J Gynecol Oncol.
2015 Jul;26(3):171-178. 10.3802/jgo.2015.26.3.171.
Cost-effectiveness of para-aortic lymphadenectomy before chemoradiotherapy in locally advanced cervical cancer
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Institute of Women's Life Medical Science, Yonsei University College of Medicine, Seoul, Korea.
- 2Institute of Health and Environment, Seoul National University Graduate School of Public Health, Seoul, Korea.
- 3Department of Health Policy and Management, Seoul National University Graduate School of Public Health, Seoul, Korea.
- 4Korean Health Promotion Foundation, Seoul, Korea.
- 5Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 6Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea.
- 7Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea. khjae@ snu.ac.kr
- 8Department of Family Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2160802
- DOI: http://doi.org/10.3802/jgo.2015.26.3.171
Abstract
OBJECTIVE
To evaluate the cost-effectiveness of nodal staging surgery before chemoradiotherapy (CRT) for locally advanced cervical cancer in the era of positron emission tomography/computed tomography (PET/CT).
METHODS
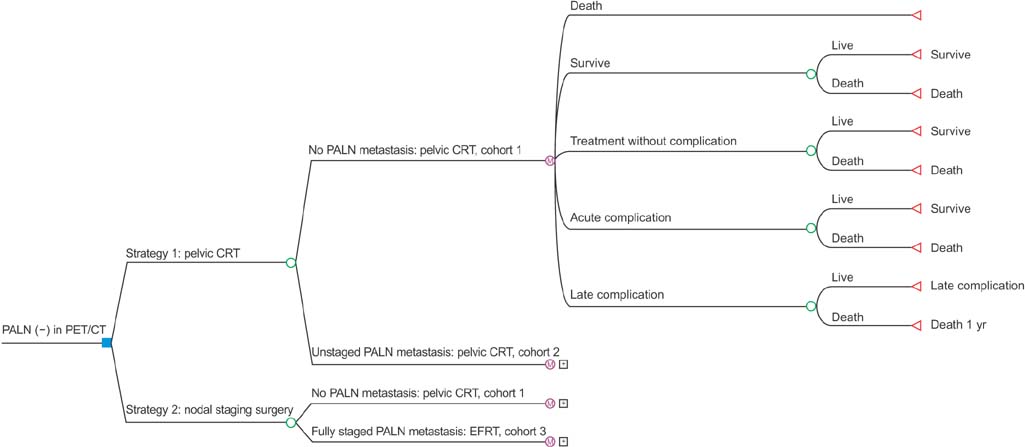
A modified Markov model was constructed to evaluate the cost-effectiveness of para-aortic staging surgery before definite CRT when no uptake is recorded in the para-aortic lymph nodes (PALN) on PET/CT. Survival and complication rates were estimated based on the published literature. Cost data were obtained from the Korean Health Insurance Review and Assessment Service. Strategies were compared using an incremental cost-effectiveness ratio (ICER). Sensitivity analyses were performed, including estimates for the performance of PET/CT, postoperative complication rate, and varying survival rates according to the radiation field.
RESULTS
We compared two strategies: strategy 1, pelvic CRT for all patients; and strategy 2, nodal staging surgery followed by extended-field CRT when PALN metastasis was found and pelvic CRT otherwise. The ICER for strategy 2 compared to strategy 1 was $19,505 per quality-adjusted life year (QALY). Under deterministic sensitivity analyses, the model was relatively sensitive to survival reduction in patients who undergo pelvic CRT alone despite having occult PALN metastasis. A probabilistic sensitivity analysis demonstrated the robustness of the case results, with a 91% probability of cost-effectiveness at the willingness-to-pay thresholds of $60,000/QALY.
CONCLUSION
Nodal staging surgery before definite CRT may be cost-effective when PET/CT imaging shows no evidence of PALN metastasis. Prospective trials are warranted to transfer these results to guidelines.
Keyword
MeSH Terms
-
Chemoradiotherapy/*economics
Combined Modality Therapy/economics
Cost-Benefit Analysis
Female
Humans
Laparoscopy/economics
Lymph Node Excision/*economics/methods
Lymphatic Metastasis
Markov Chains
Multimodal Imaging/economics
Neoplasm Staging
Positron-Emission Tomography/economics
Quality of Life
Quality-Adjusted Life Years
Tomography, X-Ray Computed/economics
Uterine Cervical Neoplasms/*economics/therapy
Figure
Reference
-
1. National Comprehensive Cancer Center (NCCN). NCCN Clinical Practice Guidelines in Oncology: Cervical Cancer [Internet]. Fort Washington, PA: National Comprehensive Cancer Network;c2014. cited 2015 Jun 10. Available from: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#cervical.2. Lai CH, Huang KG, Hong JH, Lee CL, Chou HH, Chang TC, et al. Randomized trial of surgical staging (extraperitoneal or laparoscopic) versus clinical staging in locally advanced cervical cancer. Gynecol Oncol. 2003; 89:160–167.3. Gold MA, Tian C, Whitney CW, Rose PG, Lanciano R. Surgical versus radiographic determination of para-aortic lymph node metastases before chemoradiation for locally advanced cervical carcinoma: a Gynecologic Oncology Group Study. Cancer. 2008; 112:1954–1963.4. Brockbank E, Kokka F, Bryant A, Pomel C, Reynolds K. Pre-treatment surgical para-aortic lymph node assessment in locally advanced cervical cancer. Cochrane Database Syst Rev. 2013; 3:CD008217.5. Choi HJ, Ju W, Myung SK, Kim Y. Diagnostic performance of computer tomography, magnetic resonance imaging, and positron emission tomography or positron emission tomography/computer tomography for detection of metastatic lymph nodes in patients with cervical cancer: meta-analysis. Cancer Sci. 2010; 101:1471–1479.6. Gouy S, Morice P, Narducci F, Uzan C, Gilmore J, Kolesnikov-Gauthier H, et al. Nodal-staging surgery for locally advanced cervical cancer in the era of PET. Lancet Oncol. 2012; 13:e212–e220.7. Lee JY. Management of cervical cancer patients with isolated paraaortic lymph node metastases. J Gynecol Oncol. 2013; 24:382–383.8. Eifel PJ, Winter K, Morris M, Levenback C, Grigsby PW, Cooper J, et al. Pelvic irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation for high-risk cervical cancer: an update of radiation therapy oncology group trial (RTOG) 90-01. J Clin Oncol. 2004; 22:872–880.9. Keys HM, Bundy BN, Stehman FB, Muderspach LI, Chafe WE, Suggs CL 3rd, et al. Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N Engl J Med. 1999; 340:1154–1161.10. Rose PG, Ali S, Watkins E, Thigpen JT, Deppe G, Clarke-Pearson DL, et al. Long-term follow-up of a randomized trial comparing concurrent single agent cisplatin, cisplatin-based combination chemotherapy, or hydroxyurea during pelvic irradiation for locally advanced cervical cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2007; 25:2804–2810.11. Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999; 340:1144–1153.12. Leblanc E, Narducci F, Frumovitz M, Lesoin A, Castelain B, Baranzelli MC, et al. Therapeutic value of pretherapeutic extraperitoneal laparoscopic staging of locally advanced cervical carcinoma. Gynecol Oncol. 2007; 105:304–311.13. Lim MC, Bae J, Park JY, Lim S, Kang S, Seo SS, et al. Experiences of pretreatment laparoscopic surgical staging in patients with locally advanced cervical cancer: results of a prospective study. J Gynecol Oncol. 2008; 19:123–128.14. Lesnock JL, Farris C, Beriwal S, Krivak TC. Upfront treatment of locally advanced cervical cancer with intensity modulated radiation therapy compared to four-field radiation therapy: a cost-effectiveness analysis. Gynecol Oncol. 2013; 129:574–579.15. Konski A, Watkins-Bruner D, Feigenberg S, Hanlon A, Kulkarni S, Beck JR, et al. Using decision analysis to determine the cost-effectiveness of intensity-modulated radiation therapy in the treatment of intermediate risk prostate cancer. Int J Radiat Oncol Biol Phys. 2006; 66:408–415.16. Jewell EL, Smrtka M, Broadwater G, Valea F, Davis DM, Nolte KC, et al. Utility scores and treatment preferences for clinical early-stage cervical cancer. Value Health. 2011; 14:582–586.17. Asukai Y, Valladares A, Camps C, Wood E, Taipale K, Arellano J, et al. Cost-effectiveness analysis of pemetrexed versus docetaxel in the second-line treatment of non-small cell lung cancer in Spain: results for the non-squamous histology population. BMC Cancer. 2010; 10:26.18. Gold MR, Franks P, McCoy KI, Fryback DG. Toward consistency in cost-utility analyses: using national measures to create conditionspecific values. Med Care. 1998; 36:778–792.19. Ernst EJ, Ernst ME, Hoehns JD, Bergus GR. Women's quality of life is decreased by acute cystitis and antibiotic adverse effects associated with treatment. Health Qual Life Outcomes. 2005; 3:45.20. El-Gazzaz G, Hull TL, Mignanelli E, Hammel J, Gurland B, Zutshi M. Obstetric and cryptoglandular rectovaginal fistulas: long-term surgical outcome; quality of life; and sexual function. J Gastrointest Surg. 2010; 14:1758–1763.21. Ahn JH, Kim YH. Cost-effectiveness analysis of HPV vaccine. Seoul: National Evidence-based Coolaborating Agency;2012.22. Yi JJ, Yoo WK, Kim SY, Kim KK, Yi SW. Medical expenses by site of cancer and survival time among cancer patients in the last one year of life. J Prev Med Public Health. 2005; 38:9–15.23. World Health Organization. World health report. Geneva: World Health Organization;2002.24. Eichler HG, Kong SX, Gerth WC, Mavros P, Jonsson B. Use of cost-effectiveness analysis in health-care resource allocation decision-making: how are cost-effectiveness thresholds expected to emerge? Value Health. 2004; 7:518–528.25. Gouy S, Morice P, Narducci F, Uzan C, Martinez A, Rey A, et al. Prospective multicenter study evaluating the survival of patients with locally advanced cervical cancer undergoing laparoscopic paraaortic lymphadenectomy before chemoradiotherapy in the era of positron emission tomography imaging. J Clin Oncol. 2013; 31:3026–3033.26. Occelli B, Narducci F, Lanvin D, Querleu D, Coste E, Castelain B, et al. De novo adhesions with extraperitoneal endosurgical para-aortic lymphadenectomy versus transperitoneal laparoscopic para-aortic lymphadenectomy: a randomized experimental study. Am J Obstet Gynecol. 2000; 183:529–533.27. Hong DG, Park NY, Chong GO, Cho YL, Park IS, Lee YS. Survival benefit of laparoscopic surgical staging-guided radiation therapy in locally advanced cervical cancer. J Gynecol Oncol. 2010; 21:163–168.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopy-assisted gastrectomy with para-aortic lymphadenectomy after palliative chemotherapy for advanced gastric cancer with isolated para-aortic lymph node metastasis
- Laparoscopic pelvic and para-aortic lymphadenectomy
- Is Prophylactic Irradiation to Para-aortic Lymph Nodes in Locally Advanced Cervical Cancer Necessary?
- A new technique of laparoscopic para-aortic lymphadenectomy optimizes perioperative outcome
- The Role of the Para-aortic Lymphadenectomy in Epithelial Ovarian Cancer