J Pathol Transl Med.
2015 Jul;49(4):325-330. 10.4132/jptm.2015.05.20.
WHO Grade IV Gliofibroma: A Grading Label Denoting Malignancy for an Otherwise Commonly Misinterpreted Neoplasm
- Affiliations
-
- 1Pathology Unit, Neuropathology Service, Mexico General Hospital, Mexico City, Mexico. k7nigricans@hotmail.com
- KMID: 2151142
- DOI: http://doi.org/10.4132/jptm.2015.05.20
Abstract
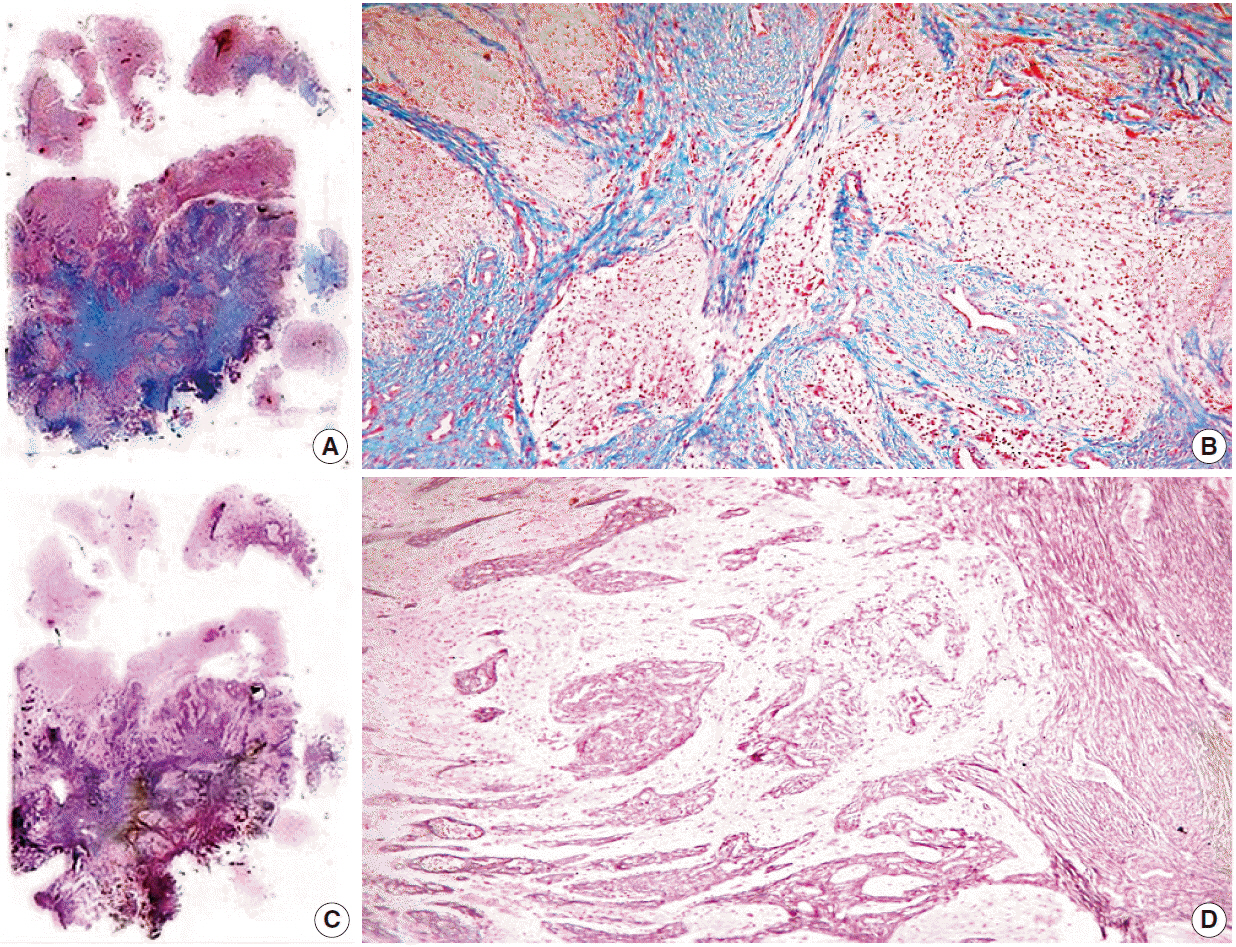
- We report a 50-year-old woman with no relevant clinical history who presented with headache and loss of memory. Magnetic resonance imaging showed a left parieto-temporal mass with annular enhancement after contrast media administration, rendering a radiological diagnosis of high-grade astrocytic neoplasm. Tumour sampling was performed but the patient ultimately died as a result of disease. Microscopically, the lesion had areas of glioblastoma mixed with a benign mesenchymal constituent; the former showed hypercellularity, endothelial proliferation, high mitotic activity and necrosis, while the latter showed fascicles of long spindle cells surrounded by collagen and reticulin fibers. With approximately 40 previously reported cases, gliofibroma is a rare neoplasm defined as either glio-desmoplastic or glial/benign mesenchymal. As shown in our case, its prognosis is apparently determined by the degree of anaplasia of the glial component.
Keyword
MeSH Terms
Figure
Reference
-
1. Friede RL. Gliofibroma: a peculiar neoplasia of collagen forming glia-like cells. J Neuropathol Exp Neurol. 1978; 37:300–13.2. Gargano P, Zuccaro G, Lubieniecki F. Intracranial gliofibroma: a case report and review of the literature. Case Rep Pathol. 2014; 2014:165025.
Article3. Prayson RA. Disseminated spinal cord astrocytoma with features of gliofibroma: a review of the literature. Clin Neuropathol. 2013; 32:298–302.
Article4. Sharma MC, Gaikwad S, Mehta VS, Dhar J, Sarkar C. Gliofibroma: mixed glial and mesenchymal tumour: report of three cases. Clin Neurol Neurosurg. 1998; 100:153–9.
Article5. Vazquez M, Miller DC, Epstein F, Allen JC, Budzilovich GN. Glioneurofibroma: renaming the pediatric “gliofibroma”: a neoplasm composed of Schwann cells and astrocytes. Mod Pathol. 1991; 4:519–23.6. Deb P, Sarkar C, Garg A, Singh VP, Kale SS, Sharma MC. Intracranial gliofibroma mimicking a meningioma: a case report and review of literature. Clin Neurol Neurosurg. 2006; 108:178–86.
Article7. Suarez CR, Raj AB, Bertolone SJ, Coventry S. Carboplatinum and vincristine chemotherapy for central nervous system gliofibroma: case report and review of the literature. J Pediatr Hematol Oncol. 2004; 26:756–60.8. Snipes GJ, Steinberg GK, Lane B, Horoupian DS. Gliofibroma: case report. J Neurosurg. 1991; 75:642–6.9. Schober R, Bayindir C, Canbolat A, Urich H, Wechsler W. Gliofibroma: immunohistochemical analysis. Acta Neuropathol. 1992; 83:207–10.
Article10. Cerda-Nicolas M, Kepes JJ. Gliofibromas (including malignant forms), and gliosarcomas: a comparative study and review of the literature. Acta Neuropathol. 1993; 85:349–61.
Article11. Caldemeyer KS, Zimmerman RA, Azzarelli B, Smith RR, Moran CC. Gliofibroma: CT and MRI. Neuroradiology. 1995; 37:481–5.
Article12. Kim Y, Suh YL, Sung C, Hong SC. Gliofibroma: a case report and review of the literature. J Korean Med Sci. 2003; 18:625–9.
Article13. Bastos Leite AJ, Palmeira de Sousa C, Honavar M. Malignant gliofibroma (desmoplastic glioblastoma) in an adult: case report. J Neuroradiol. 2002; 29:215–8.14. Altamirano E, Jones MC, Drut R. Gliofibroma. Comunicación de un caso pediátrico y revisión de la bibliografía. Patol Rev Latinoam. 2011; 49:221–5.15. Biernat W, Aguzzi A, Sure U, Grant JW, Kleihues P, Hegi ME. Identical mutations of the p53 tumor suppressor gene in the gliomatous and the sarcomatous components of gliosarcomas suggest a common origin from glial cells. J Neuropathol Exp Neurol. 1995; 54:651–6.
Article16. Prayson RA. Gliofibroma: a distinct entity or a subtype of desmoplastic astrocytoma? Hum Pathol. 1996; 27:610–3.
Article17. Kim NR, Suh YL, Shin HJ, Park IS. Gliofibroma with extensive calcified deposits. Clin Neuropathol. 2003; 22:14–22.18. Matsumura A, Takano S, Nagata M, Anno I, Nose T. Cervical intramedullary gliofibroma in a child: a case report and review of the literature. Pediatr Neurosurg. 2002; 36:105–10.19. Goyal S, Puri T, Gunabushanam G, et al. Gliofibroma: a report of three cases and review of literature. Acta Oncol. 2007; 46:1202–4.
Article20. Erguvan-Onal R, Ates¸ O, Onal C, Aydin NE, Koçak A. Gliofibroma: an incompletely characterized tumor. Tumori. 2004; 90:157–60.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: WHO Grade IV Gliofibroma: A Grading Label Denoting Malignancy for an Otherwise Commonly Misinterpreted Neoplasm
- Adult Intracranial Gliofibroma : A Case Report and Review of the Literature
- Correlation of CT Findings and Pathologic Nuclear Grading in Renal Cell Carcinoma
- Gliofibroma: A Case Report and Review of the Literature
- Comparison of Rb and p53 Protein Expression with Stage and Grade as a Prognostic Value in Renal Cell Carcinoma