Ann Surg Treat Res.
2016 May;90(5):250-256. 10.4174/astr.2016.90.5.250.
Prognostic significance of intraoperative macroscopic serosal invasion finding when it shows a discrepancy in pathologic result gastric cancer
- Affiliations
-
- 1Department of Surgery, Chonbuk National University Medical School, Jeonju, Korea. happyhill@jbnu.co.kr
- 2Department of Pathology, Chonbuk National University Medical School, Jeonju, Korea.
- KMID: 2163064
- DOI: http://doi.org/10.4174/astr.2016.90.5.250
Abstract
- PURPOSE
Depth of wall invasion is an important prognostic factor in patients with gastric cancer, whereas the prognostic significance of intraoperative macroscopic serosal invasion (mSE) findings remain unclear when they show a discrepancy in pathologic findings. This study, therefore, assessed the prognostic significance of mSE.
METHODS
Data from cohort of 2,835 patients with resectable gastric cancer who underwent surgery between 1990 and 2010 were retrospectively reviewed.
RESULTS
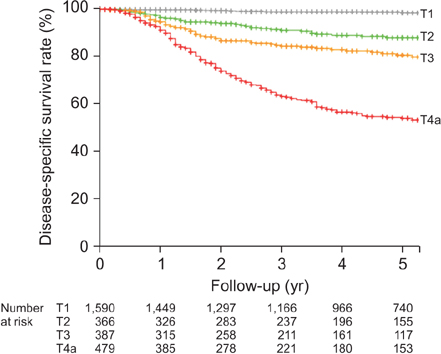
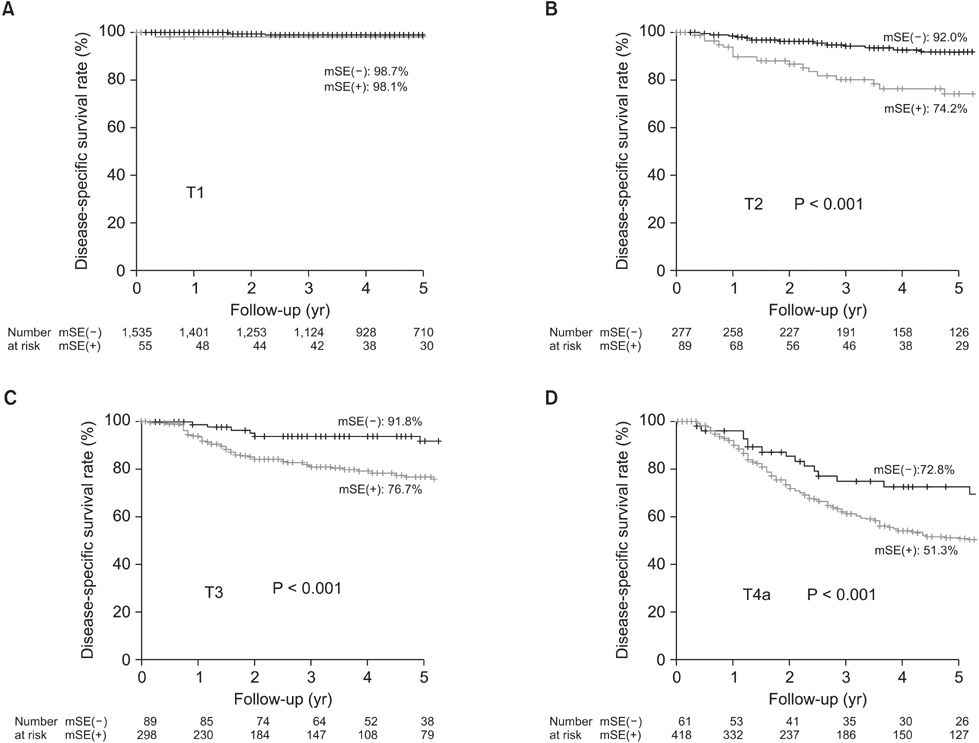
The overall accuracy of mSE and pathologic results was 83.4%. The accuracy of mSE was 75.5% in pT2. On the other hand, the accuracy of pT3 dropped to 24.5%. According to mSE findings (+/-), the 5-year disease-specific survival (DSS) rate differed significantly in patients with pT2 (+; 74.2% vs. -; 92.0%), pT3 (+; 76.7% vs. -; 91.8%) and pT4a (+; 51.3% vs. -; 72.8%) (P < 0.001 each), but not in patients with T1 tumor. Multivariate analysis showed that mSE findings (hazard ratio [HR], 2.275; 95% confidence interval [CI], 1.148-4.509), tumor depth (HR, 6.894; 95% CI, 2.325-20.437), nodal status (HR, 5.206; 95% CI, 2.298-11.791), distant metastasis (HR, 2.881; 95% CI, 1.388-6.209), radical resection (HR, 2.002; 95% CI, 1.017-3.940), and lymphatic invasion (HR, 2.713; 95% CI, 1.424-5.167) were independent predictors of 5-year DSS rate.
CONCLUSION
We observed considerable discrepancies between macroscopic and pathologic diagnosis of serosal invasion. However, macroscopic diagnosis of serosal invasion was independently prognostic of 5-year DSS. It suggests that because the pathologic results could not be perfect and the local inflammatory change with mSE(+) could affect survival, a combination of mSE(+/-) and pathologic depth may be predictive of prognosis in patients with gastric cancer.
Keyword
MeSH Terms
Figure
Reference
-
1. Takagane A, Terashima M, Abe K, Araya M, Irinoda T, Yonezawa H, et al. Evaluation of the ratio of lymph node metastasis as a prognostic factor in patients with gastric cancer. Gastric Cancer. 1999; 2:122–128.2. Lindsey H. Preoperative chemoradiotherapy shows promise in gastric cancer. Lancet Oncol. 2004; 5:519–519.3. Shimoyama S, Seto Y, Yasuda H, Mafune H, Kaminishi M. Concepts, rationale, and current outcomes of less invasive surgical strategies for early gastric cancer: data from a quarter-century of experience in a single institution. World J Surg. 2005; 59:58–65.4. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009; 59:225–249.5. Park do J, Kong SH, Lee HJ, Kim WH, Yang HK, Lee KU, et al. Subclassification of pT2 gastric adenocarcinoma according to depth of invasion (pT2a vs pT2b) and lymph node status (pN). Surgery. 2007; 141:757–763.6. Lee CC, Wu CW, Lo SS, Chen JH, Li AF, Hsieh MC, et al. Survival predictors in patients with node-negative gastric carcinoma. J Gastroenterol Hepatol. 2007; 22:1014–1018.7. Kunisaki C, Shimada H, Nomura M, Matsuda G, Otsuka Y, Ono H, et al. Clinical impact of metastatic lymph node ratioin advanced gastric cancer. Anticancer Res. 2005; 25(2B):1369–1375.8. Wang W, Sun XW, Li CF, Lv L, Li YF, Chen YB, et al. Comparison of the 6th and 7th editions of the UICC TNM staging system for gastric cancer: results of a Chinese single-institution study of 1,503 patients. Ann Surg Oncol. 2011; 18:1060–1067.9. Yoo CH, Noh SH, Shin DW, Choi SH, Min JS. Recurrence following curative resection for gastric carcinoma. Br J Surg. 2000; 87:236–242.10. Fujiwara Y, Okada K, Hanada H, Tamura S, Kimura Y, Fujita J, et al. The clinical importance of a transcription reverse-transcription concerted (TRC) diagnosis using peritoneal lavage fluids in gastric cancer with clinical serosal invasion: a prospective, multicenter study. Surgery. 2014; 155:417–423.11. Yasuda K, Shiraishi N, Inomata M, Shiroshita H, Izumi K, Kitano S. Prognostic significance of macroscopic serosal invasion in advanced gastric cancer. Hepatogastroenterology. 2007; 54:2028–2031.12. Ichiyoshi Y, Maehara Y, Tomisaki S, Oiwa H, Sakaguchi Y, Ohno S, et al. Macroscopic intraoperative diagnosis of serosal invasion and clinical outcome of gastric cancer: risk of underestimation. J Surg Oncol. 1995; 59:255–260.13. Jeong O, Ryu SY, Jeong MR, Sun JW, Park YK. Accuracy of macroscopic intraoperative diagnosis of serosal invasion and risk of over- and underestimation in gastric carcinoma. World J Surg. 2011; 35:2252–2258.14. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010; 17:1471–1474.15. Japanese Gastric Cancer Association. Japanese Classification of Gastric Carcinoma - 2nd English Edition -. Gastric Cancer. 1988; 1:10–24.16. Ribeiro U Jr, Gama-Rodrigues JJ, Safatle-Ribeiro AV, Bitelman B, Ibrahim RE, Ferreira MB, et al. Prognostic significance of intraperitoneal free cancer cells obtained by laparoscopic peritoneal lavage in patients with gastric cancer. J Gastrointest Surg. 1998; 2:244–249.17. Ikeguchi M, Oka A, Tsujitani S, Maeta M, Kaibara N. Relationship between area of serosal invasion and intraperitoneal free cancer cells in patients with gastric cancer. Anticancer Res. 1994; 14(5B):2131–2134.18. Sheen-Chen SM, Chou CW, Chen MC, Chen FC, Chen YS, Chen JJ. Adenocarcinoma in the middle third of the stomach: an evaluation for the prognostic significance of clinicopathological features. Hepatogastroenterology. 1997; 44:1488–1494.19. Kim DJ, Lee JH, Kim W. Impact of intra-operative macroscopic diagnosis of serosal invasion in pathological subserosal (pT3) gastric cancer. J Gastric Cancer. 2014; 14:252–258.20. Wang HH, Huang JY, Wang ZN, Sun Z, Li K, Xu HM. Macroscopic serosal classification as a prognostic index in radically resected stage pT3-pT4b gastric cancer. Ann Surg Oncol. 2016; 23:149–155.21. Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010; 140:883–899.22. Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010; 6:149–163.23. Shepherd NA, Baxter KJ, Love SB. The prognostic importance of peritoneal involvement in colonic cancer: a prospective evaluation. Gastroenterology. 1997; 112:1096–1102.24. Kaibara N, Iitsuka Y, Kimura A, Kobayashi Y, Hirooka Y, Nishidoi H, et al. Relationship between area of serosal invasion and prognosis in patients with gastric carcinoma. Cancer. 1987; 60:136–139.25. Bentrem D, Gerdes H, Tang L, Brennan M, Coit D. Clinical correlation of endoscopic ultrasonography with pathologic stage and outcome in patients undergoing curative resection for gastric cancer. Ann Surg Oncol. 2007; 14:1853–1859.26. Yamamoto M, Yoshinaga K, Matsuyama A, Tsutsui S, Ishida T. CEA/CA72-4 levels in peritoneal lavage fluid are predictive factors in patients with gastric carcinoma. J Cancer Res Clin Oncol. 2014; 140:607–612.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Macroscopic Serosal Invasion in Advanced Gastric Cancer
- Impact of Intraoperative Macroscopic Diagnosis of Serosal Invasion in Pathological Subserosal (pT3) Gastric Cancer
- The Prognostic Significance of the Preoperative Serum CEA, CA19-9 and AFP Levels in Gastric Cancer Patients
- Prognostic Value of Early Postoperative Intraperitoneal Chemotherapy for Gastric Cancer with Serosal Invasion
- Significance of Carcinoembryonic Antigen Levels in Peritoneal Washings for Gastric Cancer Patients