Korean J Radiol.
2015 Oct;16(5):1038-1046. 10.3348/kjr.2015.16.5.1038.
T2-Weighted Liver MRI Using the MultiVane Technique at 3T: Comparison with Conventional T2-Weighted MRI
- Affiliations
-
- 1Department of Radiology, Myongji Hospital, Seonam University College of Medicine, Goyang 10475, Korea.
- 2Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 06351, Korea. jmyr@dreamwiz.com
- 3Philips Healthcare Korea, Philips, Seoul 04342, Korea.
- 4Biostatistics and Clinical Epidemiology Center, Samsung Medical Center, Seoul 06351, Korea.
- KMID: 2160771
- DOI: http://doi.org/10.3348/kjr.2015.16.5.1038
Abstract
OBJECTIVE
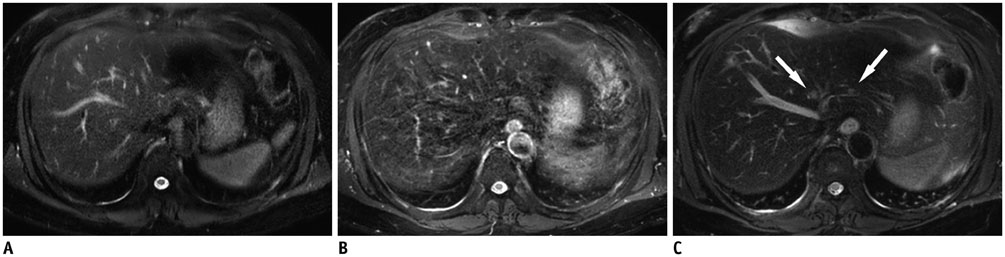
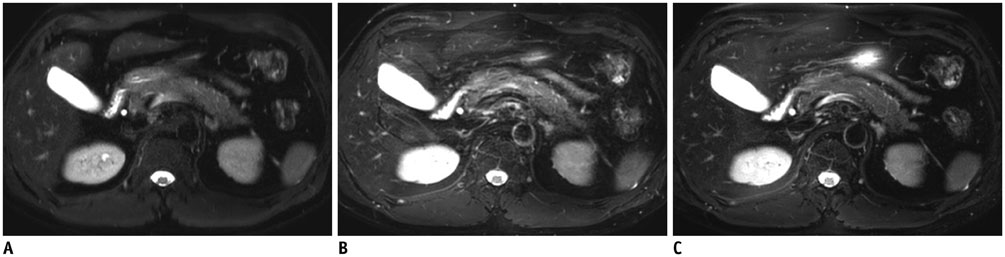
To assess the value of applying MultiVane to liver T2-weighted imaging (T2WI) compared with conventional T2WIs with emphasis on detection of focal liver lesions.
MATERIALS AND METHODS
Seventy-eight patients (43 men and 35 women) with 86 hepatic lesions and 20 pancreatico-biliary diseases underwent MRI including T2WIs acquired using breath-hold (BH), respiratory-triggered (RT), and MultiVane technique at 3T. Two reviewers evaluated each T2WI with respect to artefacts, organ sharpness, and conspicuity of intrahepatic vessels, hilar duct, and main lesion using five-point scales, and made pairwise comparisons between T2WI sequences for these categories. Diagnostic accuracy (Az) and sensitivity for hepatic lesion detection were evaluated using alternative free-response receiver operating characteristic analysis.
RESULTS
MultiVane T2WI was significantly better than BH-T2WI or RT-T2WI for organ sharpness and conspicuity of intrahepatic vessels and main lesion in both separate reviews and pairwise comparisons (p < 0.001). With regard to motion artefacts, MultiVane T2WI or BH-T2WI was better than RT-T2WI (p < 0.001). Conspicuity of hilar duct was better with BH-T2WI than with MultiVane T2WI (p = 0.030) or RT-T2WI (p < 0.001). For detection of 86 hepatic lesions, sensitivity (mean, 97.7%) of MultiVane T2WI was significantly higher than that of BH-T2WI (mean, 89.5%) (p = 0.008) or RT-T2WI (mean, 84.9%) (p = 0.001).
CONCLUSION
Applying the MultiVane technique to T2WI of the liver is a promising approach to improving image quality that results in increased detection of focal liver lesions compared with conventional T2WI.
MeSH Terms
Figure
Reference
-
1. Hussain HK, Syed I, Nghiem HV, Johnson TD, Carlos RC, Weadock WJ, et al. T2-weighted MR imaging in the assessment of cirrhotic liver. Radiology. 2004; 230:637–644.2. Kim YK, Lee YH, Kim CS, Han YM. Added diagnostic value of T2-weighted MR imaging to gadolinium-enhanced three-dimensional dynamic MR imaging for the detection of small hepatocellular carcinomas. Eur J Radiol. 2008; 67:304–310.3. Maetani Y, Itoh K, Watanabe C, Shibata T, Ametani F, Yamabe H, et al. MR imaging of intrahepatic cholangiocarcinoma with pathologic correlation. AJR Am J Roentgenol. 2001; 176:1499–1507.4. McFarland EG, Mayo-Smith WW, Saini S, Hahn PF, Goldberg MA, Lee MJ. Hepatic hemangiomas and malignant tumors: improved differentiation with heavily T2-weighted conventional spin-echo MR imaging. Radiology. 1994; 193:43–47.5. Reinig JW. Breath-hold fast spin-echo MR imaging of the liver: a technique for high-quality T2-weighted images. Radiology. 1995; 194:303–304.6. Tang Y, Yamashita Y, Namimoto T, Abe Y, Takahashi M. Liver T2-weighted MR imaging: comparison of fast and conventional half-Fourier single-shot turbo spin-echo, breath-hold turbo spin-echo, and respiratory-triggered turbo spin-echo sequences. Radiology. 1997; 203:766–772.7. Augui J, Vignaux O, Argaud C, Coste J, Gouya H, Legmann P. Liver: T2-weighted MR imaging with breath-hold fast-recovery optimized fast spin-echo compared with breath-hold half-Fourier and non-breath-hold respiratory-triggered fast spin-echo pulse sequences. Radiology. 2002; 223:853–859.8. Hirokawa Y, Isoda H, Maetani YS, Arizono S, Shimada K, Togashi K. Evaluation of motion correction effect and image quality with the periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER) (BLADE) and parallel imaging acquisition technique in the upper abdomen. J Magn Reson Imaging. 2008; 28:957–962.9. Hirokawa Y, Isoda H, Maetani YS, Arizono S, Shimada K, Togashi K. MRI artifact reduction and quality improvement in the upper abdomen with PROPELLER and prospective acquisition correction (PACE) technique. AJR Am J Roentgenol. 2008; 191:1154–1158.10. Kiryu S, Watanabe M, Kabasawa H, Akahane M, Aoki S, Ohtomo K. Evaluation of super paramagnetic iron oxide-enhanced diffusion-weighted PROPELLER T2-fast spin echo magnetic resonance imaging: preliminary experience. J Comput Assist Tomogr. 2006; 30:197–200.11. Klessen C, Asbach P, Kroencke TJ, Fischer T, Warmuth C, Stemmer A, et al. Magnetic resonance imaging of the upper abdomen using a free-breathing T2-weighted turbo spin echo sequence with navigator triggered prospective acquisition correction. J Magn Reson Imaging. 2005; 21:576–582.12. Lee SS, Byun JH, Hong HS, Park SH, Won HJ, Shin YM, et al. Image quality and focal lesion detection on T2-weighted MR imaging of the liver: comparison of two high-resolution free-breathing imaging techniques with two breath-hold imaging techniques. J Magn Reson Imaging. 2007; 26:323–330.13. Pipe JG. Motion correction with PROPELLER MRI: application to head motion and free-breathing cardiac imaging. Magn Reson Med. 1999; 42:963–969.14. Zech CJ, Herrmann KA, Huber A, Dietrich O, Stemmer A, Herzog P, et al. High-resolution MR-imaging of the liver with T2-weighted sequences using integrated parallel imaging: comparison of prospective motion correction and respiratory triggering. J Magn Reson Imaging. 2004; 20:443–450.15. Hirokawa Y, Isoda H, Maetani YS, Arizono S, Shimada K, Okada T, et al. Hepatic lesions: improved image quality and detection with the periodically rotated overlapping parallel lines with enhanced reconstruction technique--evaluation of SPIO-enhanced T2-weighted MR images. Radiology. 2009; 251:388–397.16. Haneder S, Dinter D, Gutfleisch A, Schoenberg SO, Michaely HJ. Image quality of T2w-TSE of the abdomen and pelvis with Cartesian or BLADE-type k-space sampling: a retrospective interindividual comparison study. Eur J Radiol. 2011; 79:177–182.17. Rosenkrantz AB, Mannelli L, Mossa D, Babb JS. Breath-hold T2-weighted MRI of the liver at 3T using the BLADE technique: impact upon image quality and lesion detection. Clin Radiol. 2011; 66:426–433.18. Bruix J, Sherman M;. Management of hepatocellular carcinoma: an update. Hepatology. 2011; 53:1020–1022.19. Deák Z, Grimm JM, Treitl M, Geyer LL, Linsenmaier U, Körner M, et al. Filtered back projection, adaptive statistical iterative reconstruction, and a model-based iterative reconstruction in abdominal CT: an experimental clinical study. Radiology. 2013; 266:197–206.20. Obuchowski NA. Nonparametric analysis of clustered ROC curve data. Biometrics. 1997; 53:567–578.21. Kwak M, Um SW, Jung SH. Comparison of operational characteristics for binary tests with clustered data. Stat Med. 2015; 05. 20. [Epub]. DOI: 10.1002/sim.6485.22. Tamada T, Ito K, Ueki A, Kanki A, Higaki A, Higashi H, et al. Peripheral low intensity sign in hepatic hemangioma: diagnostic pitfall in hepatobiliary phase of Gd-EOB-DTPA-enhanced MRI of the liver. J Magn Reson Imaging. 2012; 35:852–858.23. Tamada T, Ito K, Yamamoto A, Sone T, Kanki A, Tanaka F, et al. Hepatic hemangiomas: evaluation of enhancement patterns at dynamic MRI with gadoxetate disodium. AJR Am J Roentgenol. 2011; 196:824–830.24. Heverhagen JT. Noise measurement and estimation in MR imaging experiments. Radiology. 2007; 245:638–639.25. Kim YK, Kwak HS, Kim CS, Han YM. Detection and characterization of focal hepatic tumors: a comparison of T2-weighted MR images before and after the administration of gadoxectic acid. J Magn Reson Imaging. 2009; 30:437–443.26. Song KD, Kim YK, Lee WJ, Lee MW, Park MJ, Hwang J, et al. Detection and characterization of small focal hepatic lesions (≤ 2.5 cm in diameter): a comparison of diffusion-weighted images before and after administration of gadoxetic acid disodium at 3.0T. Acta Radiol. 2012; 53:485–493.27. Muhi A, Ichikawa T, Motosugi U, Sou H, Sano K, Araki T. Diffusion- and T2-weighted MR imaging of the liver: effect of intravenous administration of gadoxetic acid disodium. Magn Reson Med Sci. 2012; 11:185–191.28. Jeong YY, Mitchell DG, Holland GA. Liver lesion conspicuity: T2-weighted breath-hold fast spin-echo MR imaging before and after gadolinium enhancement--initial experience. Radiology. 2001; 219:455–460.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Utility of Limited T2-Weighted-Only Lumbar Spine MRI in Pain Intervention Clinics
- Gradient-Echo MRI in Defining the Severity of Cerebral Fat Embolism
- The relative signal intensity of retrodiscal tissue in TMJ using a T2-weighted MRI
- The Usefulness of Diffusion: Weighted Magnetic Resonance Image in the Diagnosis of Neonatal Seizure
- Efficacy of IVIRI for Therapeutic Evaluation of Bone Lymphoma