Gestational age at delivery and neonatal outcome in uncomplicated twin pregnancies: what is the optimal gestational age for delivery according to chorionicity?
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. drmaxmix.choi@samsung.com
- KMID: 2152638
- DOI: http://doi.org/10.5468/ogs.2016.59.1.9
Abstract
OBJECTIVE
To investigate the neonatal outcome according to the gestational age at delivery and to determine the optimal timing for delivery in uncomplicated monochorionic and dichorionic twin pregnancies.
METHODS
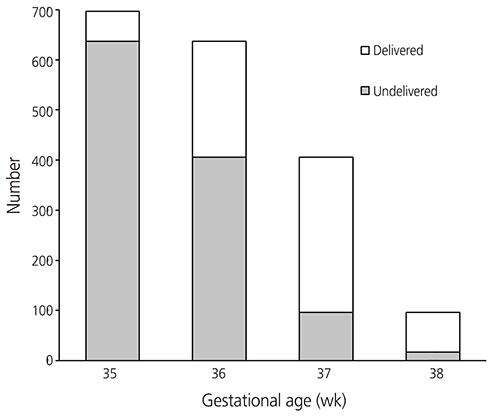
This is a retrospective cohort study of women with uncomplicated twin pregnancies delivered at or beyond 35 weeks of gestation from 1995 to 2013. The primary outcome was neonatal composite morbidity, which was defined as when either one or both twins have one or more of the followings: fetal death after 35 weeks gestation, admission to neonatal intensive care unit, mechanical ventilator requirement, respiratory distress syndrome and neonatal death. To determine the optimal gestational age for delivery according to chorionicity, we compared the neonatal composite morbidity rate between women who delivered and women who remained undelivered at each gestational week in both monochorionic and dichorionic twin pregnancies.
RESULTS
A total of 697 twin pregnancies were included (171 monochorionic and 526 dichorionic twins). The neonatal composite morbidity rate significantly decreased with advancing gestational age at delivery and its nadir was observed at 38 and > or =39 weeks of gestation in monochorionic and dichorionic twins, respectively. However, the composite morbidity rate did not differ between women who delivered and women who remained undelivered > or =36 and > or =37 weeks in monochorionic and dichorionic twins, respectively.
CONCLUSION
Our data suggest that the optimal gestational age for delivery was at > or =36 and > or =37 weeks in uncomplicated monochorionic and dichorionic twin pregnancies, respectively.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Changes in the perinatal outcomes of twin pregnancies delivered at a tertiary referral center in Korea during a 24-year period from 1995 to 2018
Ji Young Hong, Hye Ran Lee, Yejin Kim, Yoo-Min Kim, Ji-Hee Sung, Suk-Joo Choi, Soo-young Oh, Cheong-Rae Roh
Obstet Gynecol Sci. 2020;63(3):251-260. doi: 10.5468/ogs.2020.63.3.251.Optimal Timing of Delivery Based on the Risk of Stillbirth and Infant Death Associated with Each Additional Week of Expectant Management in Multiple Pregnancies: a National Cohort Study of Koreans
Hyun Sun Ko, Sae Kyung Choi, Jeong Ha Wie, In Yang Park, Yong Gyu Park, Jong Chul Shin
J Korean Med Sci. 2018;33(10):. doi: 10.3346/jkms.2018.33.e80.Comparison of perinatal outcomes in late preterm birth between singleton and twin pregnancies
Eun-Hye Yoo, Dasom Chun, Mi Ju Kim, Hyun-Hwa Cha, Won Joon Seong
Obstet Gynecol Sci. 2017;60(5):421-426. doi: 10.5468/ogs.2017.60.5.421.
Reference
-
1. Committee for Assisted Reproductive Technology. Korean Society of Obstetrics and Gynecology. Choi YM, Chun SS, Han HD, Hwang JH, et al. Current status of assisted reproductive technology in Korea, 2009. Obstet Gynecol Sci. 2013; 56:353–361.2. Lee GH, Song HJ, Lee KS, Choi YM. Current status of assisted reproductive technology in Korea, 2010. Clin Exp Reprod Med. 2015; 42:8–13.3. Korea Institute for Health and Social Affairs. Health and welfare data portal [Internet]. Sejong: Korea Institute for Health and Social Affairs;cited 2015 Mar 20. Available from: https://data.kihasa.re.kr/index.jsp.4. Newman RB, Unal ER. Multiple gestations: timing of indicated late preterm and early-term births in uncomplicated dichorionic, monochorionic, and monoamniotic twins. Semin Perinatol. 2011; 35:277–285.5. Blickstein I, Goldman RD, Mazkereth R. Risk for one or two very low birth weight twins: a population study. Obstet Gynecol. 2000; 96:400–402.6. Lee CM, Yang SH, Lee SP, Hwang BC, Kim SY. Clinical factors affecting the timing of delivery in twin pregnancies. Obstet Gynecol Sci. 2014; 57:436–441.7. Dodd JM, Crowther CA, Haslam RR, Robinson JS. Timing of birth for women with a twin pregnancy at term: a randomised controlled trial. BMC Pregnancy Childbirth. 2010; 10:68.8. Cheung YB, Yip P, Karlberg J. Mortality of twins and singletons by gestational age: a varying-coefficient approach. Am J Epidemiol. 2000; 152:1107–1116.9. van Baaren GJ, Peelen MJ, Schuit E, van der Post JA, Mol BW, Kok M, et al. Preterm birth in singleton and multiple pregnancies: evaluation of costs and perinatal outcomes. Eur J Obstet Gynecol Reprod Biol. 2015; 186:34–41.10. Dodd JM, Deussen AR, Grivell RM, Crowther CA. Elective birth at 37 weeks' gestation for women with an uncomplicated twin pregnancy. Cochrane Database Syst Rev. 2014; 2:CD003582.11. Lee YM. Delivery of twins. Semin Perinatol. 2012; 36:195–200.12. Vilchez GA, Dai J, Hoyos LR, Chelliah A, Bahado-Singh R, Sokol RJ. Optimal timing for term delivery of twin pregnancies: a population-based study. Am J Perinatol. 2015; 32:487–496.13. Vergani P, Russo FM, Follesa I, Cozzolino S, Fedeli T, Ventura L, et al. Perinatal complications in twin pregnancies after 34 weeks: effects of gestational age at delivery and chorionicity. Am J Perinatol. 2013; 30:545–550.14. Hartley RS, Emanuel I, Hitti J. Perinatal mortality and neonatal morbidity rates among twin pairs at different gestational ages: optimal delivery timing at 37 to 38 weeks' gestation. Am J Obstet Gynecol. 2001; 184:451–458.15. Doss AE, Mancuso MS, Cliver SP, Jauk VC, Jenkins SM. Gestational age at delivery and perinatal outcomes of twin gestations. Am J Obstet Gynecol. 2012; 207:410.e1–410.e6.16. Kahn B, Lumey LH, Zybert PA, Lorenz JM, Cleary-Goldman J, D'Alton ME, et al. Prospective risk of fetal death in singleton, twin, and triplet gestations: implications for practice. Obstet Gynecol. 2003; 102:685–692.17. Minakami H, Sato I. Reestimating date of delivery in multifetal pregnancies. JAMA. 1996; 275:1432–1434.18. Lewi L, Van Schoubroeck D, Gratacos E, Witters I, Timmerman D, Deprest J. Monochorionic diamniotic twins: complications and management options. Curr Opin Obstet Gynecol. 2003; 15:177–194.19. Van Mieghem T, De Heus R, Lewi L, Klaritsch P, Kollmann M, Baud D, et al. Prenatal management of monoamniotic twin pregnancies. Obstet Gynecol. 2014; 124:498–506.20. National Institute for Health and Clinical Excellence. Antenatal management of multiple gestations: NICE clinical guideline 129 [Internet]. London: National Institute for Health and Care Excellence;c2011. cited 2015 Mar 20. http://guidance.nice.org.uk/CG129.21. Spong CY, Mercer BM, D'alton M, Kilpatrick S, Blackwell S, Saade G. Timing of indicated late-preterm and early-term birth. Obstet Gynecol. 2011; 118(2 Pt 1):323–333.22. Robinson BK, Miller RS, D'Alton ME, Grobman WA. Effectiveness of timing strategies for delivery of monochorionic diamniotic twins. Am J Obstet Gynecol. 2012; 207:53.e1–53.e7.23. Dias T, Akolekar R. Timing of birth in multiple pregnancy. Best Pract Res Clin Obstet Gynaecol. 2014; 28:319–326.24. Burgess JL, Unal ER, Nietert PJ, Newman RB. Risk of late-preterm stillbirth and neonatal morbidity for monochorionic and dichorionic twins. Am J Obstet Gynecol. 2014; 210:578.e1–578.e9.25. Hack KE, Derks JB, Elias SG, Franx A, Roos EJ, Voerman SK, et al. Increased perinatal mortality and morbidity in monochorionic versus dichorionic twin pregnancies: clinical implications of a large Dutch cohort study. BJOG. 2008; 115:58–67.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Successful Delayed-Interval Delivery without Cerclage Operation after One Fetal Delivery in a Case of Twin Pregnancy
- Twin Pregnancies with One Fetal Demise
- Effects of Single Fetal Death on Mother and Live Co-twin in Twin Pregnancy
- Twin Gestations with a Single Anomalous Fetus
- Twin pregnancies conceived by In-vitro fertilization compared with normally conceived twin pregnancies: Maternal and neonatal outcome