Ann Rehabil Med.
2016 Feb;40(1):142-151. 10.5535/arm.2016.40.1.142.
The Additive Effects of Core Muscle Strengthening and Trunk NMES on Trunk Balance in Stroke Patients
- Affiliations
-
- 1Department of Rehabilitation Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. mhchun@amc.seoul.kr
- 2Department of Physical Medicine and Rehabilitation Medicine, Dream Hospital, Seoul, Korea.
- 3Department of Rehabilitation Medicine, Raphael Geriatric Hospital, Suwon, Korea.
- KMID: 2155177
- DOI: http://doi.org/10.5535/arm.2016.40.1.142
Abstract
OBJECTIVE
To investigate an additive effect of core muscle strengthening (CMS) and trunk neuromuscular electrical stimulation (tNEMS) on trunk balance in stroke patients.
METHODS
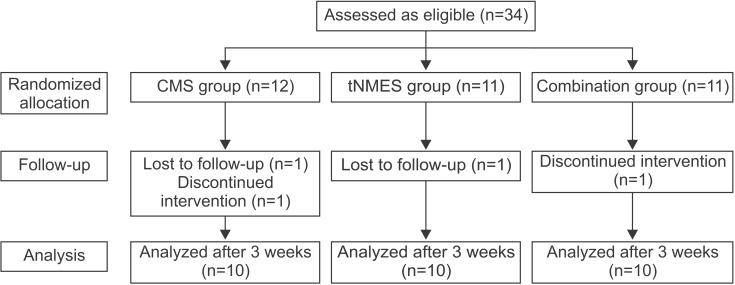
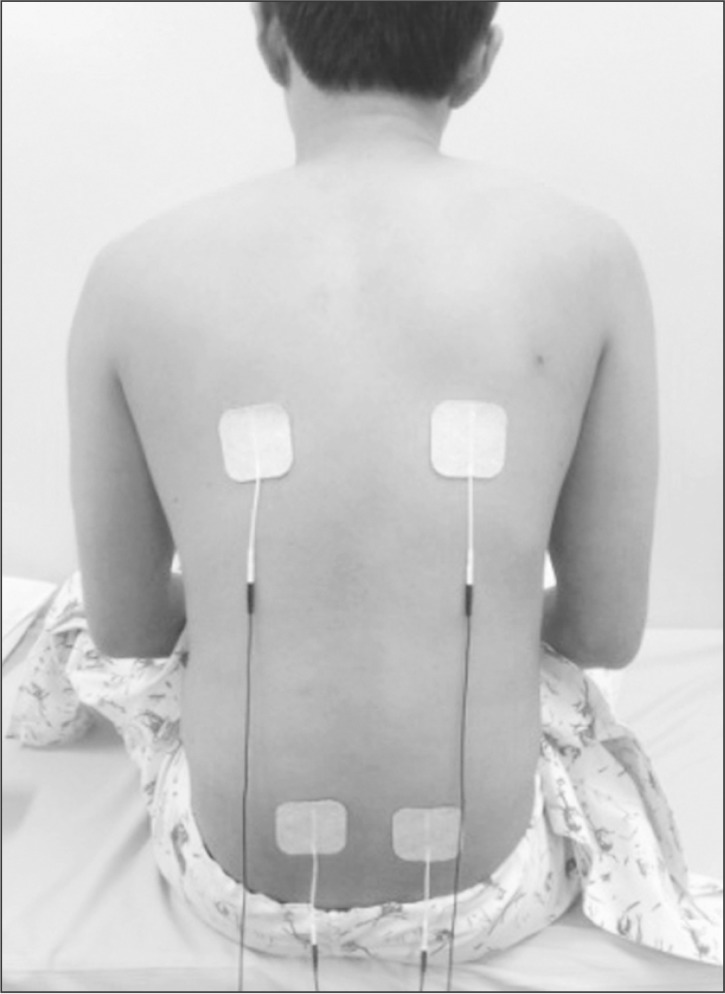
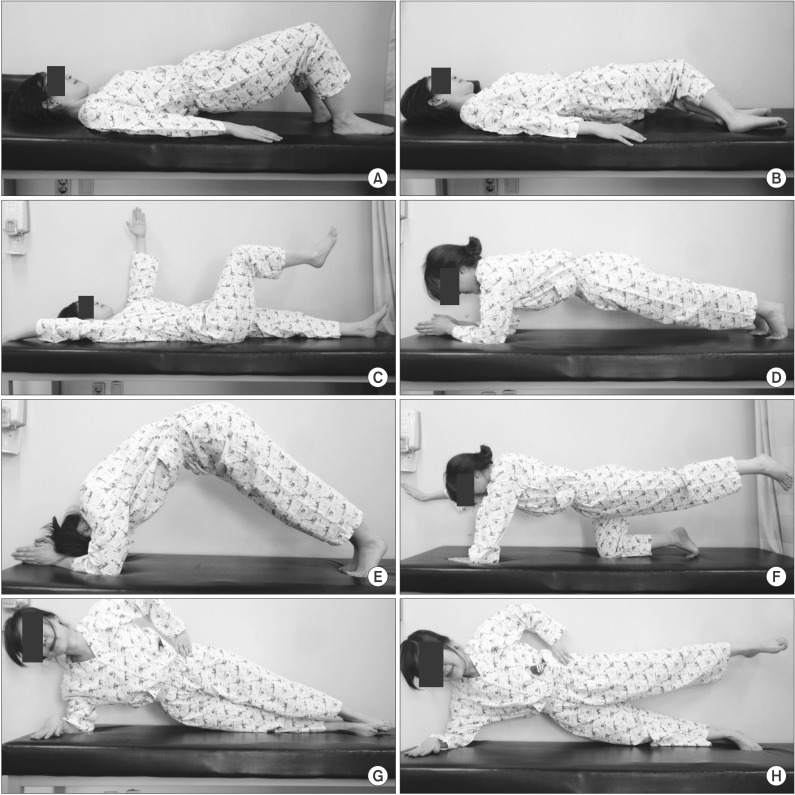
Thirty patients with acute or subacute stroke who were unable to maintain static sitting balance for >5 minutes were enrolled and randomly assigned to 3 groups, i.e., patients in the CMS (n=10) group received additional CMS program; the tNMES group (n=10) received additional tNMES over the posterior back muscles; and the combination (CMS and tNMES) group (n=10) received both treatments. Each additional treatment was performed 3 times per week for 20 minutes per day over 3 weeks. Korean version of Berg Balance Scale (K-BBS), total score of postural assessment scale for stroke patients (PASS), Trunk Impairment Scale (TIS), and Korean version of Modified Barthel Index (K-MBI) were evaluated before and after 3 weeks of therapeutic intervention.
RESULTS
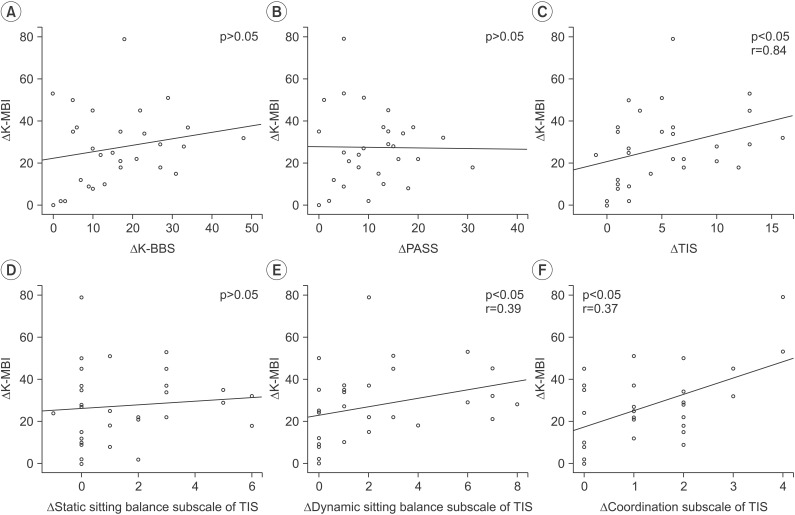
All 3 groups showed improvements in K-BBS, PASS, TIS, and K-MBI after therapeutic interventions, with some differences. The combination group showed more improvements in K-BBS and the dynamic sitting balance of TIS, as compared to the CMS group; and more improvement in K-BBS, as compared to the tNMES group.
CONCLUSION
The results indicated an additive effect of CMS and tNMES on the recovery of trunk balance in patients with acute or subacute stroke who have poor sitting balance. Simultaneous application of CMS and tNMES should be considered when designing a rehabilitation program to improve trunk balance in stroke patients.
Keyword
Figure
Cited by 1 articles
-
Comparison Between Neuromuscular Electrical Stimulation to Abdominal and Back Muscles on Postural Balance in Post-stroke Hemiplegic Patients
Mingeun Park, Hyun Seok, Sang-Hyun Kim, Kyudong Noh, Seung Yeol Lee
Ann Rehabil Med. 2018;42(5):652-659. doi: 10.5535/arm.2018.42.5.652.
Reference
-
1. Warlow CP, van Gijn J, Dennis MS, Wardlaw JM, Bamford JM, Hankey GJ, et al. Stroke: practical management. 3rd ed. Malden: Blackwell Publishing;2008.2. Merkert J, Butz S, Nieczaj R, Steinhagen-Thiessen E, Eckardt R. Combined whole body vibration and balance training using Vibrosphere: improvement of trunk stability, muscle tone, and postural control in stroke patients during early geriatric rehabilitation. Z Gerontol Geriatr. 2011; 44:256–261. PMID: 21505939.3. Perlmutter S, Lin F, Makhsous M. Quantitative analysis of static sitting posture in chronic stroke. Gait Posture. 2010; 32:53–56. PMID: 20399661.
Article4. Carr LJ, Harrison LM, Stephens JA. Evidence for bilateral innervation of certain homologous motoneurone pools in man. J Physiol. 1994; 475:217–227. PMID: 8021829.
Article5. Yoo SD, Jeong YS, Kim DH, Lee MA, Noh SG, Shin YW, et al. The efficacy of core strengthening on the trunk balance in patients with subacute stroke. J Korean Acad Rehabil Med. 2010; 34:677–682.6. Karatas M, Cetin N, Bayramoglu M, Dilek A. Trunk muscle strength in relation to balance and functional disability in unihemispheric stroke patients. Am J Phys Med Rehabil. 2004; 83:81–87. PMID: 14758293.
Article7. Slijper H, Latash ML, Rao N, Aruin AS. Task-specific modulation of anticipatory postural adjustments in individuals with hemiparesis. Clin Neurophysiol. 2002; 113:642–655. PMID: 11976044.
Article8. Dickstein R, Shefi S, Marcovitz E, Villa Y. Anticipatory postural adjustment in selected trunk muscles in post stroke hemiparetic patients. Arch Phys Med Rehabil. 2004; 85:261–267. PMID: 14966711.9. Hsieh CL, Sheu CF, Hsueh IP, Wang CH. Trunk control as an early predictor of comprehensive activities of daily living function in stroke patients. Stroke. 2002; 33:2626–2630. PMID: 12411652.
Article10. Moreland J, Thomson MA. Efficacy of electromyo-graphic biofeedback compared with conventional physical therapy for upper-extremity function in patients following stroke: a research overview and meta-analysis. Phys Ther. 1994; 74:534–547. PMID: 8197240.
Article11. van der Lee JH, Snels IA, Beckerman H, Lankhorst GJ, Wagenaar RC, Bouter LM. Exercise therapy for arm function in stroke patients: a systematic review of randomized controlled trials. Clin Rehabil. 2001; 15:20–31. PMID: 11237158.
Article12. Yu SH, Park SD. The effects of core stability strength exercise on muscle activity and trunk impairment scale in stroke patients. J Exerc Rehabil. 2013; 9:362–367. PMID: 24278885.
Article13. Kim YM, Chun MH, Kang SH, Ahn WH. The effect of neuromuscular electrical stimulation on trunk control in hemiparetic stroke patients. J Korean Acad Rehabil Med. 2009; 33:265–270.14. Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther. 2008; 88:559–566. PMID: 18292215.
Article15. Benaim C, Perennou DA, Villy J, Rousseaux M, Pelissier JY. Validation of a standardized assessment of postural control in stroke patients: the Postural Assessment Scale for Stroke Patients (PASS). Stroke. 1999; 30:1862–1868. PMID: 10471437.16. Verheyden G, Nieuwboer A, Mertin J, Preger R, Kiekens C, De Weerdt W. The Trunk Impairment Scale: a new tool to measure motor impairment of the trunk after stroke. Clin Rehabil. 2004; 18:326–334. PMID: 15137564.
Article17. Jung HY, Park JH, Shim JJ, Kim MJ, Hwang MR, Kim SH. Reliability test of Korean version of Berg Balance Scale. J Korean Acad Rehabil Med. 2006; 30:611–618.18. Verheyden G, Nieuwboer A, Feys H, Thijs V, Vaes K, De Weerdt W. Discriminant ability of the Trunk Impairment Scale: a comparison between stroke patients and healthy individuals. Disabil Rehabil. 2005; 27:1023–1028. PMID: 16096256.
Article19. Verheyden G, Vereeck L, Truijen S, Troch M, Lafosse C, Saeys W, et al. Additional exercises improve trunk performance after stroke: a pilot randomized controlled trial. Neurorehabil Neural Repair. 2009; 23:281–286. PMID: 18955513.
Article20. Van Nes IJ, Nienhuis B, Latour H, Geurts AC. Posturographic assessment of sitting balance recovery in the subacute phase of stroke. Gait Posture. 2008; 28:507–512. PMID: 18424149.21. Verheyden G, Vereeck L, Truijen S, Troch M, Herregodts I, Lafosse C, et al. Trunk performance after stroke and the relationship with balance, gait and functional ability. Clin Rehabil. 2006; 20:451–458. PMID: 16774097.
Article22. Hodges PW. Core stability exercise in chronic low back pain. Orthop Clin North Am. 2003; 34:245–254. PMID: 12914264.
Article23. Richardson CA, Jull GA, Hodges PW, Hides JA. Therapeutic exercise for spinal segmental stabilization in low back pain: scientific basis and clinical approach. Edinburgh: Churchill Livingstone;1999.24. Porterfield JA, DeRosa C. Mechanical low back pain: perspectives in functional anatomy. 2nd ed. Philadelphia: W. B. Saunders;1998.25. Tanaka S, Hachisuka K, Ogata H. Muscle strength of trunk flexion-extension in post-stroke hemiplegic patients. Am J Phys Med Rehabil. 1998; 77:288–290. PMID: 9715916.26. Kimberley TJ, Lewis SM, Auerbach EJ, Dorsey LL, Lojovich JM, Carey JR. Electrical stimulation driving functional improvements and cortical changes in subjects with stroke. Exp Brain Res. 2004; 154:450–460. PMID: 14618287.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Clam Exercise on the Trunk Control and Balance of Stroke Patients
- The Efficacy of Core Strengthening on the Trunk Balance in Patients with Subacute Stroke
- Comparison Between Neuromuscular Electrical Stimulation to Abdominal and Back Muscles on Postural Balance in Post-stroke Hemiplegic Patients
- The Effects of Isokinetic Strengthening of Trunk Muscles on Balance in Hemiplegic Patients
- The Effect of an Abdominal Drawing-In Maneuver Combined with Low·High Frequency Neuromuscular Electrical Stimulation on Trunk Muscle Activity, Muscle Fatigue, and Balance in Stroke Patients