J Korean Med Sci.
2011 Mar;26(3):425-430. 10.3346/jkms.2011.26.3.425.
Usefulness of Videofluoroscopic Swallow Study with Mixed Consistency Food for Patients with Stroke or Other Brain Injuries
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Chung-Ang University College of Medicine, Seoul, Korea. donkim21@gmail.com
- KMID: 2157882
- DOI: http://doi.org/10.3346/jkms.2011.26.3.425
Abstract
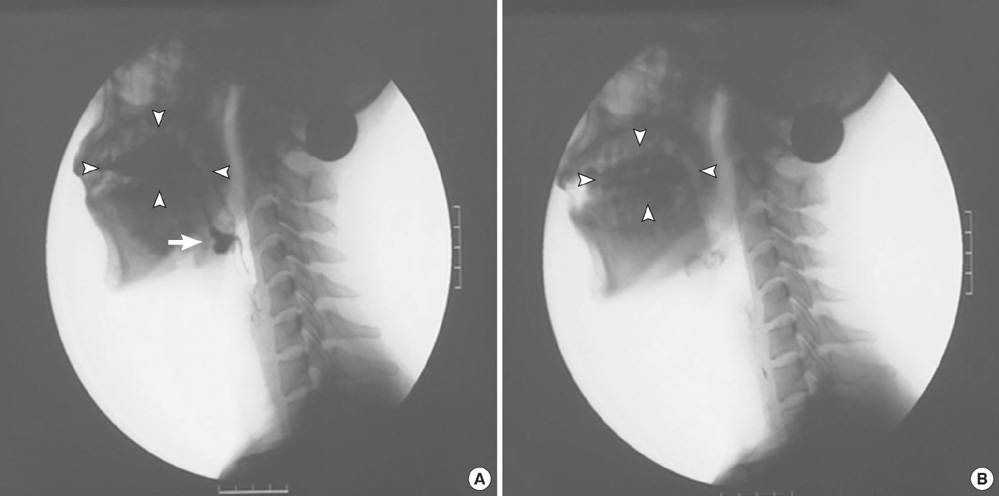
- This study evaluated the feasibility of mixed consistency foods test in patients with dysphagia which developed after stroke or other brain injuries. The findings of a videofluoroscopic swallow study (VFSS) were compared using single versus mixed consistency foods. Forty-nine patients with stroke or other brain injuries who had no significant abnormal findings in the single consistency food VFSS and started regular hospital diet were recruited for this study. Twenty-five (51%) of the 49 patients showed normal findings whereas 24 (49%) patients showed abnormal findings in the mixed consistency food VFSS. Abnormal findings included posterior spillage of liquid prematurely to pyriform sinus (n = 23), laryngeal penetration (n = 6), subglottic aspiration in the oral preparatory phase of swallowing (chewing), solid components (n = 2), and significant (more than 10%) residue in valleculae or pyriform sinus (n = 2). There was an increased risk of abnormal findings in mixed consistency food VFSS such as aspiration and penetration when a patient showed delayed pharyngeal delay time in single consistency food using liquids. In conclusion, VFSS protocols using mixed consistency foods would be useful before starting regular diet for patients after stroke or other brain injuries.
Keyword
MeSH Terms
Figure
Reference
-
1. Barer DH. The natural history and functional consequences of dysphagia after hemispheric stroke. J Neurol Neurosurg Psychiatry. 1989. 52:236–241.2. Meng NH, Wang TG, Lien IN. Dysphagia in patients with brainstem stroke: incidence and outcome. Am J Phys Med Rehabil. 2000. 79:170–175.3. Safaz I, Alaca R, Yasar E, Tok F, Yilmaz B. Medical complications, physical function and communication skills in patients with traumatic brain injury: a single centre 5-year experience. Brain Inj. 2008. 22:733–739.4. Perlman AL. Dysphagia in stroke patients. Semin Neurol. 1996. 16:341–348.5. Saitoh E, Shibata S, Matsuo K, Baba M, Fujii W, Palmer JB. Chewing and food consistency: effects on bolus transport and swallow initiation. Dysphagia. 2007. 22:100–107.6. Hiiemae KM, Palmer JB. Food transport and bolus formation during complete feeding sequences on foods of different initial consistency. Dysphagia. 1999. 14:31–42.7. Logemann JA. Manual for the videofluorographic study of swallowing. 1993. 2nd ed. Austin: Pro-Ed;157–162.8. Han TR, Paik NJ, Park JW, Kwon BS. The prediction of persistent dysphagia beyond six months after stroke. Dysphagia. 2008. 23:59–64.9. Han TR, Paik NJ, Park JW. The functional dysphagia scale using videofluoroscopic swallowing study in stroke patients. J Korean Acad Rehabil Med. 1999. 23:1118–1126.10. Logemann JA. Evaluation and treatment of swallowing disorders. 1998. 2nd ed. Austin: Pro-Ed;89–96.11. Johnson ER, McKenzie SW, Rosenquist CJ, Liberman JS, Sievers AE. Dysphagia following stroke: quantitative evaluation of pharyngeal transit times. Arch Phys Med Rehabil. 1992. 73:419–423.12. Han TR, Kim JH, Paik NJ, Lim JH, Jeong JK, Han JK. Quantitative evaluation of dysphagia in hemiplegic patients. J Korean Acad Rehabil Med. 1996. 20:45–52.13. Tracy JF, Logemann JA, Kahrilas PJ, Jacob P, Kobara M, Krugler C. Preliminary observations on the effects of age on oropharyngeal deglutition. Dysphagia. 1989. 4:90–94.14. Ozaki K, Kagaya H, Yokoyama M, Saitoh E, Okada S, González-Fernández M, Palmer JB, Uematsu AH. The risk of penetration or aspiration during videofluoroscopic examination of swallowing varies depending on food types. Tohoku J Exp Med. 2010. 220:41–46.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Functional Dysphagia Scale Using Videofluoroscopic Swallowing Study in Stroke Patients
- Recommendation of Nasogastric Tube Removal in Acute Stroke Patients Based on Videofluoroscopic Swallow Study
- The Comparison of Videofluoroscopic Findings between the Patients with Lateral Medullary Infarct and Middle Cerebral Artery Territorial Infarct
- Prognostic Indicators in Dysphagia Recovery
- The Effect of Balloon Dilatation through Video-Fluoroscopic Swallowing Study (VFSS) in Stroke Patients with Cricopharyngeal Dysfunction