Korean J Pain.
2016 Jan;29(1):40-47. 10.3344/kjp.2016.29.1.40.
Nefopam Reduces Dysesthesia after Percutaneous Endoscopic Lumbar Discectomy
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, School of Medicine, Pusan National University, Yangsan, Korea. pain@pusan.ac.kr
- KMID: 2151659
- DOI: http://doi.org/10.3344/kjp.2016.29.1.40
Abstract
- BACKGROUND
Neuropathic pain, including paresthesia/dysesthesia in the lower extremities, always develops and remains for at least one month, to variable degrees, after percutaneous endoscopic lumbar discectomy (PELD). The recently discovered dual analgesic mechanisms of action, similar to those of antidepressants and anticonvulsants, enable nefopam (NFP) to treat neuropathic pain. This study was performed to determine whether NFP might reduce the neuropathic pain component of postoperative pain.
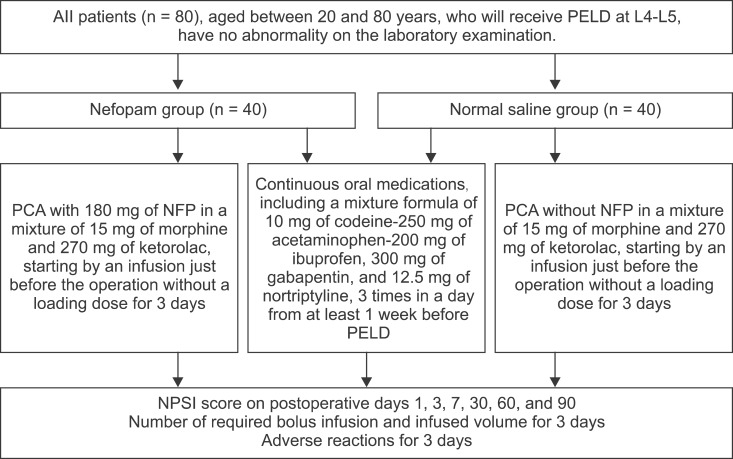
METHODS
Eighty patients, who underwent PELD due to herniated nucleus pulposus (HNP) at L4-L5, were randomly divided into two equal groups, one receiving NFP (with a mixture of morphine and ketorolac) and the other normal saline (NS) with the same mixture. The number of bolus infusions and the infused volume for 3 days were compared in both groups. The adverse reactions (ADRs) in both groups were recorded and compared. The neuropathic pain symptom inventory (NPSI) score was compared in both groups on postoperative days 1, 3, 7, 30, 60, and 90.
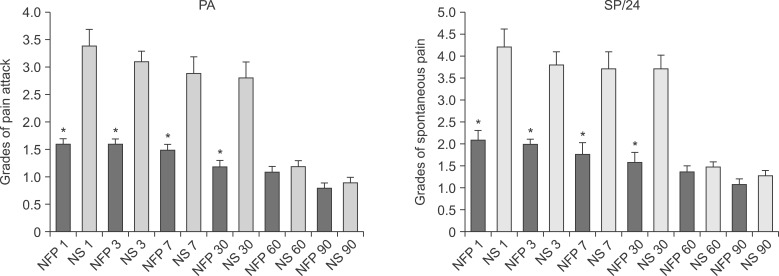
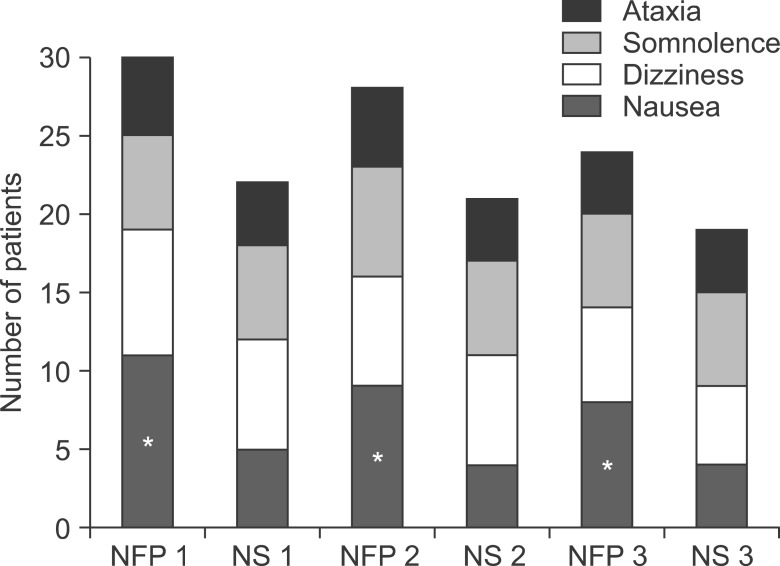
RESULTS
The mean attempted number of bolus infusions, and effective infused bolus volume for 3 days was lower in the NFP group for 3 days. The most commonly reported ADRs were nausea, dizziness, and somnolence, in order of frequency in the NFP group. The median NPSI score, and all 5 median sub-scores in the NFP group, were significantly lower than that of the NS group until postoperative day 30.
CONCLUSIONS
NFP significantly reduced the neuropathic pain component, including paresthesia/dysesthesia until 1 month after PELD. The common ADRs were nausea, dizziness, somnolence, and ataxia.
Keyword
MeSH Terms
-
Anticonvulsants
Antidepressive Agents
Ataxia
Diskectomy*
Diskectomy, Percutaneous
Dizziness
Drug-Related Side Effects and Adverse Reactions
Humans
Infusions, Intravenous
Intervertebral Disc Displacement
Lower Extremity
Morphine
Nausea
Nefopam*
Neuralgia
Pain, Postoperative
Paresthesia*
Symptom Assessment
Anticonvulsants
Antidepressive Agents
Morphine
Nefopam
Figure
Cited by 2 articles
-
Tapentadol: Can It Kill Two Birds with One Stone without Breaking Windows?
Eun Jung Chang, Eun Ji Choi, Kyung Hoon Kim
Korean J Pain. 2016;29(3):153-157. doi: 10.3344/kjp.2016.29.3.153.Earlier treatment improves the chances of complete relief from postherpetic neuralgia
Dong Hee Kang, Su Young Kim, Hyuck Goo Kim, Jung Hyun Park, Tae Kyun Kim, Kyung Hoon Kim
Korean J Pain. 2017;30(3):214-219. doi: 10.3344/kjp.2017.30.3.214.
Reference
-
1. Kim KH. Use of lidocaine patch for percutaneous endoscopic lumbar discectomy. Korean J Pain. 2011; 24:74–80. PMID: 21716614.
Article2. Cho JY, Lee SH, Lee HY. Prevention of development of postoperative dysesthesia in transforaminal percutaneous endoscopic lumbar discectomy for intracanalicular lumbar disc herniation: floating retraction technique. Minim Invasive Neurosurg. 2011; 54:214–218. PMID: 22287030.
Article3. Loeser JD. Pain of neurologic origin in the hips and lower extremities. In : Loeser JD, Bonica JJ, editors. Bonica's management of pain. 3rd ed. Philadelphia (PA): Lippincott Williams & Wilkins;2001. p. 1565–1578.4. Gregori-Puigjané E, Setola V, Hert J, Crews BA, Irwin JJ, Lounkine E, et al. Identifying mechanism-of-action targets for drugs and probes. Proc Natl Acad Sci U S A. 2012; 109:11178–11183. PMID: 22711801.
Article5. Moore RA, Derry S, McQuay HJ, Wiffen PJ. Single dose oral analgesics for acute postoperative pain in adults. Cochrane Database Syst Rev. 2011; CD008659. PMID: 21901726.
Article6. Alfonsi P, Adam F, Passard A, Guignard B, Sessler DI, Chauvin M. Nefopam, a nonsedative benzoxazocine analgesic, selectively reduces the shivering threshold in unanesthetized subjects. Anesthesiology. 2004; 100:37–43. PMID: 14695722.
Article7. Heel RC, Brogden RN, Pakes GE, Speight TM, Avery GS. Nefopam: a review of its pharmacological properties and therapeutic efficacy. Drugs. 1980; 19:249–267. PMID: 6991238.8. Podranski T, Bouillon TW, Riva T, Kurz AM, Oehmke MJ. Compartmental pharmacokinetics of nefopam during mild hypothermia. Br J Anaesth. 2012; 108:784–791. PMID: 22331396.
Article9. Bouhassira D, Attal N, Fermanian J, Alchaar H, Gautron M, Masquelier E, et al. Development and validation of the Neuropathic Pain Symptom Inventory. Pain. 2004; 108:248–257. PMID: 15030944.
Article10. Czuczwar M, Czuczwar K, Cięszczyk J, Kiś J, Saran T, Łuszczki JJ, et al. Nefopam enhances the protective activity of antiepileptics against maximal electroshock-induced convulsions in mice. Pharmacol Rep. 2011; 63:690–696. PMID: 21857079.
Article11. Novelli A, Groppetti A, Rossoni G, Manfredi B, Ferrero-Gutiérrez A, Pérez-Gómez A, et al. Nefopam is more potent than carbamazepine for neuroprotection against veratridine in vitro and has anticonvulsant properties against both electrical and chemical stimulation. Amino Acids. 2007; 32:323–332. PMID: 17021653.
Article12. Novelli A, Díaz-Trelles R, Groppetti A, Fernández-Sánchez MT. Nefopam inhibits calcium influx, cGMP formation, and NMDA receptor-dependent neurotoxicity following activation of voltage sensitive calcium channels. Amino Acids. 2005; 28:183–191. PMID: 15714253.
Article13. Verleye M, André N, Heulard I, Gillardin JM. Nefopam blocks voltage-sensitive sodium channels and modulates glutamatergic transmission in rodents. Brain Res. 2004; 1013:249–255. PMID: 15193535.
Article14. Kim KH, Abdi S. Rediscovery of nefopam for the treatment of neuropathic pain. Korean J Pain. 2014; 27:103–111. PMID: 24748937.
Article15. Sittl R, Irnich D, Lang PM. Update on preemptive analgesia: options and limits of preoperative pain therapy. Anaesthesist. 2013; 62:789–796. PMID: 24052051.16. Choi I, Ahn JO, So WS, Lee SJ, Choi IJ, Kim H. Exiting root injury in transforaminal endoscopic discectomy: preoperative image considerations for safety. Eur Spine J. 2013; 22:2481–2487. PMID: 23754603.
Article17. Durrieu G, Olivier P, Bagheri H, Montastruc JL;. Overview of adverse reactions to nefopam: an analysis of the French Pharmacovigilance database. Fundam Clin Pharmacol. 2007; 21:555–558. PMID: 17868209.
Article