelli M. Struggling with food and eating--life after major upper gastrointestinal surgery. Support Care Cancer. 2013; 21:2749–2757.28. Copland L, Liedman B, Rothenberg E, Bosaeus I. Effects of nutritional support long time after total gastrectomy. Clin Nutr. 2007; 26:605–613.29. Tian J, Chen JS. Nutritional status and quality of life of the gastric cancer patients in Changle County of China. World J Gastroenterol. 2005; 11:1582–1586.30. Song WJ, Kang KC, Heo YS, Shin SH. Comparison of short-term and long-term qualities of life after curative open gastrectomy in patients with gastric cancer. Korean J Clin Oncol. 2010; 6:12–19.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Nutrition Education on the Eating Habits and Quality of Life of Gastric Cancer Outpatients Undergoing Gastrectomy
- Nutritional treatment after gastrectomy
- Nutritional Status and Food Insufficiency of Korean Population through the Life-Course by Education Level Based on 2005 National Health and Nutrition Survey
- The Effect of Nutrition Education Program in Physical Health, Nutritional Status and Health-Related Quality of Life of the Elderly in Seoul
- The Effects of Nutrition Education and Regular Exercise on Nutritional Status, Quality of Life and Fatigue in Hemodialysis Patients