Clin Endosc.
2011 Sep;44(1):27-32.
Efficacy of I-scan Endoscopy in the Diagnosis of Gastroesophageal Reflux Disease with Minimal Change
- Affiliations
-
- 1Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea. sychoi@dau.ac.kr
Abstract
- BACKGROUND/AIMS
The aim of the study was to evaluate the efficacy of i-scans for the diagnosis of gastroesophageal reflux disease, especially where only minimal change is involved.
METHODS
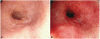
The esophageal mucosa was inspected using an i-scan following conventional white light endoscopy. The examination with iscan was performed under tone enhancement (TE) esophagus (e) mode. Patients with subtle distal esophageal mucosal changes without definite mucosal breaks, such as blurring of Z-line (B), mucosal coarseness (C), hyperemic or purplish discoloration (D), erythema (E), ectopic gastric mucosal islet (I) and mixed type were classified as minimal change.
RESULTS
A total of 156 patients were included. Using i-scan endoscopy, the number of minimal change was found to further increase from 94 (conventional endoscopy; 19B, 9C, 29D, 13E, 5I, 19 mixed type) to 109 (i-scan; 15B, 8C, 29D, 16E, 5I, 36 mixed type). And 14 patients who had single type by conventional endoscopy were converted to mixed type after i-scan. Therefore, 29 of 156 patients were upgraded after i-scan, they were account for 19% (p<0.0001; 95% confidence interval, 0.13 to 0.25).
CONCLUSIONS
The use of i-scan endoscopy significantly improves the identification of minimal change and helps to identify more precisely the type of minimal change.
Keyword
Figure
Reference
-
1. DeVault KR, Castell DO. American College of Gastroenterology. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol. 2005; 100:190–200. PMID: 15654800.
Article2. Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997; 112:1448–1456. PMID: 9136821.
Article3. Kim HY, Kim N, Kim SM, et al. Clinical spectrum and risk factors of erosive and non-erosive GERD in health check-up subjects. Korean J Med. 2006; 71:491–500.4. Youn YH, Kang YW, Ahn SH, Park SK. Prevalence alteration of reflux esophagitis in recent years. Korean J Gastrointest Endosc. 2001; 23:144–148.5. Jeon SG, Sohn CI, Kim JE, et al. Prevalence of gastroesophageal reflux in routine check-up subjects. Korean J Med. 2000; 58:145–151.6. Rhee PI. Evidence based guideline for diagnosis and treatment: diagnostic guideline for GERD. Korean J Neurogastroenterol Motil. 2005; 11:5–12.7. Jones R. Gastro-oesophageal reflux disease in general practice. Scand J Gastroenterol Suppl. 1995; 211:35–38. PMID: 8545629.
Article8. Kim WJ, Cho JY, Jeong SW, et al. Comparison of autofluorescence imaging endoscopic findings with pathologic findings after endoscopic submucosal dissection of gastric neoplasms. Gut Liver. 2008; 2:186–192. PMID: 20485645.
Article9. Chaiteerakij R, Rerknimitr R, Kullavanijaya P. Role of digital chromoendoscopy in detecting minimal change esophageal reflux disease. World J Gastrointest Endosc. 2010; 2:121–129. PMID: 21160727.
Article10. Sharma P, Wani S, Bansal A, et al. A feasibility trial of narrow band imaging endoscopy in patients with gastroesophageal reflux disease. Gastroenterology. 2007; 133:454–464. PMID: 17681166.
Article11. Hoffman A, Basting N, Goetz M, et al. High-definition endoscopy with i-Scan and Lugol's solution for more precise detection of mucosal breaks in patients with reflux symptoms. Endoscopy. 2009; 41:107–112. PMID: 19214887.
Article12. Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999; 45:172–180. PMID: 10403727.
Article13. Hongo M. Minimal changes in reflux esophagitis: red ones and white ones. J Gastroenterol. 2006; 41:95–99. PMID: 16568367.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimal Change Esophagitis
- Is Gastroesophageal Reflux Disease and Achalasia Coincident or Not?
- Usefulness of the Korean Version of the Gastroesophageal Reflux Disease Questionnaire for the Diagnosis of Gastroesophageal Reflux Disease Using Validation Study
- Diagnosis and Treatment of Gastroesophageal Reflux Disease
- Radiologic studies on gastroesophageal reflux