Chonnam Med J.
2016 Jan;52(1):64-69. 10.4068/cmj.2016.52.1.64.
Clinical and Laboratory Characteristics of Childhood Diabetes Mellitus: A Single-Center Study from 2000 to 2013
- Affiliations
-
- 1Department of Pediatrics, Chonbuk National University Medical School, Jeonju, Korea. children@jbnu.ac.kr
- 2Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Institute of Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2152658
- DOI: http://doi.org/10.4068/cmj.2016.52.1.64
Abstract
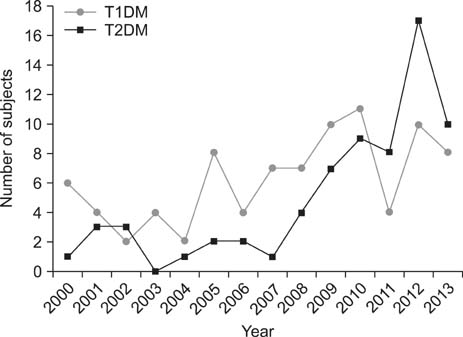
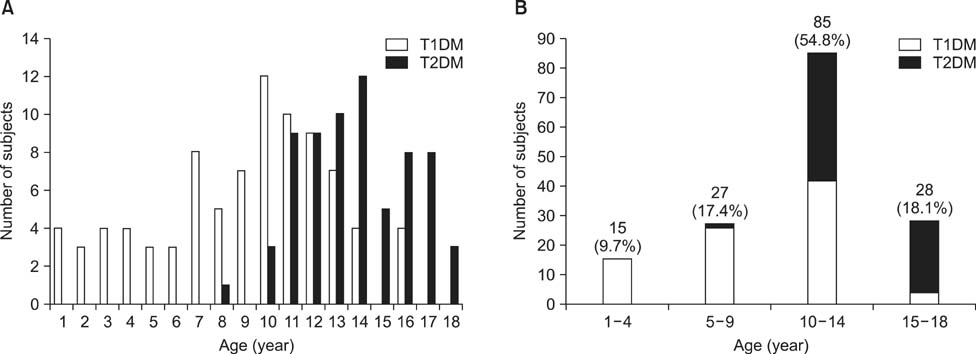
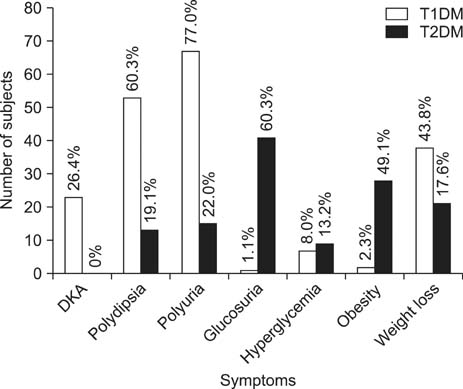
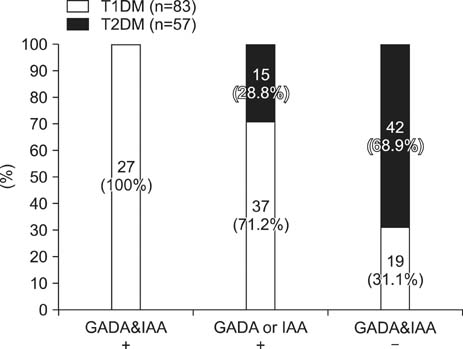
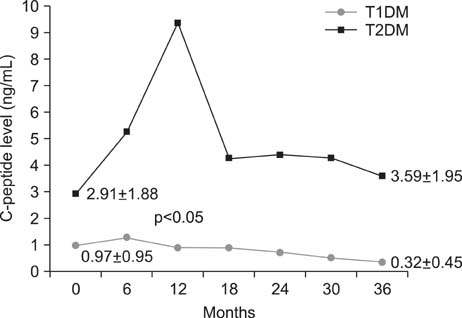
- We examined the clinical and laboratory characteristics of children newly diagnosed with diabetes mellitus (DM) in a single-center study. We retrospectively reviewed the data of 155 children with DM between January 2000 and December 2013. Of 155 diabetic children, 87 (56.1%) were diagnosed with type 1 DM (T1DM) and 68 (43.9%) with type 2 DM (T2DM). Mean ages at diagnosis were 8.95+/-3.89 years (T1DM) and 13.76+/-2.23 years (T2DM), respectively (p<0.001). There were significant differences in HbA1c, C-peptide, and glutamic acid decarboxylase antibody levels between the T1DM and T2DM groups. Annual numbers of children with DM have increased, and since 2011 the number of children with T2DM has surpassed the number with T1DM. The most common clinical symptom in T1DM was polyuria, and 26.4% of children with T1DM presented initially with diabetic ketoacidosis. In contrast, 60.3% of T2DM children showed glucosuria in a school urine screening, and only 19.1% presented with polydipsia. The rate of positivity for at least more than one islet autoantibody was 77.1% in T1DM and 26.3% in T2DM. Serum C-peptide levels in T2DM were increased up to 12 months after onset and remained >3.59 ng/mL for 36 months. However, serum C-peptide levels in T1DM were slightly increased up to 6 months after onset and gradually decreased to 0.32 ng/mL for 36 months. The prevalence of children with DM has increased over the last 14 years, and the proportion of T2DM patients has rapidly increased since 2009. Because childhood DM is associated with several metabolic and cardiovascular complications, children should be screened for early detection of DM, especially asymptomatic T2DM in children and adolescents.
Keyword
MeSH Terms
Figure
Reference
-
1. Dejkhamron P, Menon RK, Sperling MA. Childhood diabetes mellitus: recent advances & future prospects. Indian J Med Res. 2007; 125:231–250.2. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997; 20:1183–1197.3. Sperling MA. Diabetes Mellitus. In : Sperling MA, editor. Pediatric endocrinology. 2nd ed. Philadelphia: Saunders;2002. p. 323–366.4. Aanstoot HJ, Anderson BJ, Daneman D, Danne T, Donaghue K, Kaufman F, et al. The global burden of youth diabetes: perspectives and potential. Pediatr Diabetes. 2007; 8:Suppl 8. 1–44.5. Devendra D, Liu E, Eisenbarth GS. Type 1 diabetes: recent developments. BMJ. 2004; 328:750–754.
Article6. Ize-Ludlow D, Sperling MA. The classification of diabetes mellitus: a conceptual framework. Pediatr Clin North Am. 2005; 52:1533–1552.
Article7. Reinehr T. Type 2 diabetes mellitus in children and adolescents. World J Diabetes. 2013; 4:270–281.
Article8. Arslanian S. Type 2 diabetes in children: clinical aspects and risk factors. Horm Res. 2002; 57:Suppl 1. 19–28.
Article9. Craig ME, Hattersley A, Donaghue KC. Definition, epidemiology and classification of diabetes in children and adolescents. Pediatr Diabetes. 2009; 10:Suppl 12. 3–12.
Article10. Barrett TG. Non autoimmune forms of diabetes: Neonatal diabetes, DIDMOAAD-Wolfram, and related syndromes. In : Sperling MA, editor. Type 1 Diabetes. Totowa: Humana Press;2003. p. 163–182.11. Porter JR, Barrett TG. Acquired non-type 1 diabetes in childhood: subtypes, diagnosis, and management. Arch Dis Child. 2004; 89:1138–1144.
Article12. Samuelsson U, Stenhammar L. Clinical characteristics at onset of Type 1 diabetes in children diagnosed between 1977 and 2001 in the south-east region of Sweden. Diabetes Res Clin Pract. 2005; 68:49–55.
Article13. Hekkala A, Knip M, Veijola R. Ketoacidosis at diagnosis of type 1 diabetes in children in northern Finland: temporal changes over 20 years. Diabetes Care. 2007; 30:861–866.
Article14. Morimoto A, Nishimura R, Tajima N. Trends in the epidemiology of patients with diabetes in Japan. JMAJ. 2010; 53:36–40.15. Lee CW, Shin HJ, Kim DH. Prevalence of autoimmune antibodies in type i diabetic children and their siblings. J Korean Soc Pediatr Endocrinol. 1999; 4:78–87.16. Hong EH, Park JS, Lee HS, Cho MH, Ko CW. Clinical characteristics and laboratory findings of children who were newly diagnosed with diabetes mellitus (From 2001 to 2008). J Korean Soc Pediatr Endocrinol. 2009; 14:110–115.17. Yu J, Shin CH, Yang SW, Park MH, Eisenbarth GS. Analysis of children with type 1 diabetes in Korea: high prevalence of specific anti-islet autoantibodies, immunogenetic similarities to Western populations with "unique" haplotypes, and lack of discrimination by aspartic acid at position 57 of DQB. Clin Immunol. 2004; 113:318–325.
Article18. Klingensmith GJ, Pyle L, Arslanian S, Copeland KC, Cuttler L, Kaufman F, et al. The presence of GAD and IA-2 antibodies in youth with a type 2 diabetes phenotype: results from the TODAY study. Diabetes Care. 2010; 33:1970–1975.
Article19. Kong YH, Kim MS, Lee DY. Comparison of the prevalence of islet autoantibodies according to age and disease duration in patients with type 1 diabetes mellitus. Ann Pediatr Endocrinol Metab. 2013; 18:65–70.
Article20. Katz LE, Jawad AF, Ganesh J, Abraham M, Murphy K, Lipman TH. Fasting c-peptide and insulin-like growth factor-binding protein-1 levels help to distinguish childhood type 1 and type 2 diabetes at diagnosis. Pediatr Diabetes. 2007; 8:53–59.
Article21. Cho MJ, Kim MS, Kim CJ, Kim EY, Kim JD, Kim EY, et al. Fasting serum C-peptide is useful for initial classification of diabetes mellitus in children and adolescents. Ann Pediatr Endocrinol Metab. 2014; 19:80–85.
Article22. Besser RE. Determination of C-peptide in children: when is it useful. Pediatr Endocrinol Rev. 2013; 10:494–502.23. Jones AG, Hattersley AT. The clinical utility of C-peptide measurement in the care of patients with diabetes. Diabet Med. 2013; 30:803–817.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Genetics in Diabetes Mellitus - Contribution to the Classification and Management
- Comparison of Insulin-Treated Patients with Ambiguous Diabetes Type with Definite Type 1 and Type 2 Diabetes Mellitus Subjects: A Clinical Perspective
- Genetic Diseases Associated with Diabetes Mellitus
- Diabetes Mellitus and Tuberculosis
- Childhood diabetes in India