Clin Exp Otorhinolaryngol.
2016 Mar;9(1):70-74. 10.21053/ceo.2016.9.1.70.
Voice Outcome in Patients Treated With Endoscopic Laryngopharyngeal Surgery for Superficial Hypopharyngeal Cancer
- Affiliations
-
- 1Department of Otolaryngology-Head & Neck Surgery, Graduate School of Medicine, Kyoto University, Kyoto, Japan. tateya@ent.kuhp.kyoto-u.ac.jp
- 2Department of Gastroenterology & Hepatology, Graduate School of Medicine, Kyoto University, Kyoto, Japan.
- 3Department of Clinical Oncology, Graduate School of Medicine, Kyoto University, Kyoto, Japan.
- KMID: 2166292
- DOI: http://doi.org/10.21053/ceo.2016.9.1.70
Abstract
OBJECTIVES
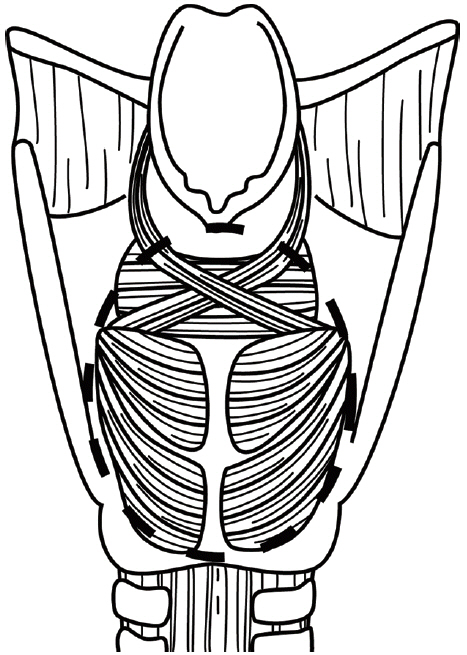
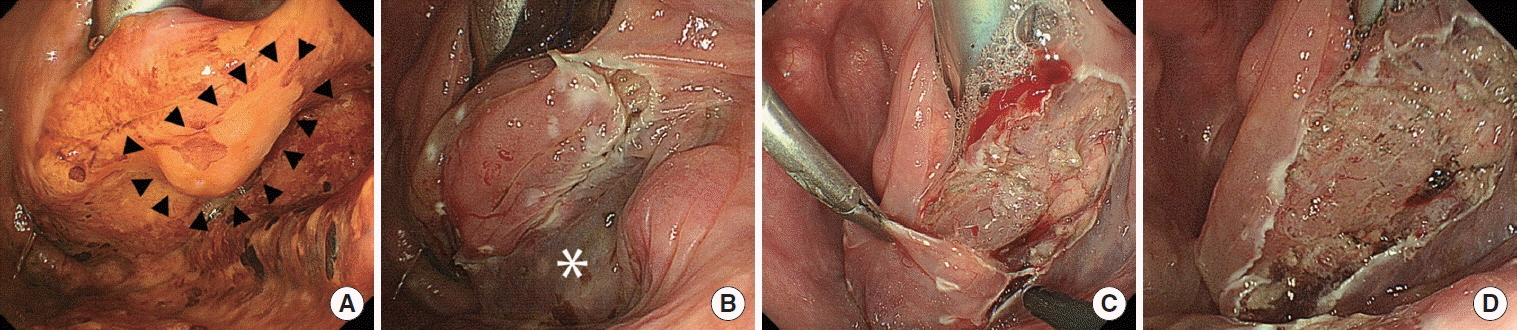
Endoscopic laryngopharyngeal surgery (ELPS) is a minimally invasive transoral surgery that was developed to treat superficial larygo-pharyngeal cancer, in which a mucosal lesion is resected transorally while preserving deeper structures by subepithelial injection. The purpose of this retrospective study is to evaluate voice outcome in patients who underwent ELPS for superficial hypopharyngeal cancer. As important structures in producing voice, such as intrinsic laryngeal muscles, their fascia, and recurrent laryngeal nerve, are located in the medial side of the piriform sinus and the postcricoid region of the hypopharynx, we focused on patients with cancer lesions involving these regions.
METHODS
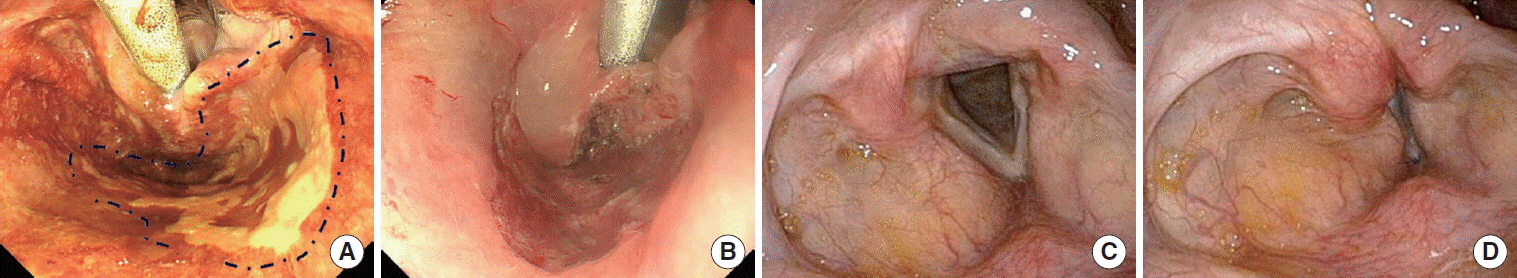
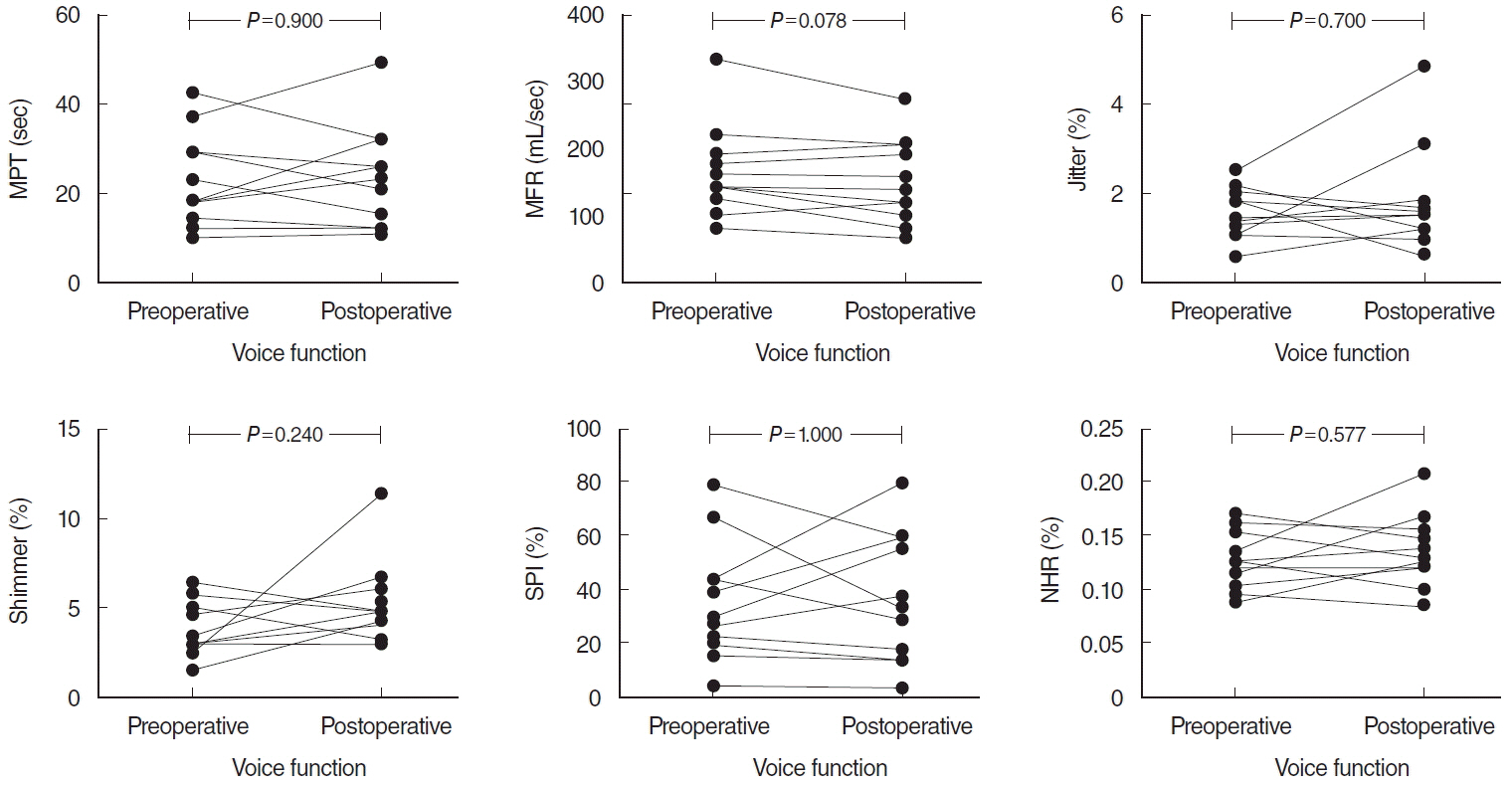
From April 2010 to March 2011, 25 consecutive patients with superficial laryngopharyngeal cancer were treated with ELPS at Kyoto University Hospital. Among the 25 patients, 11 patients with cancer lesions on the medial side of the piriform sinus or the postcricoid area were studied. Preoperative and postoperative voice functions including maximum phonation time (MPT), mean flow rate (MFR), jitter, shimmer, soft phonation index (SPI), and noise-to-harmonic ratio (NHR), were compared retrospectively.
RESULTS
Five of 11 cancer lesions had submucosal invasion and no lesion had invaded the muscular layer pathologically. T stage was classified as Tis in 5 cases, T1 in 4 cases, and T2 in 2 cases. All lesions involved the medial side of the piriform sinus and 2 also involved the postcricoid area. Vocal fold movement was normal in all cases after the surgery. Average preoperative and postoperative values for MPT, MFR, jitter, shimmer, SPI, and NHR, were 22.7 seconds and 23.4 seconds, 165 mL/sec and 150 mL/sec, 1.53% and 1.77%, 3.82% and 5.17%, 35.5 and 36.6, and 0.13% and 0.14%, respectively. There was no statistical difference between preoperative and postoperative data for all values examined.
CONCLUSION
ELPS is useful in preserving voice function in the treatment of superficial hypopharyngeal cancer. Preserving the deeper structures including intrinsic muscles and their fascia may be important for preserving voice function as long as the lesions are superficial.
Keyword
MeSH Terms
Figure
Reference
-
1. Muto M, Horimatsu T, Ezoe Y, Morita S, Miyamoto S. Improving visualization techniques by narrow band imaging and magnification endoscopy. J Gastroenterol Hepatol. 2009; Aug. 24(8):1333–46.
Article2. Muto M, Katada C, Sano Y, Yoshida S. Narrow band imaging: a new diagnostic approach to visualize angiogenesis in superficial neoplasia. Clin Gastroenterol Hepatol. 2005; Jul. 3(7 Suppl 1):S16–20.
Article3. Muto M, Minashi K, Yano T, Saito Y, Oda I, Nonaka S, et al. Early detection of superficial squamous cell carcinoma in the head and neck region and esophagus by narrow band imaging: a multicenter randomized controlled trial. J Clin Oncol. 2010; Mar. 28(9):1566–72.
Article4. Muto M, Nakane M, Katada C, Sano Y, Ohtsu A, Esumi H, et al. Squamous cell carcinoma in situ at oropharyngeal and hypopharyngeal mucosal sites. Cancer. 2004; Sep. 101(6):1375–81.
Article5. Sato Y, Omori Y, Tagawa M. Treatment of superficial carcinoma in hypopharynx. Nihon Jibiinkoka Gakkai Kaiho. 2006; Dec. 109(7):581–6.6. Tateya I, Morita S, Muto M, Miyamoto S, Hayashi T, Funakoshi M, et al. Magnifying endoscope with NBI to predict the depth of invasion in laryngo-pharyngeal cancer. Laryngoscope. 2015; May. 125(5):1124–9.7. Japan Society for Head and Neck Cancer. General rules for clinical studies on head and neck cancer. 5th ed. Tokyo: Kanehara Publishing Group;2012.8. Japan Esophageal Society. Japanese classification of esophageal cancer, tenth edition: part I. Esophagus. 2009; Mar. 6(1):1–25.9. Steiner W. Experience in endoscopic laser surgery of malignant tumours of the upper aero-digestive tract. Adv Otorhinolaryngol. 1988; 39:135–44.
Article10. O’Malley BW Jr, Weinstein GS, Snyder W, Hockstein NG. Transoral robotic surgery (TORS) for base of tongue neoplasms. Laryngoscope. 2006; Aug. 116(8):1465–72.11. Weinstein GS, O’Malley BW Jr, Snyder W, Hockstein NG. Transoral robotic surgery: supraglottic partial laryngectomy. Ann Otol Rhinol Laryngol. 2007; Jan. 116(1):19–23.
Article12. Park YM, Byeon HK, Chung HP, Choi EC, Kim SH. Comparison study of transoral robotic surgery and radical open surgery for hypopharyngeal cancer. Acta Otolaryngol. 2013; Jun. 133(6):641–8.
Article13. Tomifuji M, Araki K, Yamashita T, Shiotani A. Transoral videolaryngoscopic surgery for oropharyngeal, hypopharyngeal, and supraglottic cancer. Eur Arch Otorhinolaryngol. 2014; Mar. 271(3):589–97.
Article14. Park YM, Kim WS, De Virgilio A, Lee SY, Seol JH, Kim SH. Transoral robotic surgery for hypopharyngeal squamous cell carcinoma: 3-year oncologic and functional analysis. Oral Oncol. 2012; Jun. 48(6):560–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pepsin and Laryngeal and Hypopharyngeal Carcinomas
- Endoscopic Resection of Hypopharyngeal Squamous Cell Carcinoma
- Change of Voice Quality before and after Treatment of Short-Term Therapy with Proton Pump Inhibitor in Laryngopharyngeal Reflux
- A Case of Hypopharyngeal Cancer Treated by Endoscopic Submucosal Dissection
- A Hypopharyngeal Ductal Cyst Masquerading as a Laryngopharyngeal Reflux Disease