J Cerebrovasc Endovasc Neurosurg.
2016 Mar;18(1):42-47. 10.7461/jcen.2016.18.1.42.
Posterior Spinal Artery Aneurysm Presenting with Leukocytoclastic Vasculitis
- Affiliations
-
- 1New York University School of Medicine, New York, NY, USA.
- 2Department of Neurosurgery, New York University School of Medicine, New York, NY, USA. paul.huang@nyumc.org
- 3Department of Pathology, New York University School of Medicine, New York, NY, USA.
- 4Department of Radiology, New York University School of Medicine, New York, NY, USA.
- 5Department of Neurosurgery, Naval Medical Center Portsmouth, Portsmouth, VA, USA.
- KMID: 2161702
- DOI: http://doi.org/10.7461/jcen.2016.18.1.42
Abstract
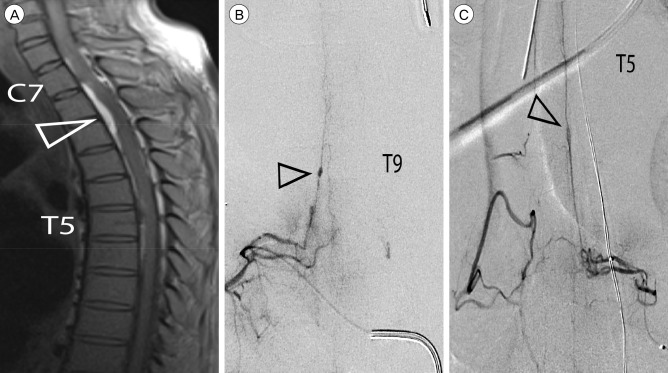
- Rupture of isolated posterior spinal artery (PSA) aneurysms is a rare cause of subarachnoid hemorrhage (SAH) that presents unique diagnostic challenges owing to a nuanced clinical presentation. Here, we report on the diagnosis and management of the first known case of an isolated PSA aneurysm in the context of leukocytoclastic vasculitis. A 53-year-old male presented to an outside institution with acute bilateral lower extremity paralysis 9 days after admission for recurrent cellulitis. Early magnetic resonance imaging was read as negative and repeat imaging 15 days after presentation revealed SAH and a compressive spinal subdural hematoma. Angiography identified a PSA aneurysm at T9, as well as other areas suspicious for inflammatory or post-hemorrhagic reactive changes. The patient underwent a multilevel laminectomy for clot evacuation and aneurysm resection to prevent future hemorrhage and to establish a diagnosis. The postoperative course was complicated by medical issues and led to the diagnosis of leukocytoclastic vasculitis that may have predisposed the patient to aneurysm development. Literature review reveals greater mortality for cervical lesions than thoracolumbar lesions and that the presence of meningitic symptoms portents better functional outcome than symptoms of cord compression. The outcome obtained in this case is consistent with outcomes reported in the literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Berlis A, Scheufler KM, Schmahl C, Rauer S, Götz F, Schumacher M. Solitary spinal artery aneurysms as a rare source of spinal subarachnoid hemorrhage: potential etiology and treatment strategy. AJNR Am J Neuroradiol. 2005; 2. 26(2):405–410. PMID: 15709145.2. Biondi A, Merland JJ, Hodes JE, Aymard A, Reizine D. Aneurysms of spinal arteries associated with intramedullary arteriovenous malformations. II. Results of AVM endovascular treatment and hemodynamic considerations. AJNR Am J Neuroradiol. 1992; May-Jun. 13(3):923–931. PMID: 1590192.3. Cavusoglu H, Ozdilmac A, Sahin Y, Aydin Y. Isolated posterior spinal artery aneurysm causing intracranial acute subarachnoidal hemorrhage. Acta Neurochir (Wien). 2010; 4. 152(4):721–724. PMID: 19693431.4. Doppman JL, Di Chiro G, Glancy DL. Collateral circulation through dilated spinal cord arteries in aortic coarctation and extraspinal arteriovenous shunts. An arteriographic study. Clin Radiol. 1969; 4. 20(2):192–197. PMID: 5781764.
Article5. Fody EP, Netsky MG, Mrak RE. Subarachnoid spinal hemorrhage in a case of systemic lupus erythematosus. Arch Neurol. 1980; 3. 37(3):173–174. PMID: 7356425.
Article6. Geibprasert S, Krings T, Apitzsch J, Reinges MH, Nolte KW, Hans FJ. Subarachnoid hemorrhage following posterior spinal artery aneurysm. A case report and review of the literature. Interv Neuroradiol. 2010; 6. 16(2):183–190. PMID: 20642894.7. Goto Y, Kamijyo Y, Yonekawa Y, Kikuchi H. Ruptured aneurysm of the posterior spinal artery of the upper cervical spinal cord: case report. Neurosurgery. 1988; 3. 22(3):558–560. PMID: 3362323.
Article8. Handa T, Suzuki Y, Saito K, Sugita K, Patel SJ. Isolated intramedullary spinal artery aneurysm presenting with quadriplegia. Case report. J Neurosurg. 1992; 7. 77(1):148–150. PMID: 1607957.9. Henson RA, Croft PB. Spontaneous spinal subarachnoid haemorrhage. Q J Med. 1956; 1. 25(97):53–66. PMID: 13323242.10. Johnson J, Patel S, Saraf-Lavi E, Aziz-Sultan MA, Yavagal DR. Posterior spinal artery aneurysm rupture after 'Ecstasy' abuse. J Neurointerv Surg. 2015; 7. 7(7):e23. PMID: 25006043.
Article11. Kim HJ, Choi IS. Dissecting aneurysm of the posterior spinal artery: case report and review of the literature. Neurosurgery. 2012; 9. 71(3):E749–E756. discussion E756PMID: 22592330.12. Kocak A, Ates O, Cayli SR, Sarac K. Isolated posterior spinal artery aneurysm. Br J Neurosurg. 2006; 8. 20(4):241–244. PMID: 16954077.13. Kossorotoff M, Touze E, Godon-Hardy S, Serre I, Mateus C, Mas JL, et al. Cerebral vasculopathy with aneurysm formation in HIV-infected young adults. Neurology. 2006; 4. 66(7):1121–1122. PMID: 16606935.
Article14. Massand MG, Wallace RC, Gonzalez LF, Zabramski JM, Spetzler RF. Subarachnoid hemorrhage due to isolated spinal artery aneurysm in four patients. AJNR Am J Neuroradiol. 2005; 10. 26(9):2415–2419. PMID: 16219857.15. Nemecek AN, Sviri G, Hevner R, Ghodke B, Britz GW. Dissecting aneurysm of the thoracic posterior spinal artery. Case illustration. J Neurosurg Spine. 2006; 12. 5(6):555. PMID: 17176024.16. Shankar JJ, terBrugge K, Krings T. Subarachnoid hemorrhage following posterior spinal artery aneurysm rupture. Can J Neurol Sci. 2012; 7. 39(4):531–532. PMID: 22728865.
Article17. Takahashi JC, Sakai N, Iihara K, Sakai H, Higashi T, Kogure S, et al. Subarachnoid hemorrhage from a ruptured anterior cerebral artery aneurysm caused by polyarteritis nodosa. Case report. J Neurosurg. 2002; 1. 96(1):132–134. PMID: 11794594.18. Tanweer O, Woldenberg R, Zwany S, Setton A. Endovascular obliteration of a ruptured posterior spinal artery pseudoaneurysm. J Neurosurg Spine. 2012; 10. 17(4):334–336. PMID: 22881040.
Article19. Weir B. Unruptured intracranial aneurysms: a review. J Neurosurg. 2002; 1. 96(1):3–42. PMID: 11794601.
Article20. Yoong MF, Blumbergs PC, North JB. Primary (granulomatous) angiitis of the central nervous system with multiple aneurysms of spinal arteries. Case report. J Neurosurg. 1993; 10. 79(4):603–607. PMID: 8410233.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Annular Leukocytoclastic Vasculitis
- A Case of Leukocytoclastic Vasculitis Following COVID-19 Vaccination
- Warfarin-induced Leukocytoclastic Vasculitis
- A Case of Leukocytoclastic Vasculitis Induced by Leuprolide Acetate
- A Case of Leukocytoclastic Vasculitis Associated with Pulmonary Tuberculosis