Yonsei Med J.
2007 Aug;48(4):639-644. 10.3349/ymj.2007.48.4.639.
Mid-Term Results of Reconstruction of the Right Ventricular Outflow Tract Using Cryopreserved Homografts
- Affiliations
-
- 1Division of Cardiovascular Surgery, Yonsei Cardiovascular Center, Yonsei University College of Medicine, 250 Seongsanno, Seodaemun-gu, Seoul 120-752, Korea. yhpark@yuhs.ac
- KMID: 2158169
- DOI: http://doi.org/10.3349/ymj.2007.48.4.639
Abstract
- PURPOSE
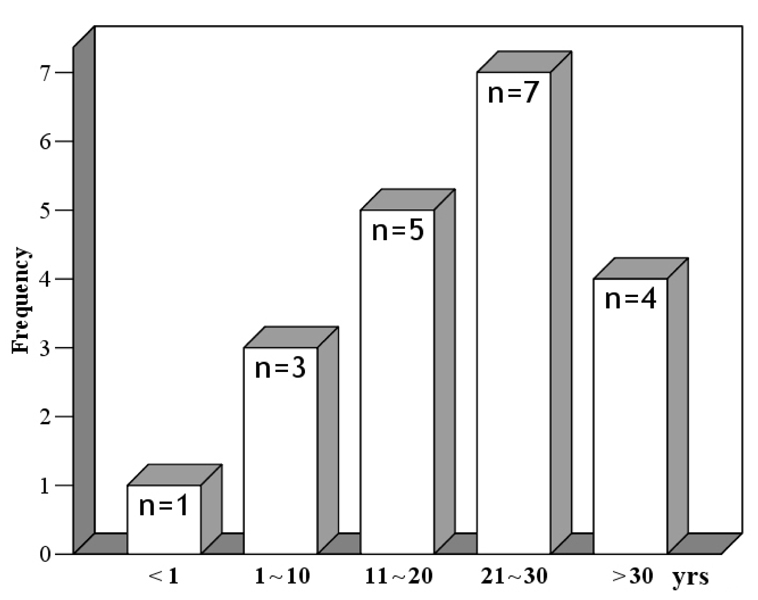
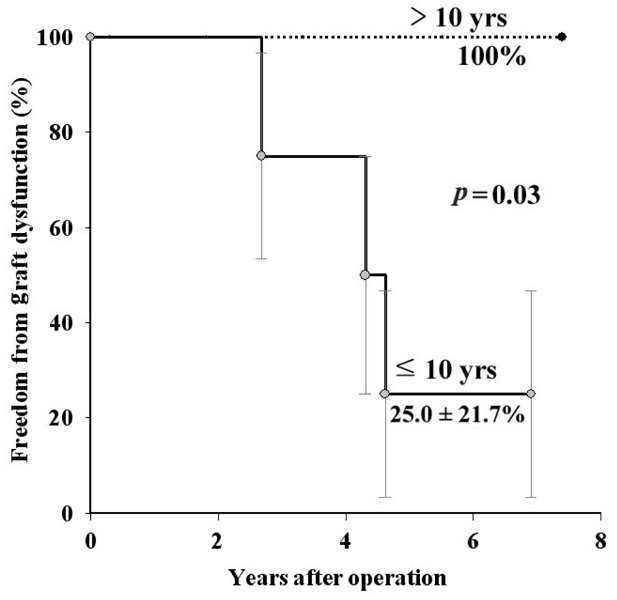
Homograft benefits include excellent hemodynamics, resistance to infection, decreased thromboembolic events, ease of handling, and lack of need for anticoagulation. We examined the short and mid-term results of right ventricular outflow tract (RVOT) reconstruction using cryopreserved homografts. PATIENTS AND METHODS: From May 1998 to May 2005, 20 patients (male:female=10:10) underwent RVOT reconstruction using cryopreserved homografts. The median age was 23.8 years (range, 0.9 to 43.3 years) and the median body weight was 57kg (range, 7.3 to 80kg). Eighteen patients underwent re-operation after shunt or corrective operations. Homograft failure was defined as either re-operation for homograft replacement or patient death. Homograft dysfunction was defined as grade 3 or more than 3 of graft regurgitation and more than 40mmHg of transvalvular pressure gradient under echocardiographic examination. RESULTS: No operative mortality occurred and there were three major complications. Graft failure was observed in one male patient with tetralogy of Fallot. The 8-year freedom from graft failure was 87.5+/-11.7% and the 7-year freedom from graft dysfunction was 62.3+/-17.9%. Multivariable analysis revealed that the independent factor for graft dysfunction was age less than 10 years. In the analysis according to age group, the 7-year freedom from graft dysfunction in the group of patients older than 10 years was 100% and 25.0+/-21.7% in patients age 10 or younger (p= 0.03). CONCLUSION: Right ventricular outflow reconstruction using cryopreserved homografts provided excellent short and mid-term results in most patients in this study. However, in patients younger than 10 years old, homografts for RVOT reconstruction showed a high dysfunction rate at mid-term.
MeSH Terms
Figure
Reference
-
1. Ross DN, Somerville J. Correction of pulmonary atresia with a homograft aortic valve. Lancet. 1966. 2:1446–1447.
Article2. Klinner W, Zenker R. Experience with correction of Fallot's tetralogy in 178 cases. Surgery. 1965. 57:353–357.3. McGoon DC, Rastelli GC, Ongley PA. An operation for the correction of truncus arteriosus. JAMA. 1968. 205:69–73.
Article4. Albert JD, Bishop DA, Fullerton DA, Campbell DN, Clarke DR. Conduit reconstruction of the right ventricular outflow tract. Lessons learned in a twelve-year experience. J Thorac Cardiovasc Surg. 1993. 106:228–236.5. Jonas RA, Freed MD, Mayer JE, Castaneda AR. Long-term follow-up of patients with synthetic right heart conduits. Circulation. 1985. 72:II77–II83.6. Santini F, Mazzucco A. Bicuspid homograft reconstruction of the right ventricular outflow tract in infants. Ann Thorac Surg. 1995. 60:S624–S625.
Article7. Bando K, Danielson GK, Schaff HV, Mair DD, Julsrud PR, Puga FJ. Outcome of pulmonary and aortic homografts for right ventricular outflow tract reconstruction. J Thorac Cardiovasc Surg. 1995. 109:509–518.
Article8. Daenen W, Gewillig M. Factors influencing medium-term performance of right-sided cryopreserved homografts. J Heart Valve Dis. 1997. 6:347–353.9. Edmunds LH, Clark RE, Cohn LH, Grunkemeier GL, Miller DC, Weisel RD. Guidelines for reporting morbidity and mortality after cardiac valvular operations. The American Association for Thoracic Surgery, Ad Hoc Liasion Committee for Standardizing, Definitions of Prosthetic Heart Valve Morbidity. Ann Thorac Surg. 1996. 62:932–935.
Article10. Gatzoulis MA, Clark AL, Cullen S, Newman CG, Redington AN. Right ventricular diastolic function 15 to 35 years after repair of tetralogy of Fallot. Restrictive physiology predicts superior exercise performance. Circulation. 1995. 91:1775–1781.
Article11. Jonsson H, Ivert T, Jonasson R, Holmgren A, Björk VO. Work capacity and central hemodynamics thirteen to twenty-six years after repair of tetralogy of Fallot. J Thorac Cardiovasc Surg. 1995. 110:416–426.
Article12. Bove EL, Kavey RE, Byrum CJ, Sondheimer HM, Blackman MS, Thomas FD. Improved right ventricular function following late pulmonary valve replacement for residual pulmonary insufficiency or stenosis. J Thorac Cardiovasc Surg. 1985. 90:50–55.
Article13. Yemets IM, Williams WG, Webb GD, Harrison DA, McLaughlin PR, Trusler GA, et al. Pulmonary valve replacement late after repair of tetralogy of Fallot. Ann Thorac Surg. 1997. 64:526–530.
Article14. Joung B, Xu Z, Kim I, Lee MH, Kim S. The effect of cryoinjury on ventricular tachycardia in the swine right ventricle. Yonsei Med J. 2006. 47:672–679.
Article15. Bielefeld MR, Bishop DA, Campbell DN, Mitchell MB, Grover FL, Clarke DR. Reoperative homograft right ventricular outflow tract reconstruction. Ann Thorac Surg. 2001. 71:482–488.
Article16. Baskett RJ, Ross DB, Nanton MA, Murphy DA. Factors in the early failure of cryopreserved homograft pulmonary valves in children: preserved immunogenicity? J Thorac Cardiovasc Surg. 1996. 112:1170–1179.
Article17. Khambadkone S, Coats L, Taylor A, Boudjemline Y, Derrick G, Tsang V, et al. Percutaneous pulmonary valve implantation in humans: results in 59 consecutive patients. Circulation. 2005. 112:1189–1197.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of Bicuspidalized Cryopreserved Allograft Valves for the RVOT Reconstruction in Complex Cardiac Anomalies
- Long Term Results of Right Ventricular Outflow Tract Reconstruction with Homografts
- Right Ventricular Outflow Tract Reconstruction with Bicuspid
- Aortic Valve Replacement with Pulmonary Autograft in Patient with Congenital Aortic Stenosis : Ross Procedure without Homograft: one case report
- A Rare Case of Unruptured Sinus of Valsalva Aneurysm Obstructing the Right Ventricular Outflow Tract