Endovascular Treatment of Dural Arteriovenous Fistulas: Single Center Experience
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea. smyoon@sch.ac.kr
- KMID: 2152914
- DOI: http://doi.org/10.3340/jkns.2016.59.1.17
Abstract
OBJECTIVE
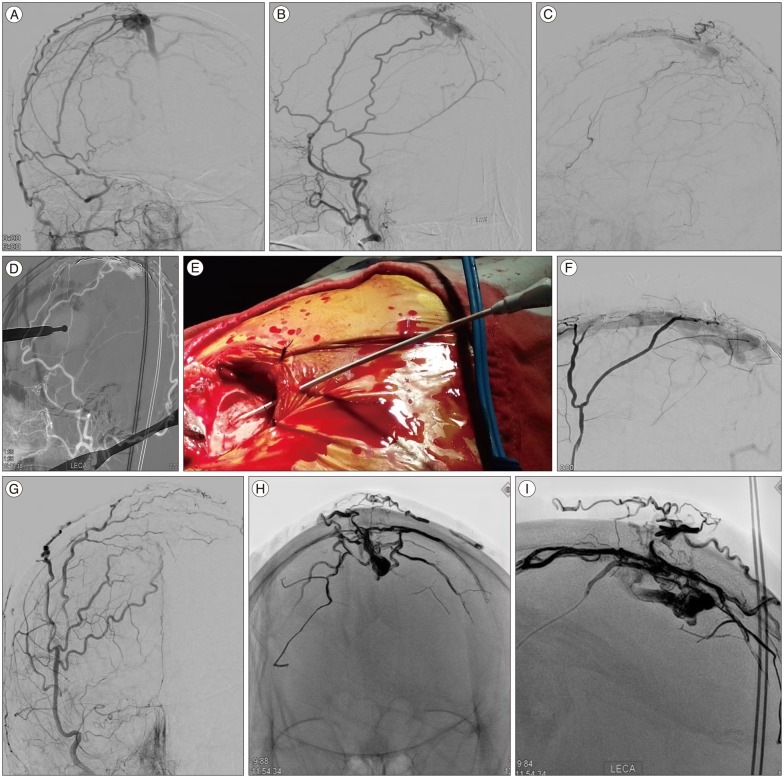
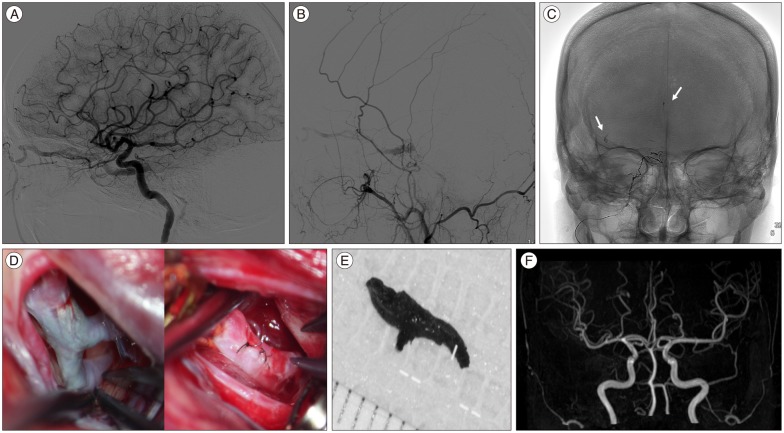
Treatment of intracranial dural arteriovenous fistulas (dAVFs) remains a challenge. However, after introduction of Onyx, transarterial approach is the preferred treatment option in many centers. We report our experience of dAVFs embolization with special emphasis on transarterial approach.
METHODS
Seventeen embolization procedures were performed in 13 patients with dAVFs between Jan 2009 and Oct 2014. Clinical symptoms, location and type of fistulas, embolization methods, complications, radiological and clinical outcomes were evaluated using charts and PACS images.
RESULTS
All 13 patients had symptomatic lesions. The locations of fistulas were transverse-sigmoid sinus in 6, middle fossa dura in 4, cavernous sinus in 2, and superior sagittal sinus in 1 patient. Cognard types were as follows : I in 4, IIa in 2, IIa+IIb in 5, and IV in 2. Embolization procedures were performed > or =2 times in 3 patients. Nine patients were treated with transarterial Onyx embolization alone. One of these required direct surgical puncture of middle meningeal artery. Complete obliteration of fistulas was achieved in 11/13 (85%) patients. There were no complications except for 1 case of Onyx migration in cavernous dAVF. Modified Rankin scale score at post-operative 3 months were 0 in 11, and 3 in 2 patients.
CONCLUSION
Transarterial Onyx embolization can be a first line therapeutic option in patients with dAVFs. However, transvenous approach should be tried first in cavernous sinus dAVF because of the risk of intracranial migration of liquid embolic materials. Furthermore, combined surgical endovascular approach can be considered as a useful option in inaccessible route.
MeSH Terms
Figure
Cited by 3 articles
-
Refractory Spontaneous Chronic Subdural Hematoma: A Rare Presentation of an Intracranial Arteriovenous Fistula
El Kim
J Cerebrovasc Endovasc Neurosurg. 2016;18(4):373-378. doi: 10.7461/jcen.2016.18.4.373.Dural Arteriovenous Fistula Manifested as Rapid Progressive Dementia Successfully Treated by Endovascular Embolization Only
Heewon Hwang, Yun Kyung La, Min Seok Baek, Kyoungwon Baik, Sang Hyun Suh, Won-Joo Kim
Neurointervention. 2017;12(1):50-53. doi: 10.5469/neuroint.2017.12.1.50.Occurrence of
De Novo Dural Arteriovenous Fistula after Transvenous Embolization of Dural Arteriovenous Fistula : Case Reports of Two Patients
Ippei Makita, Yoshinobu Kamio, Hisaya Hiramatsu, Kazuhiko Kurozumi
J Korean Neurosurg Soc. 2022;65(4):598-602. doi: 10.3340/jkns.2021.0144.
Reference
-
1. Awad IA, Little JR, Akarawi WP, Ahl J. Intracranial dural arteriovenous malformations : factors predisposing to an aggressive neurological course. J Neurosurg. 1990; 72:839–850. PMID: 2140125.
Article2. Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995; 82:166–179. PMID: 7815143.
Article3. Chung SJ, Kim JS, Kim JC, Lee SK, Kwon SU, Lee MC, et al. Intracranial dural arteriovenous fistulas : analysis of 60 patients. Cerebrovasc Dis. 2002; 13:79–88. PMID: 11867880.
Article4. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas : clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995; 194:671–680. PMID: 7862961.
Article5. Fujita A, Kuwamura K, Saitoh M, Sakagami Y, Takaishi Y, Suzuki S, et al. [Cerebral sinus thrombosis in a patient with protein S deficiency : a case report]. No Shinkei Geka. 1997; 25:467–472. PMID: 9145407.6. Gerlach R, Yahya H, Rohde S, Böhm M, Berkefeld J, Scharrer I, et al. Increased incidence of thrombophilic abnormalities in patients with cranial dural arteriovenous fistulae. Neurol Res. 2003; 25:745–748. PMID: 14579793.
Article7. Hu YC, Newman CB, Dashti SR, Albuquerque FC, McDougall CG. Cranial dural arteriovenous fistula : transarterial Onyx embolization experience and technical nuances. J Neurointerv Surg. 2011; 3:5–13. PMID: 21990779.
Article8. Kerber CW, Newton TH. The macro and microvasculature of the dura mater. Neuroradiology. 1973; 6:175–179. PMID: 4772438.
Article9. Kiyosue H, Hori Y, Okahara M, Tanoue S, Sagara Y, Matsumoto S, et al. Treatment of intracranial dural arteriovenous fistulas : current strategies based on location and hemodynamics, and alternative techniques of transcatheter embolization. Radiographics. 2004; 24:1637–1653. PMID: 15537974.
Article10. Kojima T, Miyachi S, Sahara Y, Nakai K, Okamoto T, Hattori K, et al. The relationship between venous hypertension and expression of vascular endothelial growth factor : hemodynamic and immunohistochemical examinations in a rat venous hypertension model. Surg Neurol. 2007; 68:277–284. discussion 284PMID: 17719966.
Article11. Lv X, Jiang C, Li Y, Wu Z. Results and complications of transarterial embolization of intracranial dural arteriovenous fistulas using Onyx-18. J Neurosurg. 2008; 109:1083–1090. PMID: 19035723.
Article12. Nabors MW, Azzam CJ, Albanna FJ, Gulya AJ, Davis DO, Kobrine AI. Delayed postoperative dural arteriovenous malformations. Report of two cases. J Neurosurg. 1987; 66:768–772. PMID: 3572502.13. Natarajan SK, Ghodke B, Kim LJ, Hallam DK, Britz GW, Sekhar LN. Multimodality treatment of intracranial dural arteriovenous fistulas in the Onyx era : a single center experience. World Neurosurg. 2010; 73:365–379. PMID: 20849795.
Article14. Nogueira RG, Dabus G, Rabinov JD, Eskey CJ, Ogilvy CS, Hirsch JA, et al. Preliminary experience with onyx embolization for the treatment of intracranial dural arteriovenous fistulas. AJNR Am J Neuroradiol. 2008; 29:91–97. PMID: 17974618.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular management of cavernous sinus dural arteriovenous fistulas: Overall review and considerations
- Role of surgery in management of intracranial dural arteriovenous fistulas
- Tentorial Dural Arteriovenous Fistulas: A Single-Center Cohort of 12 Patients
- Stereotactic radiosurgery for dural arteriovenous fistula
- Endovascular Treatment of Dural Sinus Malformation in Infant: A Case Report