J Korean Med Sci.
2012 Dec;27(12):1499-1506. 10.3346/jkms.2012.27.12.1499.
Acute and Long-Term Angiographic Outcomes of Side Branch Stenosis after Randomized Treatment of Zotarolimus-, Sirolimus-, and Paclitaxel-Eluting Stent for Coronary Artery Stenosis
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Kangwon National University School of Medicine, Kangwon National University Hospital, Chuncheon, Korea.
- 2Department of Cardiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. sjpark@amc.seoul.kr
- 3Division of Biostatistics, Center for Medical Research and Information, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 4Department of Cardiology, Chungnam National University Hospital, Daejeon, Korea.
- KMID: 2157973
- DOI: http://doi.org/10.3346/jkms.2012.27.12.1499
Abstract
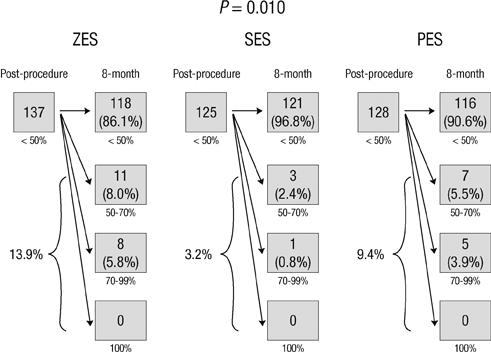
- This was designed to assess the outcomes of side branch (SB) stenosis after implantation of three drug-eluting stents (DES). From 2,645 patients in the ZEST (Comparison of the Efficacy and Safety of Zotarolimus-Eluting Stent with Sirolimus-Eluting and PacliTaxel-Eluting Stent for Coronary Lesions) Trial, 788 patients had 923 bifurcation lesions with SB > or = 1.5 mm were included. SB was treated in 150 lesions, including 35 (3.8%) receiving SB stenting. Of untreated SB with baseline stenosis < 50%, the incidences of periprocedural SB compromise was similar in the zotarolimus (15.8%), sirolimus (17.2%), and paclitaxel (16.6%) stent groups (P = 0.92). At follow-up angiography, delayed SB compromise occurred in 13.9%, 3.2%, and 9.4% (P = 0.010) of these groups. When classified into four groups (< 50%, 50%-70%, 70%-99%, and 100%), 9.0% of untreated SB were worsened, whereas improvement and stationary were observed in 9.6% and 81.4%. In a multivariable logistic regression model, main branch (MB) stenosis at follow-up (%) was the only independent predictor of SB stenosis worsening (odds ratio, 1.03; 95% confidence interval, 1.01-1.04; P < 0.001). After MB stenting in bifurcation lesions, a minority of SB appears to worsen. DES with strong anti-restenotic efficacy may help maintain SB patency.
Keyword
MeSH Terms
-
Acute Disease
Aged
Blood Vessels/physiopathology
Cardiovascular Agents/*therapeutic use
Coronary Angiography
Coronary Stenosis/*drug therapy/physiopathology/radiography
Drug-Eluting Stents/*adverse effects
Female
Follow-Up Studies
Humans
Logistic Models
Male
Middle Aged
Myocardial Infarction/etiology/radiography
Myocardial Revascularization
Odds Ratio
Paclitaxel/*therapeutic use
Predictive Value of Tests
Sirolimus/*analogs & derivatives/*therapeutic use
Thrombosis/etiology
Treatment Outcome
Cardiovascular Agents
Paclitaxel
Sirolimus
Figure
Reference
-
1. Kim YH, Park DW, Suh IW, Jang JS, Hwang ES, Jeong YH, Lee SW, Lee SW, Lee CW, Hong MK, et al. Long-term outcome of simultaneous kissing stenting technique with sirolimus-eluting stent for large bifurcation coronary lesions. Catheter Cardiovasc Interv. 2007. 70:840–846.2. Kim YH, Park SW, Hong MK, Park DW, Park KM, Lee BK, Song JM, Han KH, Lee CW, Kang DH, et al. Comparison of simple and complex stenting techniques in the treatment of unprotected left main coronary artery bifurcation stenosis. Am J Cardiol. 2006. 97:1597–1601.3. Pan M, de Lezo JS, Medina A, Romero M, Segura J, Pavlovic D, Delgado A, Ojeda S, Melián F, Herrador J, et al. Rapamycin-eluting stents for the treatment of bifurcated coronary lesions: a randomized comparison of a simple versus complex strategy. Am Heart J. 2004. 148:857–864.4. Colombo A, Moses JW, Morice MC, Ludwig J, Holmes DR Jr, Spanos V, Louvard Y, Desmedt B, Di Mario C, Leon MB. Randomized study to evaluate sirolimus-eluting stents implanted at coronary bifurcation lesions. Circulation. 2004. 109:1244–1249.5. Steigen TK, Maeng M, Wiseth R, Erglis A, Kumsars I, Narbute I, Gunnes P, Mannsverk J, Meyerdierks O, Rotevatn S, et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. 2006. 114:1955–1961.6. Ferenc M, Gick M, Kienzle RP, Bestehorn HP, Werner KD, Comberg T, Kuebler P, Büttner HJ, Neumann FJ. Randomized trial on routine vs. provisional T-stenting in the treatment of de novo coronary bifurcation lesions. Eur Heart J. 2008. 29:2859–2867.7. Koo BK, Kang HJ, Youn TJ, Chae IH, Choi DJ, Kim HS, Sohn DW, Oh BH, Lee MM, Park YB, et al. Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. 2005. 46:633–637.8. Louvard Y, Thomas M, Dzavik V, Hildick-Smith D, Galassi AR, Pan M, Burzotta F, Zelizko M, Dudek D, Ludman P, et al. Classification of coronary artery bifurcation lesions and treatments: time for a consensus! Catheter Cardiovasc Interv. 2008. 71:175–183.9. Colombo A, Bramucci E, Saccà S, Violini R, Lettieri C, Zanini R, Sheiban I, Paloscia L, Grube E, Schofer J, et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) Study. Circulation. 2009. 119:71–78.10. Lefèvre T, Louvard Y, Morice MC, Dumas P, Loubeyre C, Benslimane A, Premchand RK, Guillard N, Piéchaud JF. Stenting of bifurcation lesions: classification, treatments, and results. Catheter Cardiovasc Interv. 2000. 49:274–283.11. Niemelä M, Kervinen K, Erglis A, Holm NR, Maeng M, Christiansen EH, Kumsars I, Jegere S, Dombrovskis A, Gunnes P, et al. Randomized comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: the Nordic-Baltic Bifurcation Study III. Circulation. 2011. 123:79–86.12. Poerner TC, Kralev S, Voelker W, Sueselbeck T, Latsch A, Pfleger S, Schumacher B, Borggrefe M, Haase KK. Natural history of small and medium-sized side branches after coronary stent implantation. Am Heart J. 2002. 143:627–635.13. Tanabe K, Serruys PW, Degertekin M, Regar E, van Domburg RT, Sousa JE, Wülfert E, Morice MC. Fate of side branches after coronary arterial sirolimus-eluting stent implantation. Am J Cardiol. 2002. 90:937–941.14. Arora RR, Raymond RE, Dimas AP, Bhadwar K, Simpfendorfer C. Side branch occlusion during coronary angioplasty: incidence, angiographic characteristics, and outcome. Cathet Cardiovasc Diagn. 1989. 18:210–212.15. Park DW, Kim YH, Yun SC, Kang SJ, Lee SW, Lee CW, Park SW, Seong IW, Lee JH, Tahk SJ, et al. Comparison of zotarolimus-eluting stents with sirolimus- and paclitaxel-eluting stents for coronary revascularization: the ZEST (Comparison of the Efficacy and Safety of Zotarolimus-Eluting Stent with Sirolimus-Eluting and PacliTaxel-Eluting Stent for Coronary Lesions) randomized trial. J Am Coll Cardiol. 2010. 56:1187–1195.16. Popma JJ, Leon MB, Moses JW, Holmes DR Jr, Cox N, Fitzpatrick M, Douglas J, Lambert C, Mooney M, Yakubov S, et al. Quantitative assessment of angiographic restenosis after sirolimus-eluting stent implantation in native coronary arteries. Circulation. 2004. 110:3773–3780.17. Mehran R, Dangas G, Abizaid AS, Mintz GS, Lansky AJ, Satler LF, Pichard AD, Kent KM, Stone GW, Leon MB. Angiographic patterns of in-stent restenosis: classification and implications for long-term outcome. Circulation. 1999. 100:1872–1878.18. Medina A, Suárez de Lezo J, Pan M. A new classification of coronary bifurcation lesions. Rev Esp Cardiol. 2006. 59:183.19. Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, Steg PG, Morel MA, Mauri L, Vranckx P, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007. 115:2344–2351.20. Mazur W, Grinstead WC, Hakim AH, Dabaghi SF, Abukhalil JM, Ali NM, Joseph J, French BA, Raizner AE. Fate of side branches after intracoronary implantation of the Gianturco-Roubin flex-stent for acute or threatened closure after percutaneous transluminal coronary angioplasty. Am J Cardiol. 1994. 74:1207–1210.21. Goktekin O, Kaplan S, Dimopoulos K, Barlis P, Tanigawa J, Vatankulu MA, Koning G, Tuinenburg JC, Mario CD. A new quantitative analysis system for the evaluation of coronary bifurcation lesions: comparison with current conventional methods. Catheter Cardiovasc Interv. 2007. 69:172–180.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Simultaneous Multi-Vessel Subacute Stent Thromboses in Zotarolimus-Eluting Stents
- Comparisons of the Short-Term Angiographic Outcomes of Cypher and Taxus Stents Implanted in the Same Patient
- A Case of Late Recurrent Vasospasm After Sirolimus-Eluting Stent Implantation
- Right Coronary Artery Ostial Stenosis after Re-do Aortic Valve Replacement
- A Case of Huge Coronary Aneurysm After Implantation of a Sirolimus-Eluting Stent