J Korean Soc Radiol.
2016 Feb;74(2):114-122. 10.3348/jksr.2016.74.2.114.
Anomalies of Abdominal Organs in Polysplenia Syndrome: Multidetector Computed Tomography Findings
- Affiliations
-
- 1Department of Radiology, Dongguk University Ilsan Hospital, Dongguk University School of Medicine, Goyang, Korea. yslee@dumc.or.kr
- KMID: 2152603
- DOI: http://doi.org/10.3348/jksr.2016.74.2.114
Abstract
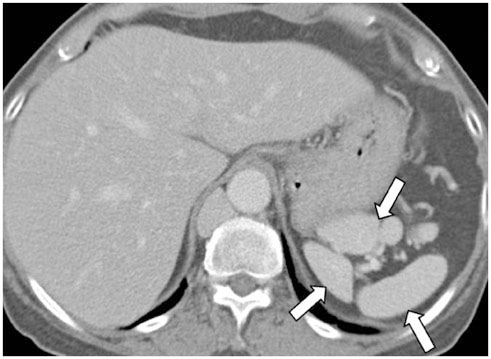
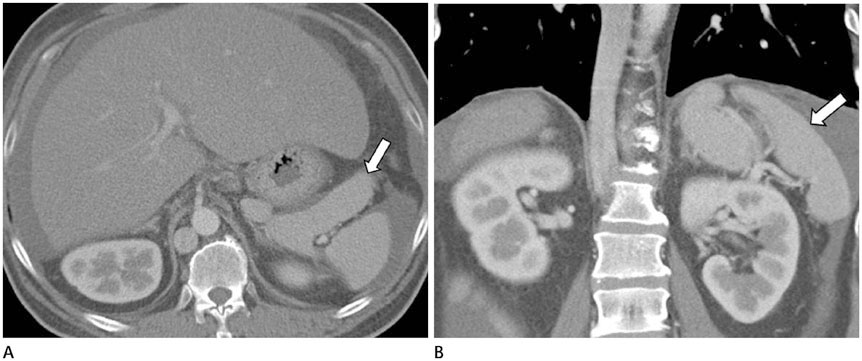
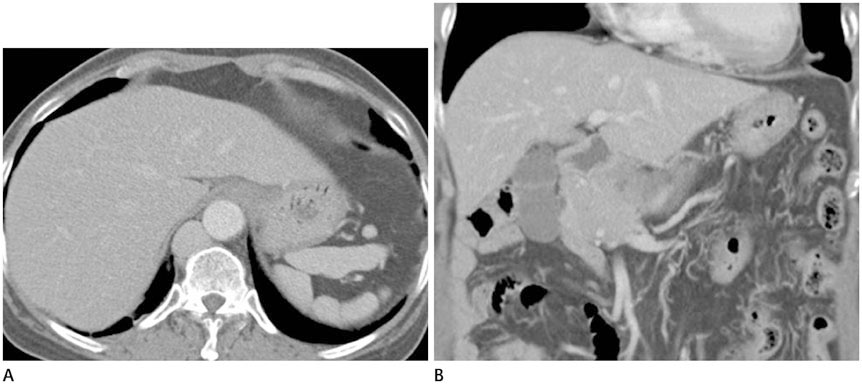
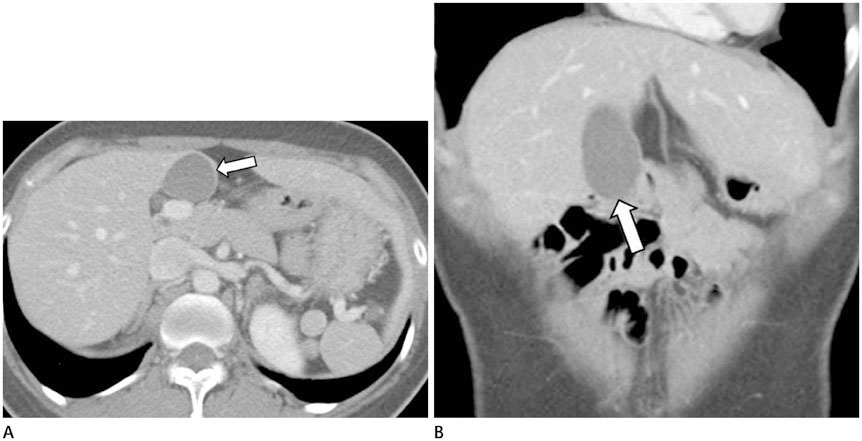
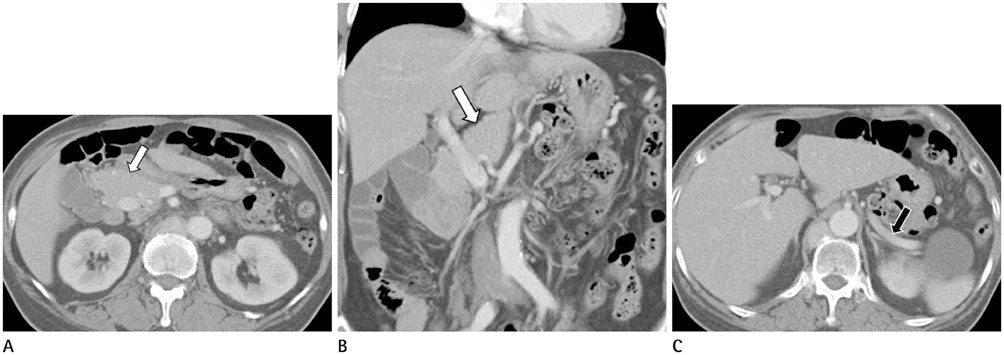
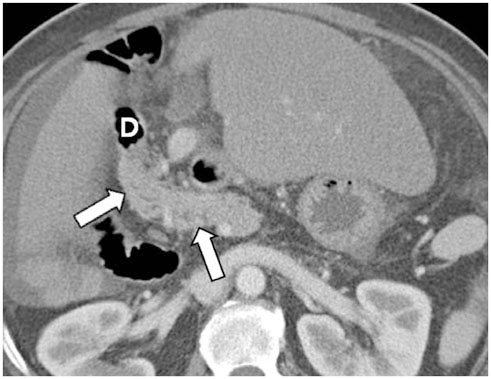
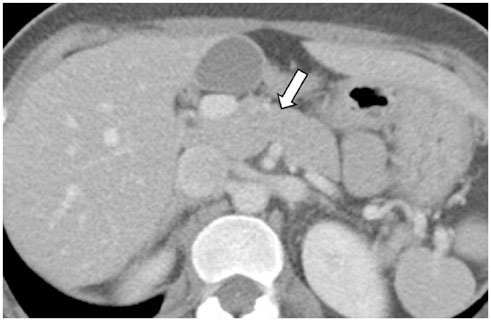
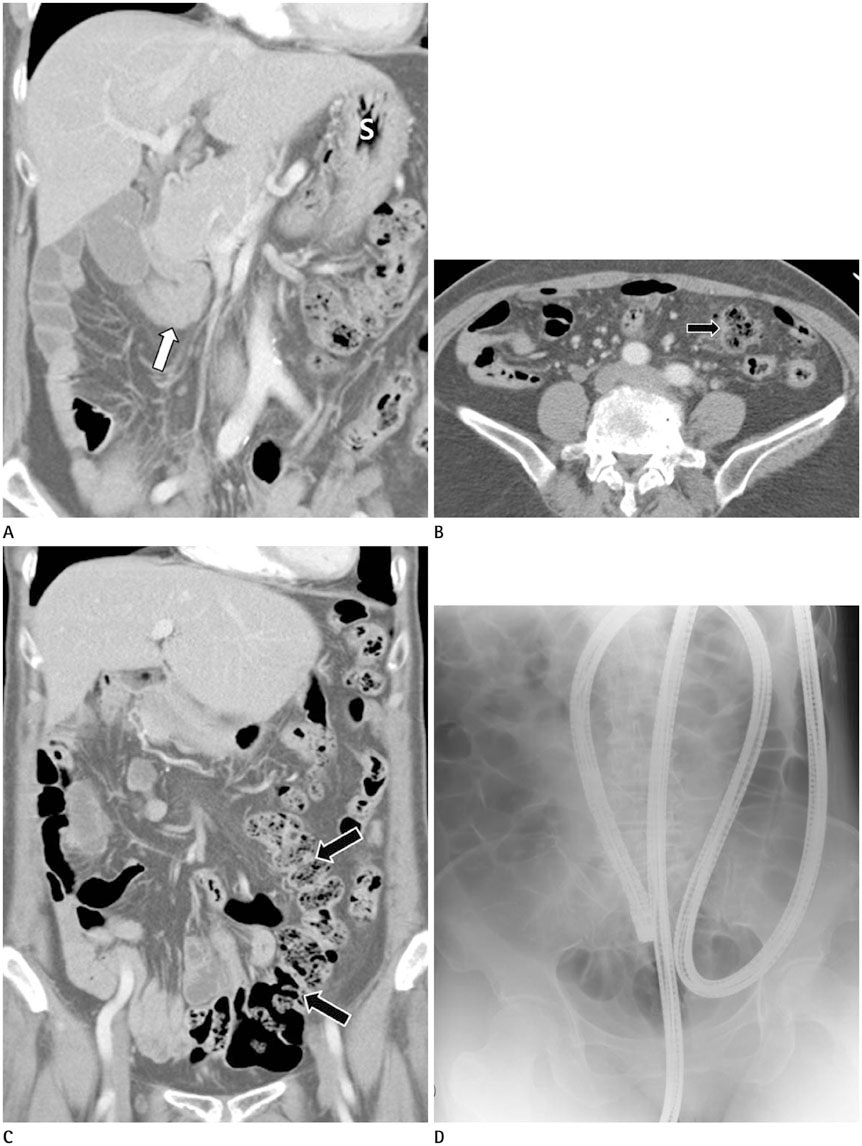
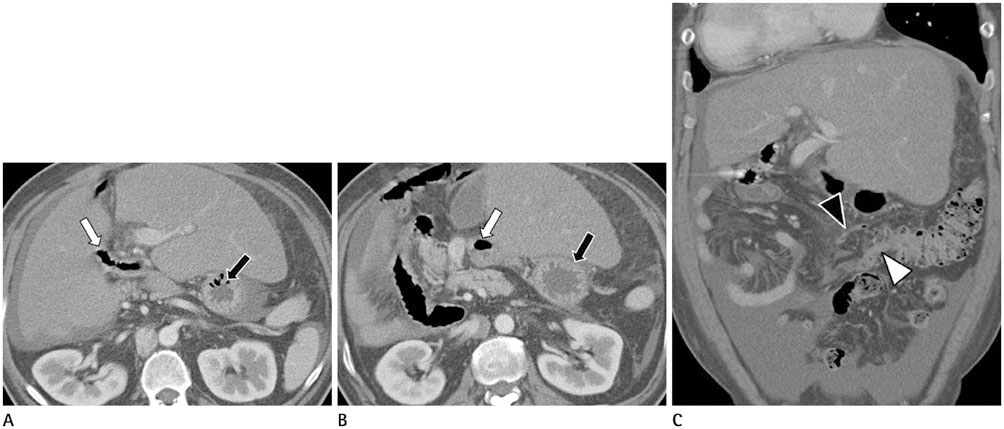
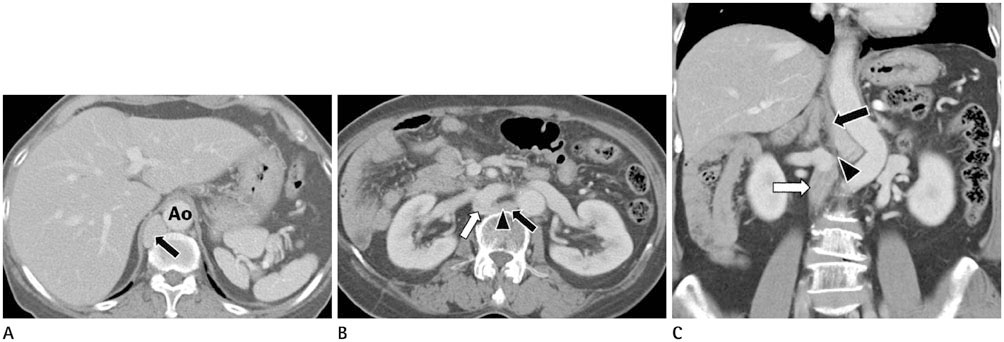
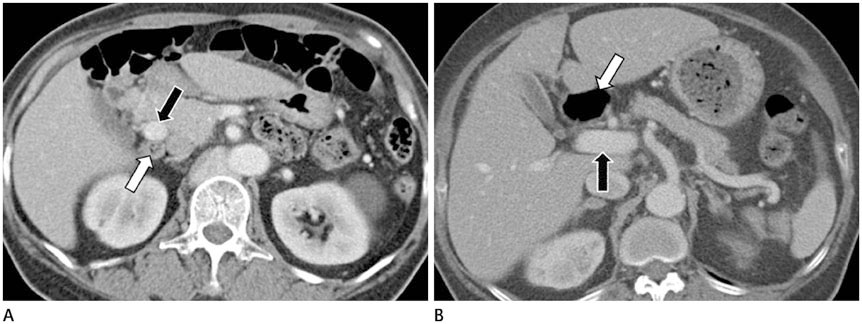
- Polysplenia syndrome is a rare situs ambiguous anomaly associated with multiple spleens and anomalies of abdominal organs. Because most of the minor anomalies do not cause clinical symptoms, polysplenia syndrome is detected incidentally in the adults. Anomalies of abdominal organs may include multiple spleens of variable size or right-sided spleen, large midline or left-sided liver, midline gallbladder, biliary tract anomalies, short pancreas, right-sided stomach, intestinal malrotation, inferior vena cava interruption with azygos or hemiazygos continuation, and a preduodenal portal vein. As the multidetector computed tomography is increasingly used, situs anomalies will likely to be found with greater frequency in the adults. Therefore, radiologists should become familiar with these rare and peculiar anomalies of abdominal organs in polysplenia syndrome.
MeSH Terms
Figure
Reference
-
1. Muneta S, Sakai S, Fukuda H, Imamura Y, Matsumoto I. Polysplenia syndrome with various visceral anomalies in an adult: embryological and clinical considerations. Intern Med. 1992; 31:1026–1031.2. Fulcher AS, Turner MA. Abdominal manifestations of situs anomalies in adults. Radiographics. 2002; 22:1439–1456.3. Applegate KE, Goske MJ, Pierce G, Murphy D. Situs revisited: imaging of the heterotaxy syndrome. Radiographics. 1999; 19:837–852. discussion 853-8544. Gayer G, Apter S, Jonas T, Amitai M, Zissin R, Sella T, et al. Polysplenia syndrome detected in adulthood: report of eight cases and review of the literature. Abdom Imaging. 1999; 24:178–184.5. Peoples WM, Moller JH, Edwards JE. Polysplenia: a review of 146 cases. Pediatr Cardiol. 1983; 4:129–137.6. Winer-Muram HT, Tonkin IL. The spectrum of heterotaxic syndromes. Radiol Clin North Am. 1989; 27:1147–1170.7. Esscher T. Preduodenal portal vein--a cause of intestinal obstruction? J Pediatr Surg. 1980; 15:609–612.8. Gayer G, Zissin R, Apter S, Atar E, Portnoy O, Itzchak Y. CT findings in congenital anomalies of the spleen. Br J Radiol. 2001; 74:767–772.9. Chandra RS. Biliary atresia and other structural anomalies in the congenital polysplenia syndrome. J Pediatr. 1974; 85:649–655.10. Gagner M, Munson JL, Scholz FJ. Hepatobiliary anomalies associated with polysplenia syndrome. Gastrointest Radiol. 1991; 16:167–171.11. Kobayashi H, Kawamoto S, Tamaki T, Konishi J, Togashi K. Polysplenia associated with semiannular pancreas. Eur Radiol. 2001; 11:1639–1641.12. Maier M, Wiesner W, Mengiardi B. Annular pancreas and agenesis of the dorsal pancreas in a patient with polysplenia syndrome. AJR Am J Roentgenol. 2007; 188:W150–W153.13. Kapa S, Gleeson FC, Vege SS. Dorsal pancreas agenesis and polysplenia/heterotaxy syndrome: a novel association with aortic coarctation and a review of the literature. JOP. 2007; 8:433–437.14. Jeong JH, Kim GH, Song GA, Lee DG, Moon JY, Cheong JH, et al. Polysplenia syndrome with congenital agenesis of dorsal pancreas presenting as acute pancreatitis and the role of endoscopic ultrasonography in its diagnosis. Korean J Gastroenterol. 2012; 60:47–51.15. Rakesh K, Choung OW, Reddy DN. Agenesis of the dorsal pancreas (ADP) and pancreatitis - is there an association? Indian J Gastroenterol. 2006; 25:35–36.16. Nishimori I, Okazaki K, Morita M, Miyao M, Sakamoto Y, Kagiyama S, et al. Congenital hypoplasia of the dorsal pancreas: with special reference to duodenal papillary dysfunction. Am J Gastroenterol. 1990; 85:1029–1033.17. Gold RP. Agenesis and pseudo-agenesis of the dorsal pancreas. Abdom Imaging. 1993; 18:141–144.18. Ditchfield MR, Hutson JM. Intestinal rotational abnormalities in polysplenia and asplenia syndromes. Pediatr Radiol. 1998; 28:303–306.19. Miyabara S, Sugihara H, Kamio A, Oota K, Abe H, Kato S. Atypical polysplenia only with absence of the hepatic segment of inferior vena cava in a middle-aged. Acta Pathol Jpn. 1984; 34:111–116.20. Seo HI, Jeon TY, Sim MS, Kim S. Polysplenia syndrome with preduodenal portal vein detected in adults. World J Gastroenterol. 2008; 14:6418–6420.21. Ishizaki Y, Tanaka M, Okuyama T. Surgical implications of preduodenal portal vein in the adult. Case report and review of the literature. Arch Surg. 1994; 129:773–777.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Absence of the Intrahepatic Inferior Vena Cava with Polysplenia Syndrome on Multidetector Computed Tomography: A Case Report
- Congenital Anomalies of the Aortic Arch: Evaluation with the Use of Multidetector Computed Tomography
- A Case of Scimitar Syndrome with H-Type Tracheoesophageal Fistula and Multiple Anomalies: Diagnosis Using Electrocardiography-Gated Chest CT
- Multidetector CT in Blunt Abdominal Trauma: Imaging Findings and Pitfalls
- Recent Progress in Abdominal CT Imaging