J Korean Orthop Assoc.
2016 Apr;51(2):125-132. 10.4055/jkoa.2016.51.2.125.
Preservation of Scaphoid in Scaphoid Nonunion Advanced Collapse Stage II and III
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea. Kangho56@yuhs.ac
- KMID: 2162046
- DOI: http://doi.org/10.4055/jkoa.2016.51.2.125
Abstract
- PURPOSE
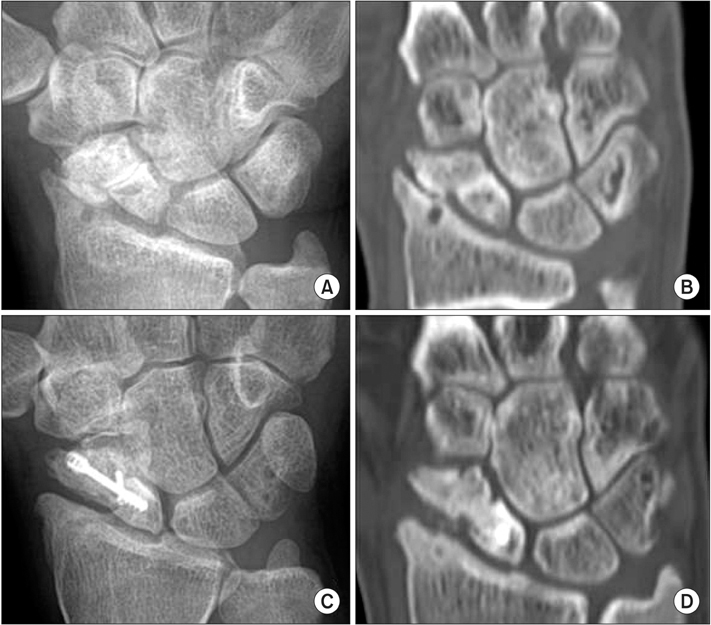
The purpose of this study is to investigate the outcome of open reduction and internal fixation with a headless screw and auto iliac bone graft for patients of scaphoid nonunion advanced collapse (SNAC) stage II and III.
MATERIALS AND METHODS
A retrospective analysis was conducted for 10 patients diagnosed with stage II or III SNAC, and consequently treated with open reduction and internal fixation with a headless screw and auto iliac bone graft with or without radial styloidectomy between 2010 and 2013. Radiographic results were evaluated by bone union, the scapholunate angle and lateral intrascaphoid angle. Clinical results were evaluated by range of motion, pain, grip strength, Mayo wrist score, and assessment of Maudsley.
RESULTS
All patients showed union after the operation. Final follow-up X-rays show smoothening of the articular surface with improvement of sclerotic lesions of the articular surface, cystic lesions and osteopenic lesions. Pain decreased after the operation compared with preoperative status, grip strength and Mayo wrist score showed significant improvement. Scapholunate angle and lateral intrascaphoid angle decreased after the operation, but it was not significant. According to assessment of Maudsley, among 10 cases, there were 4 excellent cases, 4 good cases and 2 fair cases.
CONCLUSION
Restoration of stability of scaphoid is important to SNAC stage II and III, open reduction and internal fixation with a headless screw and auto iliac bone graft shows satisfactory clinical and radiologic outcomes. Thus it is considered a recommendable operation.
Keyword
MeSH Terms
Figure
Reference
-
1. Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br. 1984; 66:114–123.2. Hove LM. Epidemiology of scaphoid fractures in Bergen, Norway. Scand J Plast Reconstr Surg Hand Surg. 1999; 33:423–426.3. Leventhal EL, Wolfe SW, Moore DC, Akelman E, Weiss AP, Crisco JJ. Interfragmentary motion in patients with scaphoid nonunion. J Hand Surg Am. 2008; 33:1108–1115.4. Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984; 9:358–365.5. Watson HK, Ryu J. Evolution of arthritis of the wrist. Clin Orthop Relat Res. 1986; 202:57–67.6. Strauch RJ. Scapholunate advanced collapse and scaphoid nonunion advanced collapse arthritis: update on evaluation and treatment. J Hand Surg Am. 2011; 36:729–735.7. Shah CM, Stern PJ. Scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist arthritis. Curr Rev Musculoskelet Med. 2013; 6:9–17.8. Trumble TE, Rafijah G, Alexander H, Waitayawinyu T. Scaphoidectomy and capsulodesis for SNAC or SLAC stage II. J Wrist Surg. 2012; 1:129–134.9. Malizos KN, Koutalos A, Papatheodorou L, Varitimidis S, Kontogeorgakos V, Dailiana Z. Vascularized bone grafting and distal radius osteotomy for scaphoid nonunion advanced collapse. J Hand Surg Am. 2014; 39:872–879.10. Kiefhaber TR. Management of scapholunate advanced collapse pattern of degenerative arthritis of the wrist. J Hand Surg Am. 2009; 34:1527–1530.11. Maudsley RH, Chen SC. Screw fixation in the management of the fractured carpal scaphoid. J Bone Joint Surg Br. 1972; 54:432–441.12. Hidaka Y, Nakamura R. Progressive patterns of degenerative arthritis in scaphoid nonunion demonstrated by threedimensional computed tomography. J Hand Surg Br. 1998; 23:765–770.13. Ruby LK, Stinson J, Belsky MR. The natural history of scaphoid non-union. A review of fifty-five cases. J Bone Joint Surg Am. 1985; 67:428–432.14. Sendher R, Ladd AL. The scaphoid. Orthop Clin North Am. 2013; 44:107–120.15. Moon ES, Dy CJ, Derman P, Vance MC, Carlson MG. Management of nonunion following surgical management of scaphoid fractures: current concepts. J Am Acad Orthop Surg. 2013; 21:548–557.16. Dacho A, Grundel J, Holle G, Germann G, Sauerbier M. Long-term results of midcarpal arthrodesis in the treatment of scaphoid nonunion advanced collapse (SNAC-Wrist) and scapholunate advanced collapse (SLAC-Wrist). Ann Plast Surg. 2006; 56:139–144.17. Kent ME, Rehmatullah NN, Young L, Chojnowski AJ. Scaphoid nonunion in the presence of a degenerate carpus: don't rush to salvage surgery. J Hand Surg Eur Vol. 2012; 37:56–60.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arthroscopic Bone Grafting and Kirschner-Wires Fixation for Scaphoid Nonunion
- Scaphoid Nonunion: Herbert Screw Fixation through Dorsal Approach
- Midcarpal Fusion with Excision of Scaphoid for Scapholunate Advanced Collapse ( SLAC )
- Flexor Pollicis Longus Tendon Rupture due to Scaphoid Nonunion
- The Effect of Smoking on the Outcomes of Vascularized Bone Graft Surgery in Scaphoid Nonunion through Meta-analysis