Pediatr Gastroenterol Hepatol Nutr.
2016 Mar;19(1):20-28. 10.5223/pghn.2016.19.1.20.
Foreign Body Ingestion in Children: Should Button Batteries in the Stomach Be Urgently Removed?
- Affiliations
-
- 1Department of Pediatrics, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea. shimjo@korea.ac.kr
- KMID: 2160472
- DOI: http://doi.org/10.5223/pghn.2016.19.1.20
Abstract
- PURPOSE
Foreign body (FB) ingestion is common in children, and button battery (BB) ingestion has been increasing in recent years. This study was to identify factors related to outcomes of FB ingestion, particularly BBs in the stomach. We evaluated whether the current recommendations are appropriate and aimed to suggest indications for endoscopic removal of BB in the stomach in young children.
METHODS
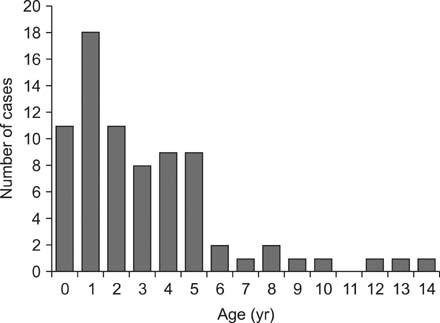
We investigated patient age, shape, size, location of FBs, spontaneous passage time and resulting complications among 76 children. We observed types, size, location of BB and outcomes, and analyzed their associations with complications.
RESULTS
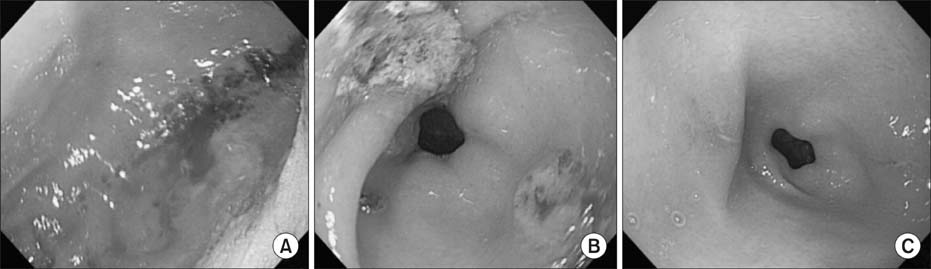
Coins and BB were the two most common FBs. Their shapes and sizes were not associated with the spontaneous passage time. Size, spontaneous passage time, and age were also not associated with any specific complications. For BB ingestion, all 5 cases with lithium batteries (≥1.5 cm, 3 V) presented moderate to major complications in the esophagus and stomach without any symptoms, even when the batteries were in the stomach and beyond the duodenum, while no complications were noted in 7 cases with alkaline batteries (<1.5 cm, 1.5 V) (p=0.001). All endoscopies were conducted within 24 hours after ingestion.
CONCLUSION
The type and voltage of the battery should be considered when determining whether endoscopy is required to remove a BB in the stomach. For lithium battery ingestion in young children, urgent endoscopic removal might be important in order to prevent complications, even if the child is asymptomatic and the battery is smaller than 2 cm.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Foreign Body Removal in Children Using Foley Catheter or Magnet Tube from Gastrointestinal Tract
Jae Young Choe, Byung-Ho Choe
Pediatr Gastroenterol Hepatol Nutr. 2019;22(2):132-141. doi: 10.5223/pghn.2019.22.2.132.Migrating foreign body in an adult bronchus: An aspirated denture
Binita Panigrahi, Nishant Sahay, Devi P Samaddar, Abhishek Chatterjee
J Dent Anesth Pain Med. 2018;18(4):267-270. doi: 10.17245/jdapm.2018.18.4.267.Foreign Body Ingestion in Children
Ji Hyuk Lee
Clin Endosc. 2018;51(2):129-136. doi: 10.5946/ce.2018.039.
Reference
-
1. Arana A, Hauser B, Hachimi-Idrissi S, Vandenplas Y. Management of ingested foreign bodies in childhood and review of the literature. Eur J Pediatr. 2001; 160:468–472.
Article2. Webb WA. Management of foreign bodies of the upper gastrointestinal tract. Gastroenterology. 1988; 94:204–216.
Article3. Kirkham EN, Kane M, Paul SP. Foreign body ingestion in children. Community Pract. 2015; 88:45–48.4. Lee JH, Nam SH, Lee JH, Lee HJ, Choe YH. Spontaneous passage of gastrointestinal foreign bodies in children. Korean J Pediatr Gastroenterol Nutr. 2007; 10:157–165.
Article5. Litovitz T, Schmitz BF. Ingestion of cylindrical and button batteries: an analysis of 2382 cases. Pediatrics. 1992; 89:747–757.
Article6. Litovitz TL. Button battery ingestions. A review of 56 cases. JAMA. 1983; 249:2495–2500.
Article7. Maves MD, Carithers JS, Birck HG. Esophageal burns secondary to disc battery ingestion. Ann Otol Rhinol Laryngol. 1984; 93:364–369.
Article8. Honda S, Shinkai M, Usui Y, Hirata Y, Kitagawa N, Take H, et al. Severe gastric damage caused by button battery ingestion in a 3-month-old infant. J Pediatr Surg. 2010; 45:e23–e26.
Article9. Kramer RE, Lerner DG, Lin T, Manfredi M, Shah M, Stephen TC, et al. Management of ingested foreign bodies in children: a clinical report of the NASPGHAN Endoscopy Committee. J Pediatr Gastroenterol Nutr. 2015; 60:562–574.10. Litovitz T, Whitaker N, Clark L, White NC, Marsolek M. Emerging battery-ingestion hazard: clinical implications. Pediatrics. 2010; 125:1168–1177.
Article11. Seo JK. Endoscopic management of gastrointestinal foreign bodies in children: a clinical practice guideline. Korean J Pediatr Gastroenterol Nutr. 2007; 10:Suppl 1. 64–69.12. Hamilton JM, Schraff SA, Notrica DM. Severe injuries from coin cell battery ingestions: 2 case reports. J Pediatr Surg. 2009; 44:644–647.
Article13. Mortensen A, Hansen NF, Schiødt OM. Fatal aortoesophageal fistula caused by button battery ingestion in a 1-year-old child. Am J Emerg Med. 2010; 28:984. e5–984. e6..
Article14. Virgilis D, Weinberger JM, Fisher D, Goldberg S, Picard E, Kerem E. Vocal cord paralysis secondary to impacted esophageal foreign bodies in young children. Pediatrics. 2001; 107:E101.
Article15. Soerdjbalie-Maikoe V, van Rijn RR. A case of fatal coin battery ingestion in a 2-year-old child. Forensic Sci Int. 2010; 198:e19–e22.
Article16. Sung SH, Jeon SW, Son HS, Kim SK, Jung MK, Cho CM, et al. Factors predictive of risk for complications in patients with oesophageal foreign bodies. Dig Liver Dis. 2011; 43:632–635.
Article17. Hung CW, Hung SC, Lee CJ, Lee WH, Wu KH. Risk factors for complications after a foreign body is retained in the esophagus. J Emerg Med. 2012; 43:423–427.
Article18. Judith RK, Chris AL. Foreign bodies and bezoars. In : Kliegman R, Stanton B, St Geme J, Schor NF, editors. Nelson textbook of pediatrics. 20th ed. Elsevier Saunder;2015. p. 1814–1816.19. Galligan C, Morose G. An investigation of alternatives to miniature batteries containing mercury [Internet]. Lowell: Maine Department of Environmental Protection;2003. cited 2015 Aug 27. Available from: http://www.sustainableproduction.org/downloads/MaineDEPButtonBatteryReportFinal12-17-04.pdf.20. Gryboski J. Traumatic injury. In : Walker WA, Durie PR, editors. Pediatric gastrointestinal disease. 3rd ed. Hamilton (ON): BC Decker;2000. p. 351–377.21. Mallon PT, White JS, Thompson RL. Systemic absorption of lithium following ingestion of a lithium button battery. Hum Exp Toxicol. 2004; 23:193–195.
Article22. Yardeni D, Yardeni H, Coran AG, Golladay ES. Severe esophageal damage due to button battery ingestion: can it be prevented? Pediatr Surg Int. 2004; 20:496–501.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Colonoscopic Retrieval of a Foreign Body in Children: A Button Battery and an Open Safety Pin
- Foreign Body Ingestion in Children
- Nasal Septal Perforation due to Button Battery
- A case of stacked coin ingestion mistaken for button battery
- A Gastric Magnetic Foreign Body Incidentally Detected Several Years after Ingestion