Pediatr Gastroenterol Hepatol Nutr.
2017 Sep;20(3):204-209. 10.5223/pghn.2017.20.3.204.
Two Cases of Colonoscopic Retrieval of a Foreign Body in Children: A Button Battery and an Open Safety Pin
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea. hryang@snubh.org
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2390553
- DOI: http://doi.org/10.5223/pghn.2017.20.3.204
Abstract
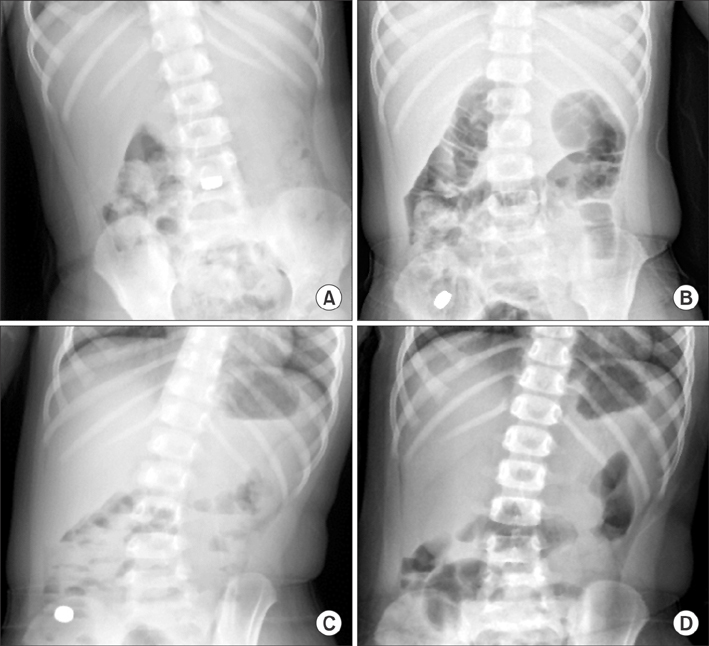
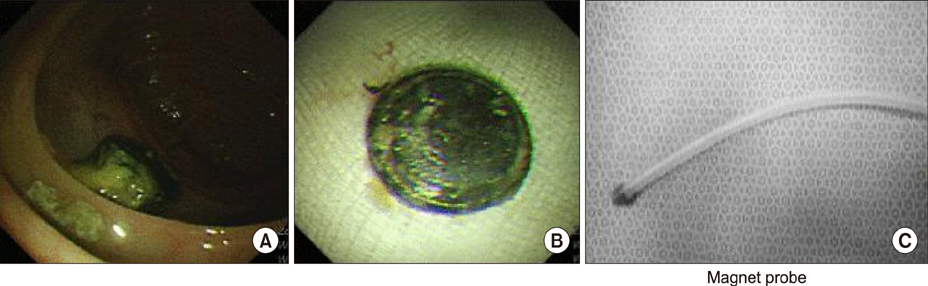
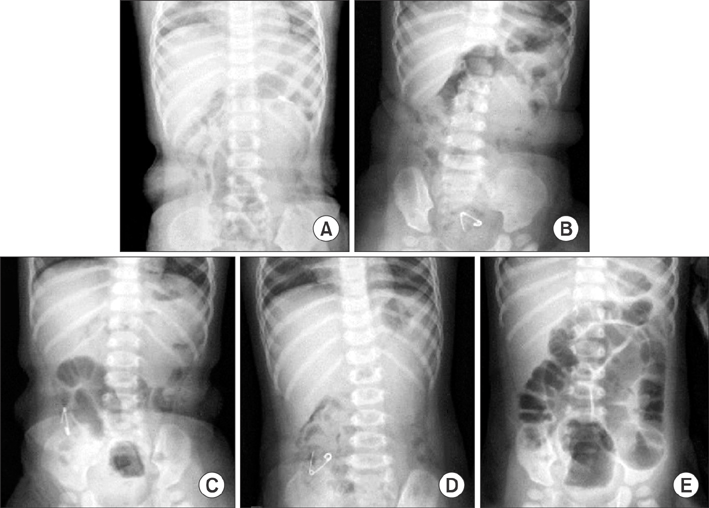
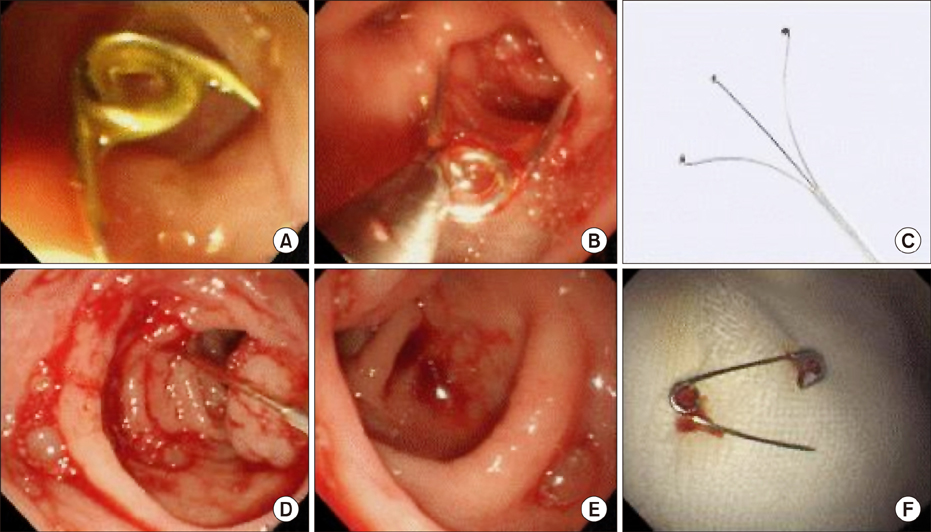
- Ingestion of foreign body in children is a relatively common problem among paediatric population. The foreign bodies mostly pass spontaneously through the gastrointestinal tract. However, complications can occur according to its anatomical location, the characteristics of the foreign body, and delays in management. Although the cases of ingested button batteries or sharp objects impacted at the gastrointestinal tract can be very serious, there have been very only a few cases have reported colonoscopic removal of these dangerous foreign bodies in adults, and there have been no case reports in children. We report one case of a button battery and one case of an open safety pin, both impacted in the terminal ileum that had moved from the stomach within a few hours of ingestion and were eventually managed by colonoscopy without any complications.
Keyword
Figure
Reference
-
1. Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc. 2002; 55:802–806.
Article2. Chang JJ, Yen CL. Endoscopic retrieval of multiple fragmented gastric bamboo chopsticks by using a flexible overtube. World J Gastroenterol. 2004; 10:769–770.
Article3. Tarnasky PR, Newcomer MK, Branch MS. Colonoscopic diagnosis and treatment of chronic chicken bone perforation of the sigmoid colon. Gastrointest Endosc. 1994; 40:373–375.
Article4. Vemula NR, Madariaga J, Brand DL, Hershey H. Colonoscopic removal of a foreign body causing colocutaneous fistulas. Gastrointest Endosc. 1982; 28:195–196.
Article5. Viceconte G, Viceconte GW, Bogliolo G, Pietropaolo V, Dell'Anna A, Montori A. Endoscopic removal of foreign bodies in the large bowel. Endoscopy. 1982; 14:176–177.
Article6. Lyons MF 2nd, Tsuchida AM. Foreign bodies of the gastrointestinal tract. Med Clin North Am. 1993; 77:1101–1114.
Article7. Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc. 1995; 41:39–51.
Article8. Ginsberg GG, Pfau PR. Foreign bodies and bezoars. In : Feldman M, Friedman LS, Sleisenger MH, editors. Sleisenger and fordtran's gastrointestinal and liver disease: pathophysiology/diagnosis/management. London: Saunders;2002. p. 395–397.9. Arana A, Hauser B, Hachimi-Idrissi S, Vandenplas Y. Management of ingested foreign bodies in childhood and review of the literature. Eur J Pediatr. 2001; 160:468–472.
Article10. Hachimi-Idrissi S, Corne L, Vandenplas Y. Management of ingested foreign bodies in childhood: our experience and review of the literature. Eur J Emerg Med. 1998; 5:319–323.11. Chang YJ, Chao HC, Kong MS, Lai MW. Clinical analysis of disc battery ingestion in children. Chang Gung Med J. 2004; 27:673–677.12. Litovitz T, Whitaker N, Clark L, White NC, Marsolek M. Emerging battery-ingestion hazard: clinical implications. Pediatrics. 2010; 125:1168–1177.
Article13. Langkau JF, Noesges RA. Esophageal burns from battery ingestion. Am J Emerg Med. 1985; 3:265.
Article14. Temple DM, McNeese MC. Hazards of battery ingestion. Pediatrics. 1983; 71:100–103.
Article15. Kramer RE, Lerner DG, Lin T, Manfredi M, Shah M, Stephen TC, et al. Management of ingested foreign bodies in children: a clinical report of the NASPGHAN Endoscopy Committee. J Pediatr Gastroenterol Nutr. 2015; 60:562–574.16. Paul RI, Christoffel KK, Binns HJ, Jaffe DM. Foreign body ingestions in children: risk of complication varies with site of initial health care contact. Pediatric Practice Research Group. Pediatrics. 1993; 91:121–127.
Article17. Paul RI, Jaffe DM. Sharp object ingestions in children: illustrative cases and literature review. Pediatr Emerg Care. 1988; 4:245–248.18. Chauvin A, Viala J, Marteau P, Hermann P, Dray X. Management and endoscopic techniques for digestive foreign body and food bolus impaction. Dig Liver Dis. 2013; 45:529–542.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nasal Septal Perforation due to Button Battery
- Two Cases of Button Battery in Nasal Cavity
- A case of stacked coin ingestion mistaken for button battery
- Spondylodiscitis Complicated by the Ingestion of a Button Battery: a Case Report
- A Case Series of Ingested Open Safety Pin Removal Using a Proposed Endoscopic Removal Technique Algorithm