Ann Rehabil Med.
2015 Jun;39(3):462-472. 10.5535/arm.2015.39.3.462.
Utility of a Three-Dimensional Interactive Augmented Reality Program for Balance and Mobility Rehabilitation in the Elderly: A Feasibility Study
- Affiliations
-
- 1Department of Rehabilitation, Eulji Hospital, Eulji University School of Medicine, Seoul, Korea. md52516@hanmail.net
- 2Department of Biomedical Engineering, Keimyung University, Daegu, Korea.
- 3Department of Rehabilitation, Daehan Hospital, Seoul, Korea.
- 4Graduate School of Technology and Innovation Management, Hanyang University, Seoul, Korea.
- 5Department of Occupational Therapy, Eulji Hospital, Seoul, Korea.
- 6Department of Physical therapy, Eulji Hospital, Seoul, Korea.
- 7Department of Biostatistics, Yonsei University of College of Medicine, Seoul, Korea.
- KMID: 2165650
- DOI: http://doi.org/10.5535/arm.2015.39.3.462
Abstract
OBJECTIVE
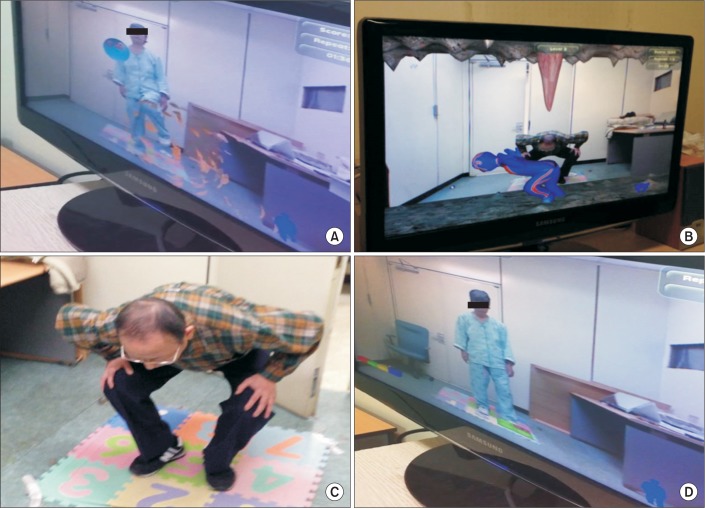
To improve lower extremity function and balance in elderly persons, we developed a novel, three-dimensional interactive augmented reality system (3D ARS). In this feasibility study, we assessed clinical and kinematic improvements, user participation, and the side effects of our system.
METHODS
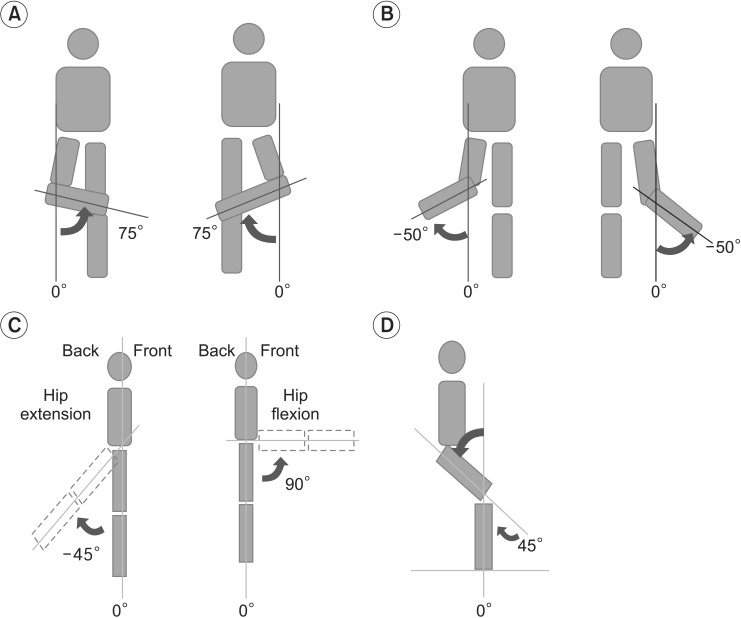
Eighteen participants (age, 56-76 years) capable of walking independently and standing on one leg were recruited. The participants received 3D ARS training during 10 sessions (30-minute duration each) for 4 weeks. Berg Balance Scale (BBS) and the Timed Up and Go (TUG) scores were obtained before and after the exercises. Outcome performance variables, including response time and success rate, and kinematic variables, such as hip and knee joint angle, were evaluated after each session.
RESULTS
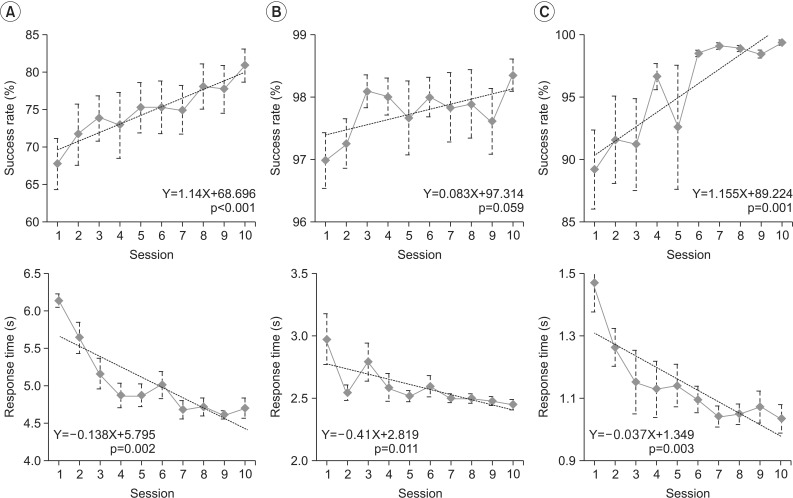
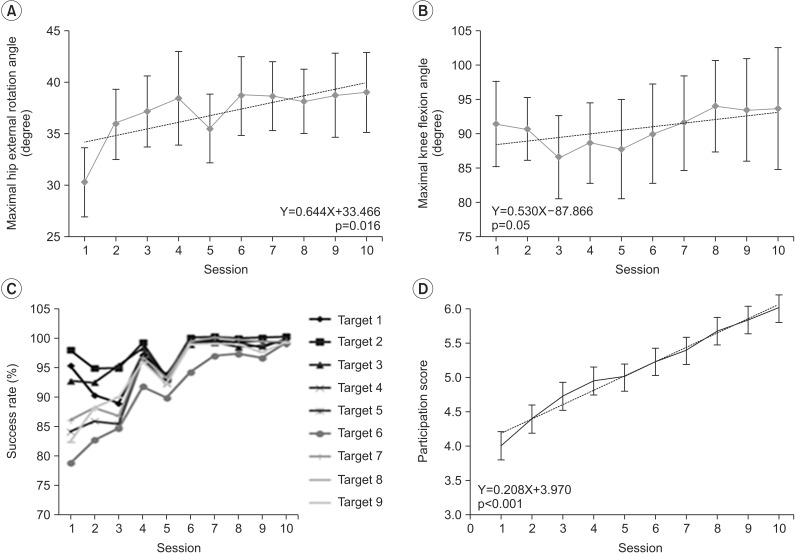
Participants exhibited significant clinical improvements in lower extremity balance and mobility following the intervention, as shown by improved BBS and TUG scores (p<0.001). Consistent kinematic improvements in the maximum joint angles of the hip and knee were observed across sessions. Outcome performance variables, such as success rate and response time, improved gradually across sessions, for each exercise. The level of participant interest also increased across sessions (p<0.001). All participants completed the program without experiencing any adverse effects.
CONCLUSION
Substantial clinical and kinematic improvements were observed after applying a novel 3D ARS training program, suggesting that this system can enhance lower extremity function and facilitate assessments of lower extremity kinematic capacity.
Keyword
MeSH Terms
Figure
Reference
-
1. Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006; 35(Suppl 2):ii37–ii41. PMID: 16926202.
Article2. Moylan KC, Binder EF. Falls in older adults: risk assessment, management and prevention. Am J Med. 2007; 120:493.e1–493.e6. PMID: 17524747.
Article3. Gschwind YJ, Kressig RW, Lacroix A, Muehlbauer T, Pfenninger B, Granacher U. A best practice fall prevention exercise program to improve balance, strength/power, and psychosocial health in older adults: study protocol for a randomized controlled trial. BMC Geriatr. 2013; 13:105. PMID: 24106864.
Article4. Hausdorff JM, Yogev G. Cognitive function may be important for fall injury prevention trials. J Am Geriatr Soc. 2006; 54:865–866. PMID: 16696767.
Article5. Mirelman A, Rochester L, Reelick M, Nieuwhof F, Pelosin E, Abbruzzese G, et al. V-TIME: a treadmill training program augmented by virtual reality to decrease fall risk in older adults: study design of a randomized controlled trial. BMC Neurol. 2013; 13:15. PMID: 23388087.
Article6. Szturm T, Betker AL, Moussavi Z, Desai A, Goodman V. Effects of an interactive computer game exercise regimen on balance impairment in frail community-dwelling older adults: a randomized controlled trial. Phys Ther. 2011; 91:1449–1462. PMID: 21799138.
Article7. Sveistrup H. Motor rehabilitation using virtual reality. J Neuroeng Rehabil. 2004; 1:10. PMID: 15679945.8. Lehrer N, Attygalle S, Wolf SL, Rikakis T. Exploring the bases for a mixed reality stroke rehabilitation system, part I: a unified approach for representing action, quantitative evaluation, and interactive feedback. J Neuroeng Rehabil. 2011; 8:51. PMID: 21875441.
Article9. Duff M, Chen Y, Attygalle S, Sundaram H, Rikakis T. Mixed reality rehabilitation for stroke survivors promotes generalized motor improvements. Conf Proc IEEE Eng Med Biol Soc. 2010; 2010:5899–5902. PMID: 21096934.
Article10. Lehrer N, Chen Y, Duff M, L Wolf S, Rikakis T. Exploring the bases for a mixed reality stroke rehabilitation system, Part II: design of interactive feedback for upper limb rehabilitation. J Neuroeng Rehabil. 2011; 8:54. PMID: 21899779.
Article11. Merians AS, Jack D, Boian R, Tremaine M, Burdea GC, Adamovich SV, et al. Virtual reality-augmented rehabilitation for patients following stroke. Phys Ther. 2002; 82:898–915. PMID: 12201804.
Article12. Duff M, Chen Y, Cheng L, Liu SM, Blake P, Wolf SL, et al. Adaptive mixed reality rehabilitation improves quality of reaching movements more than traditional reaching therapy following stroke. Neurorehabil Neural Repair. 2013; 27:306–315. PMID: 23213076.
Article13. Folstein MF, Folstein SE, McHugh PR. "Mini-mental state", a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975; 12:189–198. PMID: 1202204.14. Berg K, Wood-Dauphinee S, Williams JI. The Balance Scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995; 27:27–36. PMID: 7792547.15. Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000; 80:896–903. PMID: 10960937.16. Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991; 39:142–148. PMID: 1991946.17. Lenze EJ, Munin MC, Quear T, Dew MA, Rogers JC, Begley AE, et al. The Pittsburgh Rehabilitation Participation Scale: reliability and validity of a clinician-rated measure of participation in acute rehabilitation. Arch Phys Med Rehabil. 2004; 85:380–384. PMID: 15031821.
Article18. Altman DG, Bland JM. Absence of evidence is not evidence of absence. Aust Vet J. 1996; 74:311. PMID: 8937675.
Article19. Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012; 9:CD007146. PMID: 22972103.
Article20. Joshua AM, D'Souza V, Unnikrishnan B, Mithra P, Kamath A, Acharya V, et al. Effectiveness of progressive resistance strength training versus traditional balance exercise in improving balance among the elderly: a randomised controlled trial. J Clin Diagn Res. 2014; 8:98–102. PMID: 24783093.21. Shin SS, An DH. The effect of motor dual-task balance training on balance and gait of elderly women. J Phys Ther Sci. 2014; 26:359–361. PMID: 24707083.22. Kang KY. Effects of visual biofeedback training for fall prevention in the elderly. J Phys Ther Sci. 2013; 25:1393–1395. PMID: 24396196.23. Lee S, Shin S. Effectiveness of virtual reality using video gaming technology in elderly adults with diabetes mellitus. Diabetes Technol Ther. 2013; 15:489–496. PMID: 23560480.
Article24. Cho GH, Hwangbo G, Shin HS. The effects of virtual reality-based balance training on balance of the elderly. J Phys Ther Sci. 2014; 26:615–617. PMID: 24764645.
Article25. Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C. Exercise for improving balance in older people. Cochrane Database Syst Rev. 2011; (11):CD004963. PMID: 22071817.
Article26. Cikajlo I, Rudolf M, Goljar N, Burger H, Matjacic Z. Telerehabilitation using virtual reality task can improve balance in patients with stroke. Disabil Rehabil. 2012; 34:13–18. PMID: 21864205.
Article27. Weiss PL, Katz N. The potential of virtual reality for rehabilitation. J Rehabil Res Dev. 2004; 41:vii–x. PMID: 15558392.28. Jack D, Boian R, Merians AS, Tremaine M, Burdea GC, Adamovich SV, et al. Virtual reality-enhanced stroke rehabilitation. IEEE Trans Neural Syst Rehabil Eng. 2001; 9:308–318. PMID: 11561668.
Article29. Booth V, Masud T, Connell L, Bath-Hextall F. The effectiveness of virtual reality interventions in improving balance in adults with impaired balance compared with standard or no treatment: a systematic review and meta-analysis. Clin Rehabil. 2014; 28:419–431. PMID: 24188913.
Article30. de Bruin ED, Schoene D, Pichierri G, Smith ST. Use of virtual reality technique for the training of motor control in the elderly: some theoretical considerations. Z Gerontol Geriatr. 2010; 43:229–234. PMID: 20814798.31. Baus O, Bouchard S. Moving from virtual reality exposure-based therapy to augmented reality exposure-based therapy: a review. Front Hum Neurosci. 2014; 8:112. PMID: 24624073.
Article32. Botella CM, Juan MC, Banos RM, Alcaniz M, Guillen V, Rey B. Mixing realities? An application of augmented reality for the treatment of cockroach phobia. Cyberpsychol Behav. 2005; 8:162–171. PMID: 15938656.
Article33. Perani D, Fazio F, Borghese NA, Tettamanti M, Ferrari S, Decety J, et al. Different brain correlates for watching real and virtual hand actions. Neuroimage. 2001; 14:749–758. PMID: 11506547.
Article34. Tai YF, Scherfler C, Brooks DJ, Sawamoto N, Castiello U. The human premotor cortex is 'mirror' only for biological actions. Curr Biol. 2004; 14:117–120. PMID: 14738732.
Article35. Yoo HN, Chung E, Lee BH. The effects of augmented reality-based Otago exercise on balance, gait, and falls efficacy of elderly women. J Phys Ther Sci. 2013; 25:797–801. PMID: 24259856.36. Villiger M, Bohli D, Kiper D, Pyk P, Spillmann J, Meilick B, et al. Virtual reality-augmented neurorehabilitation improves motor function and reduces neuropathic pain in patients with incomplete spinal cord injury. Neurorehabil Neural Repair. 2013; 27:675–683. PMID: 23757298.
Article37. Prochnow D, Bermudez i, Schmidt J, Duff A, Brunheim S, Kleiser R, et al. A functional magnetic resonance imaging study of visuomotor processing in a virtual reality-based paradigm: rehabilitation gaming system. Eur J Neurosci. 2013; 37:1441–1447. PMID: 23414211.
Article38. Webster D, Celik O. Systematic review of Kinect applications in elderly care and stroke rehabilitation. J Neuroeng Rehabil. 2014; 11:108. PMID: 24996956.
Article39. Hiengkaew V, Jitaree K, Chaiyawat P. Minimal detectable changes of the Berg Balance Scale, Fugl-Meyer Assessment Scale, Timed "Up & Go" Test, gait speeds, and 2-minute walk test in individuals with chronic stroke with different degrees of ankle plantarflexor tone. Arch Phys Med Rehabil. 2012; 93:1201–1208. PMID: 22502805.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Electrical Stimulation-Augmented Virtual Reality Training in Improving Balance in Individuals with Incomplete Spinal Cord Injury: Study Protocol of a Randomized Controlled Trial
- Augmented Reality in Medicine
- Advanced Medical Use of Three-Dimensional Imaging in Congenital Heart Disease: Augmented Reality, Mixed Reality, Virtual Reality, and Three-Dimensional Printing
- Clinical Application of AR System in Early Rehabilitation Program After Stroke: 2 Case Study
- The effect of utilizing augmented reality in a mobile application for sequential tooth carving by users