J Korean Neurosurg Soc.
2015 Dec;58(6):547-549. 10.3340/jkns.2015.58.6.547.
Acute Spontaneous Subdural Hematoma due to Rupture of a Tiny Cortical Arteriovenous Malformation
- Affiliations
-
- 1Department of Neurosurgery and Medical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea. medfirst@pusan.ac.kr
- KMID: 2151157
- DOI: http://doi.org/10.3340/jkns.2015.58.6.547
Abstract
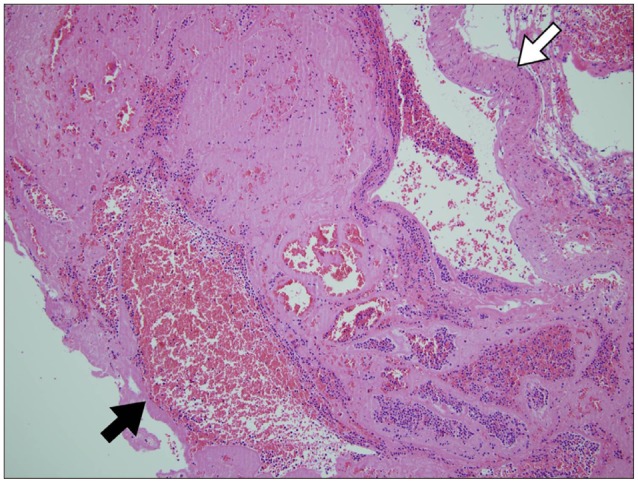
- Acute subdural hematoma (SDH) of arterial origin is rare, especially SDH associated with an arteriovenous malformation (AVM) is extremely rare. The authors report a case of acute spontaneous SDH due to rupture of a tiny cortical AVM. A 51-year-old male presented with sudden onset headache and mentality deterioration without a history of trauma. Brain CT revealed a large volume acute SDH compressing the right cerebral hemisphere with subfalcine and tentorial herniation. Emergency decompressive craniectomy was performed to remove the hematoma and during surgery a small (5 mm sized) conglomerated aciniform mass with two surrounding enlarged vessels was identified on the parietal cortex. After warm saline irrigation of the mass, active bleeding developed from a one of the vessel. The bleeding was stopped by coagulation and the vessels were removed. Histopathological examination confirmed the lesion as an AVM. We concluded that a small cortical AVM existed at this area, and that the cortical AVM had caused the acute SDH. Follow up conventional angiography confirmed the absence of remnant AVM or any other vascular abnormality. This report demonstrates rupture of a cortical AVM is worth considering when a patient presents with non-traumatic SDH without intracerebral hemorrhage or subarachnoid hemorrhage.
MeSH Terms
Figure
Reference
-
1. Byun HS, Patel PP. Spontaneous subdural hematoma of arterial origin : report of two cases. Neurosurgery. 1979; 5:611–613. PMID: 534070.2. Datta NN, Chan KY, Kwok JC, Poon CY. Posterior fossa subdural hematoma due to ruptured arteriovenous malformation. Case report. Neurosurg Focus. 2000; 8:ecp1. PMID: 16859278.3. Drake CG. Subdural haematoma from arterial rupture. J Neurosurg. 1961; 18:597–601. PMID: 13724255.
Article4. Ernestus RI, Beldzinski P, Lanfermann H, Klug N. Chronic subdural hematoma : surgical treatment and outcome in 104 patients. Surg Neurol. 1997; 48:220–225. PMID: 9290707.
Article5. Guazzo EP, Xuereb JH. Spontaneous thrombosis of an arteriovenous malformation. J Neurol Neurosurg Psychiatry. 1994; 57:1410–1412. PMID: 7964822.
Article6. Kondziolka D, Bernstein M, ter Brugge K, Schutz H. Acute subdural hematoma from ruptured posterior communicating artery aneurysm. Neurosurgery. 1988; 22(1 Pt 1):151–154. PMID: 3344078.
Article7. Matsumura H, Makita Y, Someda K, Kondo A. Arteriovenous malformations in the posterior fossa. J Neurosurg. 1977; 47:50–56. PMID: 301180.
Article8. McCormick WF, Hardman JM, Boulter TR. Vascular malformations ("angiomas") of the brain, with special reference to those occurring in the posterior fossa. J Neurosurg. 1968; 28:241–251. PMID: 5643915.
Article9. McDermott M, Fleming JF, Vanderlinden RG, Tucker WS. Spontaneous arterial subdural hematoma. Neurosurgery. 1984; 14:13–18. PMID: 6694787.
Article10. Sambasivan M. An overview of chronic subdural hematoma : experience with 2300 cases. Surg Neurol. 1997; 47:418–422. PMID: 9131021.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Subdural Hematoma of Arterial Origin
- A Neonatal Arteriovenous Malformation with Subdural and Intracerebral Hematoma
- Intracranial Dural Arteriovenous Malfirmation: Report of Three Cases
- Intraoperative Development of Contralateral Subdural Hematoma during Evacuation of Acute Subdural Hematoma: Case Report
- Spontaneously Rapid Resolution of Acute Subdural Hemorrhage with Severe Midline Shift