Korean J Perinatol.
2015 Dec;26(4):348-351. 10.14734/kjp.2015.26.4.348.
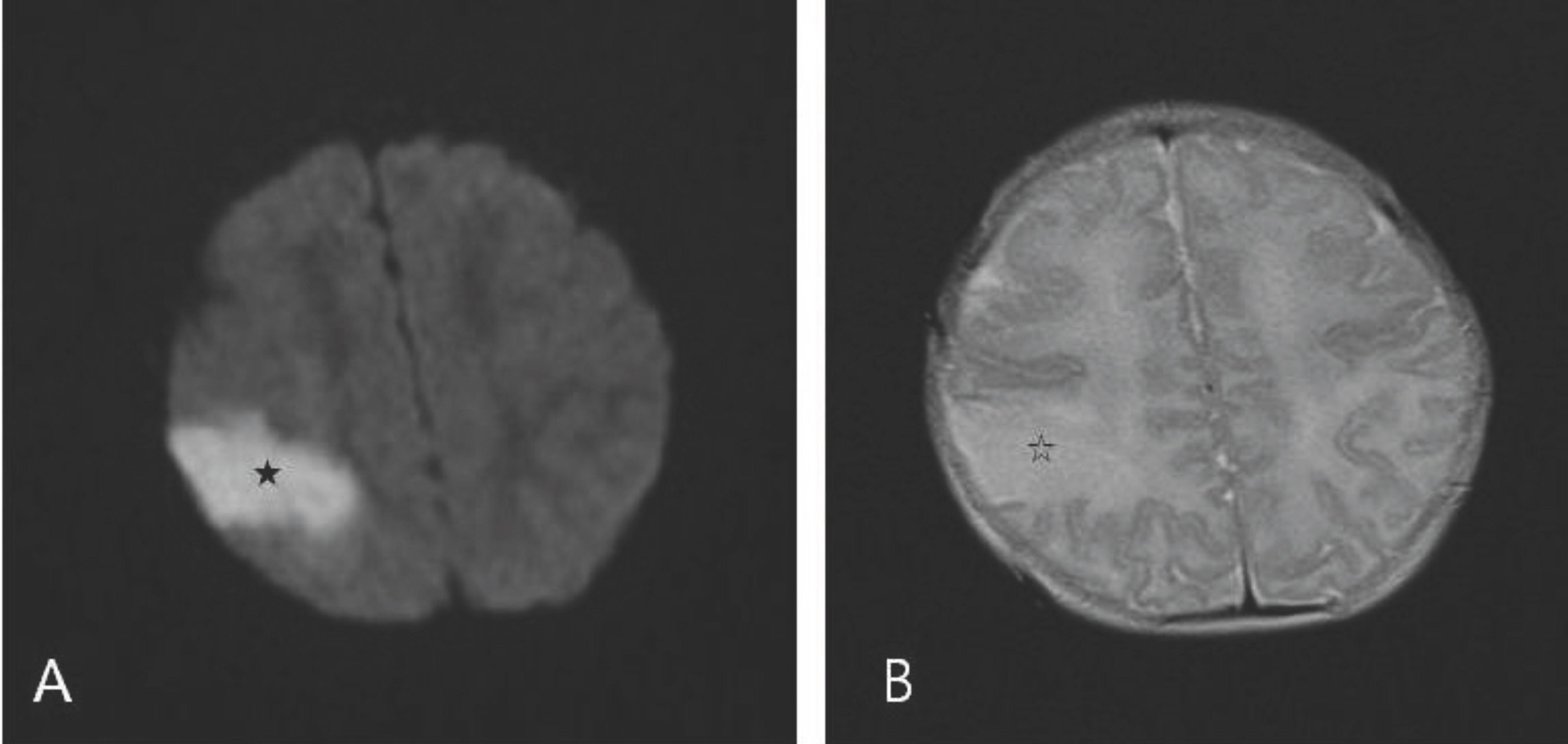
A Case of Neonatal Cerebral Infarction associated with Mutation in homozygous MTHFR C677T Gene
- Affiliations
-
- 1Department of Pediatrics, School of Medicine, Chosun University, Gwangju, Korea. skpark@chosun.ac.kr
- KMID: 2164191
- DOI: http://doi.org/10.14734/kjp.2015.26.4.348
Abstract
- C677T mutation in the gene encoding 5,10-methylenetetrahydrofolate reductase (MTHFR) predisposes to hyperhomocysteinemia in vivo and is known to be one of the causes of perinatal ischemic stroke. As MTHFR plays a role in the metabolism of homocysteine, C677T mutation may account for reduced enzymatic activity resulting in hyperhomocysteinemia. This may be prevented by introducing activity-enhancing coenzymes such as folic acid, vitamin B6, and B12. Though C677T mutation is known as a significant risk factor for cerebral infarction, reported cases of cerebral infarction among affected neonates are scarce. This report describes a case of a neonate homozygous for C677T mutation who had a perinatal ischemic stroke, born in a mother whose folic acid and nutritional consumption had been reduced during pregnancy.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Nelson KB, Lynch JK. Stroke in newborn infants. Lancet Neurol. 2004; 3:150–8.
Article2. Barmada MA, Moossy J, Shuman RM. Cerebral infarcts with arterial occlusion in neonates. Ann Neurol. 1979; 6:495–502.
Article3. deVeber G, Roach ES, Riela AR, Wiznitzer M. Stroke in children: recognition, treatment, and future directions. Semin Pediatr Neurol. 2000; 7:309–17.
Article4. McCully KS. Vascular pathology of homocysteinemia: implications for the pathogenesis of arteriosclerosis. Am J Pathol. 1969; 56:111–28.5. Clarke R, Daly L, Robinson K, Naughten E, Cahalane S, Fowler B, et al. Hyperhomocysteinemia: an independent risk factor for vascular disease. N Engl J Med. 1991; 324:1149–55.
Article6. Selhub J, Miller JW. The pathogenesis of homocysteinemia: interruption of the coordinate regulation by S-adenosylmethionine of the remethylation and transsulfuration of homocysteine. Am J Clin Nutr. 1992; 55:131–8.
Article7. Wu YW, Lynch JK, Nelson KB. Perinatal arterial stroke: understanding mechanisms and outcomes. Semin Neurol. 2005; 25:424–34.
Article8. Lee HJ, Lim BC, Hwang H, Hong JS, Kim EK, Kim HS, et al. Clinical presentations and neurodevelopmental outcomes of perinatal stroke in preterm and term neonates: a case series. J Korean Med Sci. 2010; 25:888–94.
Article9. Kim HS, Lee JH, Lee CC, Nam SH, Hong E, Kim JH, et al. Early diagnosis of perinatal ischemic stroke based on clinical and radiological characteristics. J Korean Child Neurol Soc. 2011; 19:131–41.10. Wu YW, March WM, Croen LA, Grether JK, Escobar GJ, Newman TB. Perinatal stroke inchildren with motor impairment: a population based study. Pediatrics. 2004; 114:612–9.11. Nelson KB. Thrombophilias, perinatal stroke, and cerebral palsy. Clin Obstet Gynecol. 2006; 49:875–84.
Article12. Lynch JK, Han CJ, Nee LE, Nelson KB. Prothrombotic factors in children with stroke or porencephaly. Pediatrics. 2005; 116:447–53.
Article13. Kim SB, Lee GY, Seo JH, Kim HJ, Kim OJ, Jung BW, et al. The relationship between hyperhomocysteinemia and C677T MTHFR gene polymorphism in patients with ischemic stroke. J Korean Neurol Assoc. 2002; 20:346–52.14. Choi BO, Kim HJ, Cho HJ, Kim YK, Kim SH, Lee JH, et al. Association between MTHFR C677T polymorphism and ischemic stroke. J Korean Neurol Assoc. 2005; 23:607–13.15. Chango A, Potier De Courcy G, Boisson F, Guilland JC, Barbe F, Perrin MO, et al. 5,10-methylenetetrahydrofolate reductase common mutations, folate status and plasma homocysteine in healthy French adults of the Supplementation en Vitamines et Mineraux Antioxydants (SU.VI. MAX) cohort. Br J Nutr. 2000; 84:891–6.16. Clarke R, Frost C, Leroy V, Collins R. For the homocysteine lowering trialists collaboration. lowering blood homocysteine with folic acid based supplements: metaanalysis of randomised trials. BMJ. 1998; 316:894–8.17. Gemmati D, Previati M, Serino ML, Morateli S, Guerra S, Capitani S, et al. Low folate levels and thermolabile methy-lenetetrahydrofolate reductase as primary determinant of mild hyperhomocystinemia in normal and thromboembolic subjects. Arterioscker Thromb Vasc Biol. 1999; 19:1761–7.
Article18. Stanger O, Herrmann W, Pietrzik K, Fowler B, Geisel J, Dierkes J, et al. DACH-LIGA homocystein(german, austrian and swiss homocysteine society): consensus paper on the rational clinical use of homocysteine, folic acid and B-vitamins in cardiovascular and thrombotic disease: guidelines and recommendations. Clin Chem Lab Med. 2003; 41:1392–403.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Rare Case of Cerebral Sinovenous Thrombosis Associated with MTHFR A1298C and C677T Mutations
- Cerebral Venous Sinus Thrombosis with MTHFR C677T Heterozygous Mutation
- Methylenetetrahydrofolate Reductase Gene Polymorphism in Korean Patients with Migraine or Ischemic Stroke
- Case-Control Study for MTHFR and HFE Polymorphisms in Colorectal Cancer
- Serum Homocysteine Level and MTHFR C677T, A1298C Gene Polymorphism in Korean Schizophrenics