Early results with the Mutaf technique: a novel off-midline approach in pilonidal sinus surgery
- Affiliations
-
- 1Department of General Surgery, Medical Faculty of Hitit University, Çorum, Turkey. tayfunsahiner@gmail.com
- 2Department of General Surgery, Çorum Research and Training Hospital, Medical Faculty of Hitit University, Çorum, Turkey.
- 3Department of Statistics, School of Health, Hitit University, Çorum, Turkey.
- KMID: 2163066
- DOI: http://doi.org/10.4174/astr.2016.90.5.265
Abstract
- PURPOSE
The objective of the present study was to compare different off-midline techniques in terms of their advantages and disadvantages.
METHODS
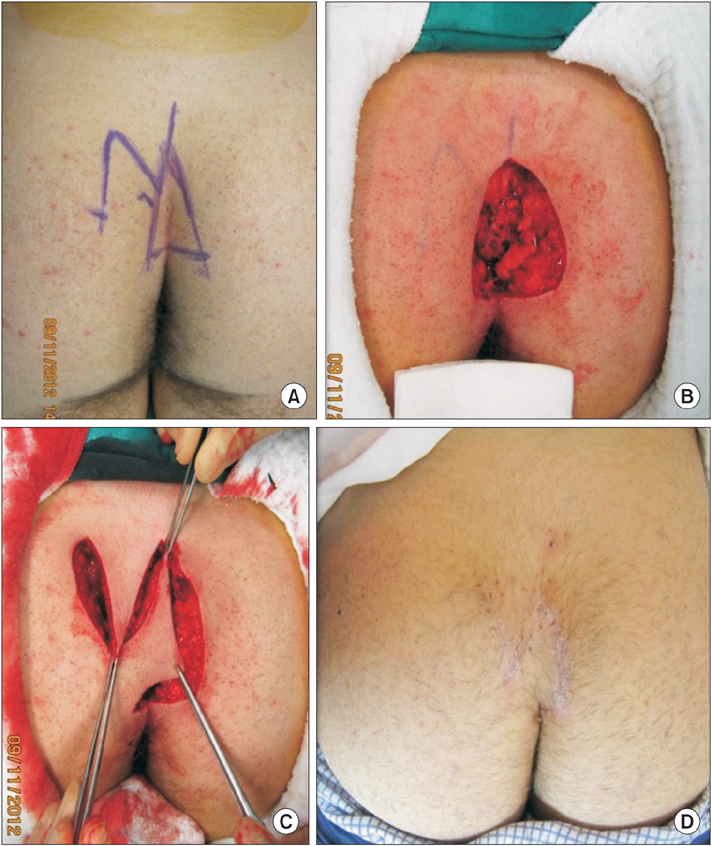
A total of 81 patients were included in this prospective, controlled, randomized study. Patients in group 1 were treated with the Limberg flap, and patients in group 2 were treated with Mutaf technique. Patients were followed up for 9 months postsurgically and assessed at regular intervals.
RESULTS
A total of 41 and 40 patients received surgical treatment with Limberg or Mutaf techniques, respectively. The 2 groups were similar in terms of age, gender, body mass index, and Tezel pilonidal sinus classification. Also, the 2 groups were comparable with regard to the frequency of preoperative discharge from the wound site, history of abscess formation, and the resultant antibiotic use. Early results showed similar recurrence rates and surgical-site complications between the 2 groups. Although a lower visual analogue scale score was found in group 2 at postoperative day 1, seroma persistence, time to withdrawal of surgical drains, and wound healing were more prolonged.
CONCLUSION
In this study, Mutaf technique was comparable to Limberg flap in the treatment of pilonidal sinus. Therefore, Mutaf technique may be offered as a viable surgical therapeutic option among off-midline closure approaches.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Evaluation of intradermal absorbable and mattress sutures to close pilonidal sinus wounds with Limberg flap: a prospective randomized comparative study
Kenan Çetin, Hasan Ediz Sikar, Aytaç Emre Kocaoğlu, Muhammet Fikri Kündeş, Mehmet Karahan, Levent Kaptanoğlu
Ann Surg Treat Res. 2018;94(2):88-93. doi: 10.4174/astr.2018.94.2.88.Inverse ‘D’ incision technique in treatment of pilonidal sinus disease; excision with minimal tissue loss, closure without tension and lateral location of the suture line
Sami Dogan, Fuat Cetin, Emin Gurleyik
Ann Surg Treat Res. 2019;97(5):261-265. doi: 10.4174/astr.2019.97.5.261.Comparative analysis of the same technique-the same surgeon approach in the surgical treatment of pilonidal sinus disease: a retrospective cohort study
Emin Kose, Mustafa Hasbahceci, Hasan Tonyali, Muslum Karagulle
Ann Surg Treat Res. 2017;93(2):82-87. doi: 10.4174/astr.2017.93.2.82.
Reference
-
1. Keskin AI, Polat Y, Duran E, Cetinkünar S, Zorlu M. Comparison of four different surgical techniques in cases with pilonidal sinus. Dicle Med J. 2014; 41:558–563.2. McCallum IJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ. 2008; 336:868–871.3. Mutaf M, Bekerecioglu M, Erkutlu I, Bulut O. A new technique for closure of large meningomyelocele defects. Ann Plast Surg. 2007; 59:538–543.4. Tezel E. A new classification according to navicular area concept for sacrococcygeal pilonidal disease. Colorectal Dis. 2007; 9:575–576.5. Mentes O, Bagci M, Bilgin T, Ozgul O, Ozdemir M. Limberg flap procedure for pilonidal sinus disease: results of 353 patients. Langenbecks Arch Surg. 2008; 393:185–189.6. Akinci OF, Bozer M, Uzunkoy A, Duzgun SA, Coskun A. Incidence and aetiological factors in pilonidal sinus among Turkish soldiers. Eur J Surg. 1999; 165:339–342.7. Horwood J, Hanratty D, Chandran P, Billings P. Primary closure or rhomboid excision and Limberg flap for the management of primary sacrococcygeal pilonidal disease? A meta-analysis of randomized controlled trials. Colorectal Dis. 2012; 14:143–151.8. Orhalmi J, Sotona O, Dusek T, Ferko A. Pilonidal sinus: possibilities surgical treatment. Rozhl Chir. 2014; 93:491–495.9. Guner A, Boz A, Ozkan OF, Ileli O, Kece C, Reis E. Limberg flap versus Bascom cleft lift techniques for sacrococcygeal pilonidal sinus: prospective, randomized trial. World J Surg. 2013; 37:2074–2080.10. Ozdemir H, Unal Ozdemir Z, Tayfun Sahiner I, Senol M. Whole natal cleft excision and flap : an alternative surgical method in extensive sacrococcygeal pilonidal sinus disease. Acta Chir Belg. 2014; 114:266–270.11. Lapid O, Rosenberg L, Cohen A. Meningomyelocele reconstruction with bilobed flaps. Br J Plast Surg. 2001; 54:570–572.12. Petersen S, Aumann G, Kramer A, Doll D, Sailer M, Hellmich G. Short-term results of Karydakis flap for pilonidal sinus disease. Tech Coloproctol. 2007; 11:235–240.13. Mentes BB, Leventoglu S, Cihan A, Tatlicioglu E, Akin M, Oguz M. Modified Limberg transposition flap for sacrococcygeal pilonidal sinus. Surg Today. 2004; 34:419–423.14. Topgul K, Ozdemir E, Kilic K, Gokbayir H, Ferahkose Z. Long-term results of limberg flap procedure for treatment of pilonidal sinus: a report of 200 cases. Dis Colon Rectum. 2003; 46:1545–1548.15. Petersen S, Koch R, Stelzner S, Wendlandt TP, Ludwig K. Primary closure techniques in chronic pilonidal sinus: a survey of the results of different surgical approaches. Dis Colon Rectum. 2002; 45:1458–1467.16. Cihan A, Mentes BB, Tatlicioglu E, Ozmen S, Leventoglu S, Ucan BH. Modified Limberg flap reconstruction compares favourably with primary repair for pilonidal sinus surgery. ANZ J Surg. 2004; 74:238–242.17. Akin M, Leventoglu S, Mentes BB, Bostanci H, Gokbayir H, Kilic K, et al. Comparison of the classic Limberg flap and modified Limberg flap in the treatment of pilonidal sinus disease: a retrospective analysis of 416 patients. Surg Today. 2010; 40:757–762.18. Ertan T, Koc M, Gocmen E, Aslar AK, Keskek M, Kilic M. Does technique alter quality of life after pilonidal sinus surgery? Am J Surg. 2005; 190:388–392.19. Jamal A, Shamim M, Hashmi F, Qureshi MI. Open excision with secondary healing versus rhomboid excision with Limberg transposition flap in the management of sacrococcygeal pilonidal disease. J Pak Med Assoc. 2009; 59:157–160.20. Mahdy T. Surgical treatment of the pilonidal disease: primary closure or flap reconstruction after excision. Dis Colon Rectum. 2008; 51:1816–1822.21. Daphan C, Tekelioglu MH, Sayilgan C. Limberg flap repair for pilonidal sinus disease. Dis Colon Rectum. 2004; 47:233–237.22. Tekin A. A simple modification with the Limberg flap for chronic pilonidal disease. Surgery. 2005; 138:951–953.23. Maghsoudi H, Nezami N, Ghamari AA. Ambulatory treatment of chronic pilonidal sinuses with lateral incision and primary suture. Can J Surg. 2011; 54:78–82.24. Yeghaneh RA, Faegheh A, Mina A. Body mass ındex and recurrence of pılonıdal sınus dısease. Iran J Surg. 2008; 16:85–90.25. Sievert H, Evers T, Matevossian E, Hoenemann C, Hoffmann S, Doll D. The influence of lifestyle (smoking and body mass index) on wound healing and longterm recurrence rate in 534 primary pilonidal sinus patients. Int J Colorectal Dis. 2013; 28:1555–1562.26. Poorghasem J, Mahoori A. The effect of body mass ındex on relapse of pilonidal sinus disease in adult patients. ZJRMS. 2012; 14:23–25.27. Alptekin H, Acar F, Sahın M, Yilmaz H, Kafali ME, Beyhan S. Specimen index may be a predictive factor for recurrence after primary closure of pilonidal disease. J Korean Surg Soc. 2012; 83:367–373.28. Karydakis GE. Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust N Z J Surg. 1992; 62:385–389.29. Tezel E, Bostanci H, Anadol AZ, Kurukahvecioglu O. Cleft lift procedure for sacrococcygeal pilonidal disease. Dis Colon Rectum. 2009; 52:135–139.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pilonidal Sinus Mimicking Inflammatory Epidermal Cyst
- Comparative analysis of the same technique-the same surgeon approach in the surgical treatment of pilonidal sinus disease: a retrospective cohort study
- Two Cases of Pilonidal Sinus
- Clinical Evaluation of Wide Excision and Simple Primary Closure of Pilonidal Sinus
- Pilonidal Cysts Occurring in the Sacrococcygeal Region and that were Misdiagnosed as a Simple Abscess