Cancer Res Treat.
2016 Jan;48(1):37-44. 10.4143/crt.2014.259.
Hypofractionated Stereotactic Radiation Therapy in Recurrent High-Grade Glioma: A New Challenge
- Affiliations
-
- 1Department of Radiotherapy and Radiosurgery, Istituto Clinico Humanitas Cancer Center and Research Hospital, Milano, Italy. piera.navarria@cancercenter.humanitas.it
- 2Department of Neurosurgical Oncology, Istituto Clinico Humanitas Cancer Center and Research Hospital, Milano, Italy.
- KMID: 2152258
- DOI: http://doi.org/10.4143/crt.2014.259
Abstract
- PURPOSE
The aim of this study was to evaluate outcomes of hypofractionated stereotactic radiation therapy (HSRT) in patients re-treated for recurrent high-grade glioma.
MATERIALS AND METHODS
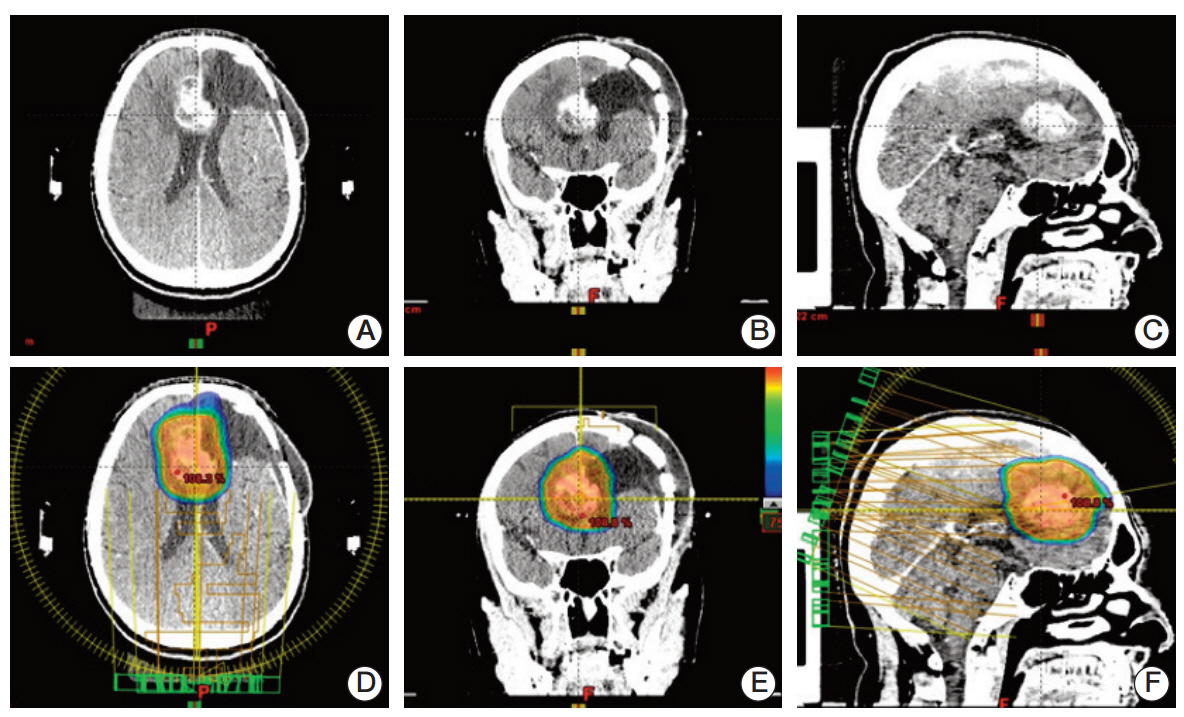
From January 2006 to September 2013, 25 patients were treated. Six patients underwent radiation therapy alone, while 19 underwent combined treatment with surgery and/or chemotherapy. Only patients with Karnofsky Performance Status (KPS) > 70 and time from previous radiotherapy greater than 6 months were re-irradiated. The mean recurrent tumor volume was 35 cm3 (range, 2.46 to 116.7 cm3), and most of the patients (84%) were treated with a total dose of 25 Gy in five fractions (range, 20 to 50 Gy in 5-10 fractions).
RESULTS
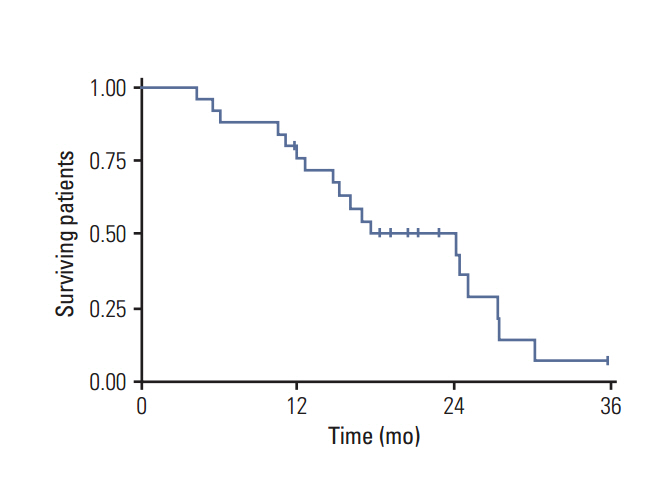
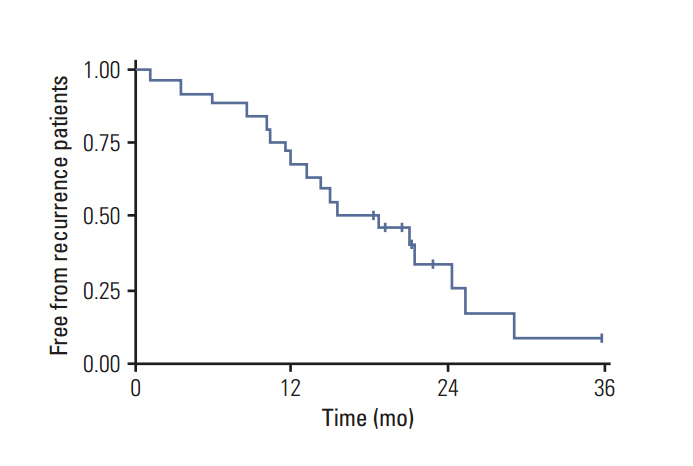
The median follow-up was 18 months (range, 4 to 36 months). The progression-free survival (PFS) at 1 and 2 years was 72% and 34% and the overall survival (OS) 76% and 50%, respectively. No severe toxicity was recorded. In univariate and multivariate analysis extent of resection at diagnosis significantly influenced PFS and OS (p < 0.01). Patients with smaller recurren tumor volume treated had better local control and survival. Indeed, the 2-year PFS was 40% (< or = 50 cm3) versus 11% (p=0.1) and the 2-year OS 56% versus 33% (> 50 cm3), respectively (p=0.26).
CONCLUSION
In our experience, HSRT could be a safe and feasible therapeutic option for recurrent high grade glioma even in patients with larger tumors. We believe that a multidisciplinary evaluation is mandatory to assure the best treatment for selected patients. Local treatment should also be considered as part of an integrated approach.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Interim Tumor Progression and Volumetric Changes of Surgical Cavities during the Surgery-to-Radiotherapy Interval in Anaplastic Gliomas: Implications for Additional Pre-radiotherapy Magnetic Resonance Imaging
Chan Woo Wee, Il Han Kim, Chul-Kee Park, Jin Wook Kim
Cancer Res Treat. 2020;52(2):524-529. doi: 10.4143/crt.2019.520.
Reference
-
References
1. Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009; 10:459–66.
Article2. National Comprehensive Cancer Network. NCCN guidelines: central nervous system cancers 2012 [Internet]. Fort Washington, PA: National Comprehensive Cancer Network;2012. [cited 2014 Dec 1]. Available from: http://www.nccn.org/professionals/physiciangls/f/guidelines.asp.3. Minniti G, Amelio D, Amichetti M, Salvati M, Muni R, Bozzao A, et al. Patterns of failure and comparison of different target volume delineations in patients with glioblastoma treated with conformal radiotherapy plus concomitant and adjuvant temozolomide. Radiother Oncol. 2010; 97:377–81.
Article4. Garden AS, Maor MH, Yung WK, Bruner JM, Woo SY, Moser RP, et al. Outcome and patterns of failure following limited-volume irradiation for malignant astrocytomas. Radiother Oncol. 1991; 20:99–110.
Article5. Hess CF, Schaaf JC, Kortmann RD, Schabet M, Bamberg M. Malignant glioma: patterns of failure following individually tailored limited volume irradiation. Radiother Oncol. 1994; 30:146–9.6. Barbagallo GM, Jenkinson MD, Brodbelt AR. 'Recurrent' glioblastoma multiforme, when should we reoperate? Br J Neurosurg. 2008; 22:452–5.
Article7. Park JK, Hodges T, Arko L, Shen M, Dello Iacono D, McNabb A, et al. Scale to predict survival after surgery for recurrent glioblastoma multiforme. J Clin Oncol. 2010; 28:3838–43.
Article8. Wick W, Platten M, Weller M. New (alternative) temozolomide regimens for the treatment of glioma. Neuro Oncol. 2009; 11:69–79.
Article9. Wick W, Weller M, Weiler M, Batchelor T, Yung AW, Platten M. Pathway inhibition: emerging molecular targets for treating glioblastoma. Neuro Oncol. 2011; 13:566–79.
Article10. Combs SE, Gutwein S, Thilmann C, Huber P, Debus J, Schulz-Ertner D. Stereotactically guided fractionated re-irradiation in recurrent glioblastoma multiforme. J Neurooncol. 2005; 74:167–71.
Article11. Combs SE, Widmer V, Thilmann C, Hof H, Debus J, Schulz-Ertner D, et al. Stereotactic radiosurgery (SRS): treatment option for recurrent glioblastoma multiforme (GBM). Cancer. 2005; 104:2168–73.12. Biswas T, Okunieff P, Schell MC, Smudzin T, Pilcher WH, Bakos RS, et al. Stereotactic radiosurgery for glioblastoma:retrospective analysis. Radiat Oncol. 2009; 4:11.
Article13. Fuller CD, Choi M, Forthuber B, Wang SJ, Rajagiriyil N, Salter BJ, et al. Standard fractionation intensity modulated radiation therapy (IMRT) of primary and recurrent glioblastoma multiforme. Radiat Oncol. 2007; 2:26.
Article14. Ang KK, Price RE, Stephens LC, Jiang GL, Feng Y, Schultheiss TE, et al. The tolerance of primate spinal cord to re-irradiation. Int J Radiat Oncol Biol Phys. 1993; 25:459–64.
Article15. Combs SE, Debus J, Schulz-Ertner D. Radiotherapeutic alternatives for previously irradiated recurrent gliomas. BMC Cancer. 2007; 7:167.
Article16. Hall WA, Djalilian HR, Sperduto PW, Cho KH, Gerbi BJ, Gibbons JP, et al. Stereotactic radiosurgery for recurrent malignant gliomas. J Clin Oncol. 1995; 13:1642–8.
Article17. Kong DS, Lee JI, Park K, Kim JH, Lim DH, Nam DH. Efficacy of stereotactic radiosurgery as a salvage treatment for recurrent malignant gliomas. Cancer. 2008; 112:2046–51.
Article18. Fokas E, Wacker U, Gross MW, Henzel M, Encheva E, Engenhart-Cabillic R. Hypofractionated stereotactic reirradiation of recurrent glioblastomas: a beneficial treatment option after high-dose radiotherapy? Strahlenther Onkol. 2009; 185:235–40.19. Ernst-Stecken A, Ganslandt O, Lambrecht U, Sauer R, Grabenbauer G. Survival and quality of life after hypofractionated stereotactic radiotherapy for recurrent malignant glioma. J Neurooncol. 2007; 81:287–94.
Article20. Henke G, Paulsen F, Steinbach JP, Ganswindt U, Isijanov H, Kortmann RD, et al. Hypofractionated reirradiation for recurrent malignant glioma. Strahlenther Onkol. 2009; 185:113–9.
Article21. Fogh SE, Andrews DW, Glass J, Curran W, Glass C, Champ C, et al. Hypofractionated stereotactic radiation therapy: an effective therapy for recurrent high-grade gliomas. J Clin Oncol. 2010; 28:3048–53.
Article22. Wen PY, Macdonald DR, Reardon DA, Cloughesy TF, Sorensen AG, Galanis E, et al. Updated response assessment criteria for high-grade gliomas: response assessment in neurooncology working group. J Clin Oncol. 2010; 28:1963–72.
Article23. Sanai N, Polley MY, McDermott MW, Parsa AT, Berger MS. An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg. 2011; 115:3–8.
Article24. Amelio D, Amichetti M. Radiation therapy for the treatment of recurrent glioblastoma: an overview. Cancers (Basel). 2012; 4:257–80.
Article25. Easaw JC, Mason WP, Perry J, Laperriere N, Eisenstat DD, Del Maestro R, et al. Canadian recommendations for the treatment of recurrent or progressive glioblastoma multiforme. Curr Oncol. 2011; 18:e126–36.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The mixed era of stereotactic radiosurgery and radiotherapy
- Surgical Experience of Multiple Recurrent Astrocytoma: Case Report
- Intracranial Undifferentiated Sarcoma Arising from a Low-Grade Glioma: A Case Report and Literature Review
- Role of Radiation Therapy for Non-small Cell Lung Cancer: Focused on Stereotactic Ablative Radiation Therapy in Stage I
- Fractionated Stereotactic Radiation Therapy for Intracranial Malignant Tumor: Preliminary Results of Clinical Application